Isolated Hypoplasia of Left Pulmonary Artery with Agenesis of Left Lobe of Thyroid: A Case Report
Mohammed Abdul Khadir1, Ganesh Narayana2, Ganavi Ramagopal3, Pradeep G Nayar4
1 Registrar, Department of Cardiology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
2 Associate Professor, Department of Cardiology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
3 Assistant Professor, Department of Paediatrics, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
4 Professor and Head, Department of Cardiology, Chettinad Hospital and Research Institute, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ganavi Ramagopal, Assistant Professor, Department of Pediatrics Chettinad Hospital and Research Institute Kelambakkkam, Chennai-603103, Tamil Nadu, India.
E-mail: ggganavi10@gmail.com
Isolated Unilateral hypoplasia or agenesis of a branch of pulmonary artery is very rare. It is usually seen associated with congenital heart diseases such as tetralogy of Fallot, atrial septal defect, coarctation of the aorta, right aortic arch, truncus arteriosus, patent ductus arteriosus and pulmonary atresia. It occurs as a result of lack of embryological development of either the left or right sixth aortic arch and has been found to present itself with various clinical manifestations as during childhood it presents as contralateral pulmonary hypertension and in adults as haemoptysis. Early diagnosis and early surgical indication avoids the evolution of pulmonary hypertension to unfavourble state of more severe and progressive degrees and also prevents the development of pulmonary systemic collateral circulation, which is mainly responsible for subsequent haemoptysis in the adulthood. We hereby, report the case of an infant who presented with features of lower respiratory tract infection and later diagnosed as isolated congenital hypoplasia of left pulmonary artery and hence planned for proper follow-up for early surgery thereby preventing complications in the future.
Hypoplasic lung, Hypoxia, Pulmonary hypertension, Respiratory distress
Case Report
A six-month-old female infant, first born out of nonconsangunious marriage was brought with fever of 3 days and history of fast breathing and refusal to feed for one day with history of cough, cold on and off since one month for which treatment was taken on outpatient basis with a local practitioner and no investigations done.
Antenatal and perinatal history were uneventful with baby being term with birth weight of 2.6 kg and no Neonatal Intensive Care Unit (NICU) admissions, developmental milestones were normal and immunized till date. The mother was operated for atrial septal defect during her childhood.
On examination, the baby was irritable, tachypnoeic with nasal flaring, intercostal and subcostal retractions and grunting. The SpO2 was 90% in room air at the time of admission. Systemic examination revealed crepitations bilateral lung fields and air entry was reduced on left side with tachycardia and no murmurs or gallops.
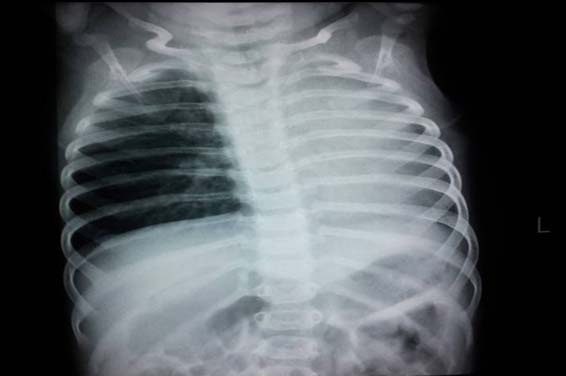
Her initial blood tests showed haemoglobin of 10g/dl and leucocytosis with neutrophilic predominance and arterial blood gases showed hypoxia for which oxygen was delivered Non Re-Breather Mask (NRBM) and SpO2 of 99% was maintained. Chest x-ray taken [Table/Fig-1] which revealed hypoplasia of the left lung, elevated left hemi diaphragm, shift of mediastinum to the left and prominent right pulmonary artery shadow.
Chest x-ray PA view showing hypoplasia of the left lung, elevated left hemi diaphragm, shift of mediastinum to the left, and prominent right pulmonary artery shadow.
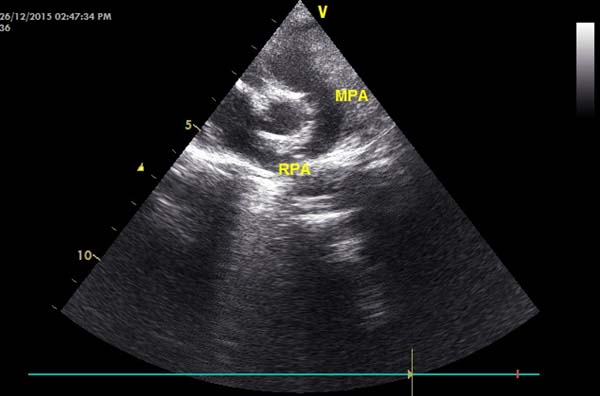
Echocardiogram revealed situs solitus, levocardia, atrioventricular and ventriculoarterial concordance. Normal right and left ventricular function. Normally related great arteries. Normal systemic and pulmonary venous connection and cardiac chambers. Trivial tricuspid regurgitation (Pressure gradient 14mmHg) with normal pulmonary artery pressures. The left pulmonary artery was absent and main pulmonary artery continued as the right pulmonary artery. There were no atrial or ventricular septal defects and no coarctation of aorta [Table/Fig-2].
Echocardiography showing the absent left pulmonary artery and main pulmonary artery continuing as the right pulmonary artery.
Further chest computed tomography [Table/Fig-3a,b] showed a hypoplastic left lung along with left pulmonary artery hypoplasia. There was reduced vascularity of the left lung. The right pulmonary artery was dilated. Computed Tomography (CT) Thorax had incidentally picked up agenesis of left lobe of thyroid [Table/Fig-4]. FreeT4 (0.92ng/dl) and T3 levels (3.4pg/ml) were normal but Thyroid Stimulating Hormone (TSH) level was 7.67uIU/ml slightly above the range (0.8-7.09) so, she was not started on any medications but was counseled for radionucleotide scan which the patient refused. The patient was treated symptomatically and her pneumonia resolved. She improved gradually and was discharged after 2 weeks and asked to come for regular follow-up to monitor pulmonary artery pressure and thyroid status once in 3 months.
CT Chest showing a hypoplastic left lung along with left pulmonary artery hypoplasia.
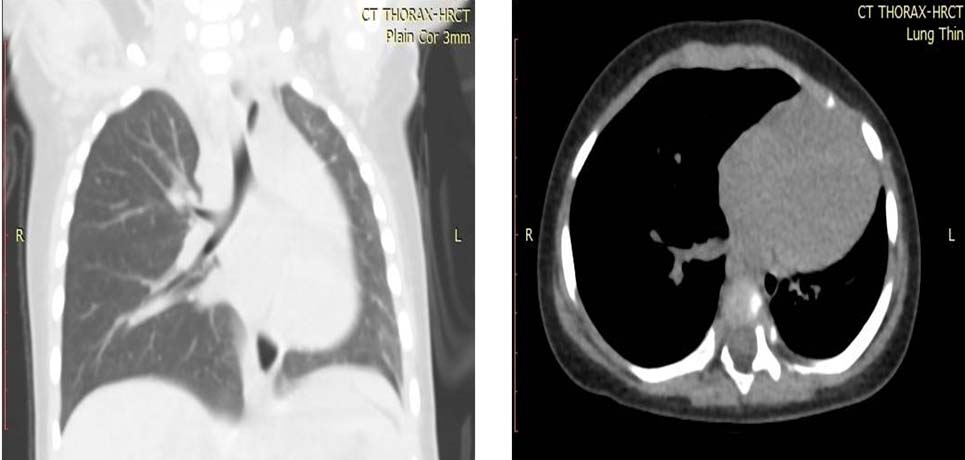
CT Chest showing agenesis of left lobe of thyroid.

Discussion
Congenital agenesis of Pulmonary Artery (PA) or hypoplasia is a rare anomaly with prevalence in the general population of 1/200,000 and is caused by a malformation of the sixth aortic arch of the affected side during embryogenesis [1]. Isolated occurrence of hypoplasia of pulmonary artery is usually rare as seen in our case and they can be accompanied by other congenital heart abnormalities such as tetralogy of fallot, atrial septal defect, coarctation of the aorta, right aortic arch, truncus arteriosus, patent ductus arteriosus, and pulmonary atresia [2]. It involves right lung in about 2/3rd of the cases in which hypoplasia of pulmonary artery is on the side of chest opposite to the aortic arch unlike in our case where left pulmonary artery is involved [3,4].
There are cases reported with the median age of 14 years with no sex predilection [3], our case was six-month-old infant similar to case reported by Purani C et al., [5].
The patients may be asymptomatic, which may delay the diagnosis or present with varied symptoms like recurrent respiratory infections as in our case, chronic dyspnea, exercise intolerance and sometimes with haemoptysis. The prognosis depends on the associated cardiovascular anomalies and the degree of Pulmonary Artery Hypoplasia (PAH) [3].
Patient’s especially young children as in our case usually present with recurrent lower respiratory tract infection which occurs due to various mechanisms like, lack of arterial blood flow to the affected lung may result in poor flow of inflammatory cells to the sites of inflammation and also impaired ciliary function. In addition, it may result in alveolar hypocapnea, leading to secondary bronchoconstriction and mucous trapping [6]. Haemoptysis is one of the serious complication which usually is presenting complaint in some adults and appears to be caused by large collateral circulation that subject venous systems to unusually high pressures.
As sequelae PAH occur due to various mechanisms, the persistent fetal structure of the unaffected pulmonary artery (opposite to the absent pulmonary artery) was the predominant mechanism postulated for pulmonary hypertension. Second mechanism cited was a reduction in the elastic property of the vasculature of the normal lung which is exposed to the total cardiac output from the right ventricle. In another mechanism, it was postulated that the blood flow directed away from absent pulmonary artery to remaining pulmonary artery and the increased blood flow leading to sheer stress on the endothelium, which results in the release of vasoconstrictors such as endothelin. Chronic vasoconstriction of the pulmonary arterioles further lead to remodeling resulting in increased resistance in the pulmonary vasculature and PAH [7,8].
Diagnosing unilateral isolated absence or hypoplasia of a pulmonary artery is very difficult unless one looks for important clues present in chest radiographs with high index of suspicion. Chest x-rays frequently show a decreased size of the affected hemithorax, compensatory hyperinflation of the contralateral hemithorax, elevation of the ipsilateral hemidiaphragm, absent ipsilateral and enlarged contralateral pulmonary artery shadow, a right-sided aortic arch and an ipsilateral shift of the mediastinum. Most of these findings were present in the chest X-ray of our case. Definite diagnosis can be made by computed tomography, magnetic resonance imaging or transthoracic echocardiogram. Pulmonary angiography is considered the gold standard for diagnosis [1,9,10].
Treatment is usually based on the symptoms and pulmonary haemodynamic status. Asymptomatic patients should be followed regularly to detect early development of PAH. Patients who develop PAH can be treated medically with vasodilator therapy, but as there was no PAH in our case it was not used [3,7]. Alternatively, revascularization of peripheral branches of the affected pulmonary artery to the pulmonary hilum can also be done in cases of PAH [2,11,12]. If patients present with haemoptysis, it may be treated with embolization, lobectomy or pneumonectomy [13,14].
Conclusion
Isolated hypoplasia of the left pulmonary artery is a rare entity, unless one looks into chest radiographs with a high index of suspicion in certain cases as the diagnosis is very difficult. However, it should be included in the differential diagnosis of a chest radiograph with a contracted hyperlucent hemithorax. Once diagnosed, early surgery avoids the unfavourable progression of pulmonary hypertension to more severe degrees and there by prevents the development of pulmonary systemic collateral circulation, responsible for subsequent haemoptysis.
[1]. Bouros D, Pare P, Panagou P, Tsintiris K, Siafakas N, The varied manifestation of pulmonary artery agenesis in adulthoodChest 1995 108(3):670-76. [Google Scholar]
[2]. Presbitero P, Bull C, Haworth SG, de Leval MR, Absent or occult pulmonary arteryBr Heart J 1984 52(2):178-85. [Google Scholar]
[3]. Ten Harkel AD, Blom NA, Ottenkamp J, Isolated unilateral absence of a pulmonary artery: A case report and review of the literatureChest 2002 122(4):1471-77. [Google Scholar]
[4]. Pfefferkorn JR, Löser H, Pech G, Toussaint R, Hilgenberg F, Absent pulmonary artery. A hint to its embryogenesisPediatr Cardiol 1982 3(4):283-86. [Google Scholar]
[5]. Purani C, Mehariya KM, Gupta K, Patel P, Hypoplasia of left pulmonary artery: A rare congenital heart diseaseIndian J Child Health 2015 2(1):31-33. [Google Scholar]
[6]. Kadir IS, Thekudan J, Dheodar A, Jones MT, Carroll KB, Congenital unilateral pulmonary artery agenesis and aspergillomaAnn Thorac Surg 2002 74(6):2169-71. [Google Scholar]
[7]. Shostak E, Sarwar A, A 50-year-old woman with dyspnea, lower extremity edema, and volume loss of the right hemithoraxChest 2009 136(2):628-32. [Google Scholar]
[8]. Rubin E, Strauss L, Congenital absence of the right pulmonary artery. Report of a case in a five month old infant, with suggestive evidence of unilateral pulmonary hypertensionAm J Cardiol 1960 6:344-50. [Google Scholar]
[9]. Harris KM, Lloyd DCF, Morrissey B, Adams H, The computed tomographic appearances in pulmonary artery atresiaClin Radiol 1992 45:382-86. [Google Scholar]
[10]. Griffin N, Mansfield L, Redmond KC, Dusmet M, Goldstraw P, Mittal TK, Imaging features of isolated unilateral pulmonary artery agenesis presenting in adulthood: A review of four casesClin Radiol 2007 62:238-44. [Google Scholar]
[11]. Welch K, Hanley F, Johnston T, Cailes C, Shah MJ, Isolated unilateral absence of right proximal pulmonary artery: surgical repair and follow-upAnn Thorac Surg 2005 79(4):1399-402. [Google Scholar]
[12]. Toews WH, Pappas G, Surgical management of absent right pulmonary artery with associated pulmonary hypertensionChest 1983 84(4):497-99. [Google Scholar]
[13]. Reñé M, Sans J, Dominguez J, Sancho C, Valldeperas J, Unilateral pulmonary artery agenesis presenting with haemoptysis: treatment by embolization of systemic collateralsCardiovasc Intervent Radiol 1995 18(4):251-54. [Google Scholar]
[14]. Bekoe S, Pellegrini RV, DiMarco RF Jr, Grant KJ, Woelfel GF, Pneumonectomy for unremitting haemoptysis in unilateral absence of pulmonary arteryAnn Thorac Surg 1993 55(6):1553-54. [Google Scholar]