Mature Teratoma at Left Lumbar Region in an Infant: A Case Report
Rajendra Kumar Ghritlaharey1
1 Professor and Head, Department of Pediatric Surgery, Gandhi Medical College and Associated Kamla Nehru and Hamidia Hospitals, Bhopal, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajendra Kumar Ghritlaharey, Department of Pediatric Surgery, Gandhi Medical College and Associated, Kamla Nehru and Hamidia Hospitals, Bhopal-462001, Madhya Pradesh, India.
E-mail: drrajendrak1@rediffmail.com
Common location of teratomas in children are sacrococcygeal, gonadal, mediastinal and retroperitoneal, but teratomas may also occur at very unusual locations. A six-month-old boy presented with a large swelling at his left lumbar region. He presented with gradually increasing lump at his back, involving more on left lumbar region and midline since birth. Clinical examination revealed a solitary, non-tender, soft to firm, irregular mass, occupying more on his left lumbar and midline region and also crossing the midline. Radiological investigations revealed a well defined mass of 9.6 x 7.5cm, with bony elements and spina bifida at L1 and L2 levels. His Computed Tomography (CT) scan finding was consistent with mature teratoma. Complete surgical excision of the tumour was done without any difficulties. Histology of the excised tumour was conclusive of mature teratoma. His post-operative period was excellent, but he lost to follow-up after discharge.
Children, Infant, Surgical therapy, Teratoma, Tumour
Case Report
A six-month-old boy was brought to the Department of Paediatric Surgery with a large swelling at his left lumbar region. He presented with a gradually increasing lump at his back, involving more on his left lumbar region and midline since, birth. There were no other complaints. Local examination revealed a solitary swelling of size 9.6 x 7.5cm in its maximum length. It was occupying more on his left lumbar region, midline and also crossing the midline region [Table/Fig-1]. Skin over the swelling was normal, soft to firm, non-tender and trans-illumination test of the swelling was negative. During clinical examination other associated obvious anomalies were not detected. Both of his gonads were descended normally in scrotum and were normal. Abdominal examination was within normal limits and there were no organomegaly or ascites. Other systemic examination was also within normal limits.
Clinical photograph showing a large swelling at left lumbar area

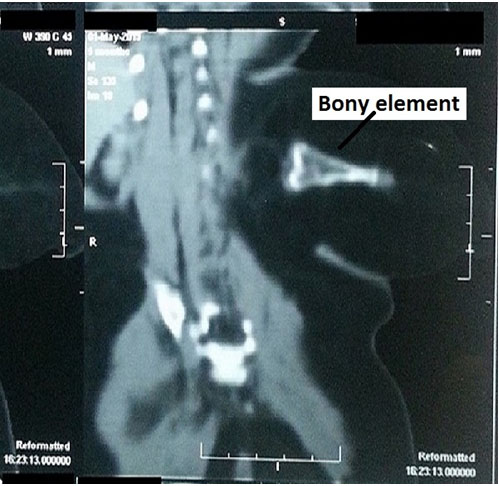
Ultrasonography, plain and Contrast Enhanced Computed Tomography (CECT) scans of the swelling revealed a well defined mass of 9.6 x 7.5cm. Spina bifida was also observed at L1 and L2 levels that also contained an ill defined soft tissue mass. There were no intra-spinal lesions seen on CT scans. CT scans also showed a hyper-dense bony structure of 1.6 x 4cm [Table/Fig-2]. His liver, kidneys and other intra-abdominal organs were normal. His CT scan finding was suggestive of mature teratoma. Serum Alpha Fetoprotein (AFP) was done prior to surgical excision of the tumour and was reported as 41.6IU/ml.
CT scan of the swelling showing bony elements and soft tissues shadow.
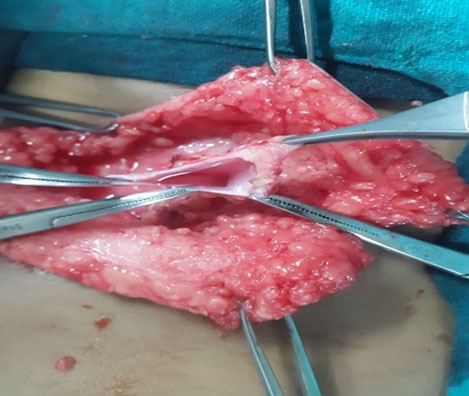
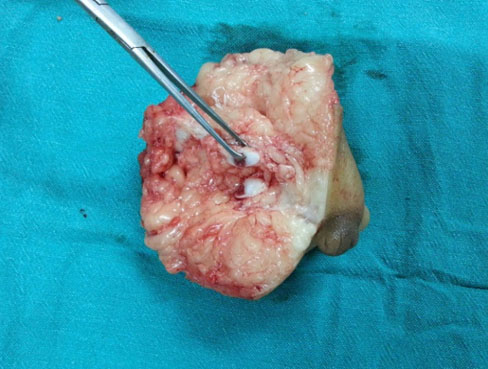
Complete surgical excision of the tumour was achieved without any difficulties [Table/Fig-3a]. An elliptical incision was given over the tumour in its transverse direction, which also crossed the midline. The tumour mostly contained fatty tissues and it was easily dissected out all around. Small bony tissues were also present within the tumour mass, which were also easily dissected out. Spina bifida was also noted at L1 – L2 levels. Part of dura was protruded outwards from spinal defect as mentioned above. Although intra-dural extension/ lesion were not reported in CT scans, but dural sac was opened up to see any attached nerve fibers [Table/Fig-3b]. Redundant dura was trimmed and it was repaired as there were no attached nerve fibers. Excised tumour was composed more of fatty tissues and few bony elements [Table/Fig-3c]. Excised tumour was submitted for histopathological examination that also confirmed the diagnosis of mature teratoma. His post-operative period was uneventful and excellent and he was discharged on fifth post-operative day. He lost to follow-up after discharge and therefore his late post-operative course could not be ascertained.
Photograph showing completely excised tumour;

Operative photograph showing opened up dura without any contents;
Photograph of excised tumour showing fatty tissues and bone elements.
Discussion
Teratoma is derived from Greek words teratos/teras, meaning "monster," and onkoma/oma, denoting a swelling, tumour or neoplasm. A teratoma is a true tumour or neoplasm having multiple tissues of kinds foreign to the parts in which it arises. Teratomas are the tumour which consists of the tissues that arise from embryonic ectoderm, mesoderm and endoderm. Common locations of teratomas in children are sacroccocygeal, gonadal, mediastinal, and retroperitoneal [1-5]. Teratomas may also occur at very unusual locations and are intra-peritoneal teratomas arising from mesentery and mesocolon, gastric teratoma, spinal teratoma, teratoma occurring at cervical region, intra-cranial teratomas occurring at medulla oblongata, teratoma occurring at liver and kidney [6-10].
In the present case, teratoma was located at left lumbar region, midline and also crossed the midline. This is a very rare location for the occurrence of teratoma. Faheem M et al., reported a similar case in a 16-year-old boy. In this case the teratoma was also located at lumbosacral region. The tumour was diagnosed as benign cystic teratoma and complete surgical excision of the tumour was achieved. Diagnosis of mature teratoma was also confirmed on histopathological examination of excised tumour [11]. They further stated that, in a study conducted over a period of 22-years at Jaipur, India revealed only one similar case of teratoma arising from lumbosacral region (in a female) among 75 cases of teratoma [11]. Intra-medullary teratomas occurring in the spinal cord are very rare, especially in adults over 50 years of age. Nonomura Y et al., reported two cases of intra-medullary teratoma that occurred in the spinal cord in adults at the age of 37 years in a female and 56 years in a male [12]. Parelkar SV et al., reported a very rare case of mature teratoma associated with ruptured meningomyelocele of lumbosacral region and they stated that, only few cases have been published in this concurrence [13].
In general complete surgical excision remains the mainstay and a therapy of choice for teratomas irrespective of its locations. Complete surgical excision alone is adequate therapy for non-malignant mature teratomas [1]. In some of the cases it is not possible to completely excise the teratoma due to its difficult locations, adhesions, and its close proximity with great vessels [5]. Post-operative adjuvant therapy is needed in the cases of malignant teratomas [2-4]. In present case it was possible to suspect during the investigation that, this was a case of teratoma due to the presence of bony elements, and it was also possible to excise the tumour completely.
Recurrence following the surgical resection of the teratoma has been reported and it mostly depends upon the histological features of the tumours. It is more commonly evident in the cases with immature and malignant teratomas, although rarely also observed following excision of mature teratomas. For the above reason a close and long-term follow-up is advisable and if recurrence is noted prompt therapy must be instituted accordingly [1,5]. Measurement of serum AFP during follow-up period is a reliable method for detecting the recurrence in the cases of teratomas and it is a must for the cases of immature and malignant teratomas. Raised serum AFP levels in patients with immature teratomas have higher risk of malignancy than with normal serum AFP levels [2,6,10].
Conclusion
Teratoma may also occur at very unusual location. Complete surgical excision remains a best option to manage teratoma, and it is always preferable to completely excise the teratoma at the earliest during the neonatal period.
[1]. Rescorla FJ, Sawin RS, Coran AG, Dillon PW, Azizkhan RG, Long-term outcome for infants and children with sacrococcygeal teratoma: a report from the childrens cancer groupJ Pediatr Surg 1998 33:171-76. [Google Scholar]
[2]. Wei Y, Wu SD, Lin T, He DW, Li XL, Liu JH, Testicular teratoma in children: Analysis of 64 casesZhonghua Nan Ke Xue 2015 21:809-15. [Google Scholar]
[3]. Zhang M, Jiang W, Li G, Xu C, Ovarian masses in children and adolescents - an analysis of 521 clinical casesJ Pediatr Adolesc Gynecol 2014 27:e73-77. [Google Scholar]
[4]. Yalçın B, Demir HA, Tanyel FC, Akçören Z, Varan A, Akyüz C, Mediastinal germ cell tumors in childhoodPediatr Hematol Oncol 2012 29:633-42. [Google Scholar]
[5]. Jones VS, Burns CR, Operative considerations in pediatric retroperitoneal teratomas --a reviewEur J Pediatr Surg 2013 23:265-69. [Google Scholar]
[6]. Srivastava J, Ghritlaharey RK, Immature mesenteric teratoma in an infant: A case reportJ Clin Diagn Res 2010 4:3581-84. [Google Scholar]
[7]. Sharma MC, Aggarwal M, Ralte AM, Vaishya V, Suri A, Gupta V, Clinicopathological study of spinal teratomas. A series of 10 caseJ Neurosurg Sci 2003 47:95-100. [Google Scholar]
[8]. Shetty KJ, Kishan Prasad HL, Rai S, Kumar YS, Bhat S, Sajjan N, Unusual presentation of immature teratoma of the neck: A rare case reportJ Cancer Res Ther 2015 11:647 [Google Scholar]
[9]. Li D, Hao SY, Wu Z, Zhang LW, Zhang JT, Primary medulla oblongata teratomasJ Neurosurg Pediatr 2014 14:296-300. [Google Scholar]
[10]. Paradies G, Zullino F, Orofino A, Leggio S, Rare extragonadal teratomas in children: complete tumor excision as a reliable and essential procedure for significant survival. Clinical experience and review of the literatureAnn Ital Chir 2014 85:56-68. [Google Scholar]
[11]. Faheem M, Syed HH, Kardam D, Maheshwari V, Khan R, Sharma A, Teratoma of the lumbosacral region: a case reportJ Med Case Rep 2011 5:370 [Google Scholar]
[12]. Nonomura Y, Miyamoto K, Wada E, Hosoe H, Nishimoto H, Ogura H, Intra-medullary teratoma of the spine: report of two adult casesSpinal Cord 2002 40:40-43. [Google Scholar]
[13]. Parelkar SV, Oak SN, Mundada D, Sanghvi BV, Joshi PB, Kapadnis SP, Midline mature teratoma inside a ruptured meningomyelocele of lumbosacral region, a case reportJ Pediatr Surg 2012 47:1934-37. [Google Scholar]