Enteric Duplication Cyst Leading to Volvulus: An Unusual Cause of Acute Intestinal Obstruction – A Case Report
Raju Rangaswamy1, Kuotho T Nyuwi2, Chabungbam Gyan Singh3, Ty Apila Sangtam4, Lalhruaitluanga Varte5
1 Junior Resident, Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India.
2 Junior Resident, Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India.
3 Assistant Professor, Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India.
4 Junior Resident, Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India.
5 Junior Resident, Department of Surgery, Regional Institute of Medical Sciences, Imphal, Manipur, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raju Rangaswamy, #6, PG Hostel-2, RIMS, Imphal-795440, Manipur, India.
E-mail: raju2rangaswamy@gmail.com
Enteric Duplication Cysts (EDC) is a rare congenital malformation, usually found in mesenteric side of Gastrointestinal (GI) tract. Generally patients present with non-specific symptoms depending on size and location of the cyst in GI tract. EDC presenting as small bowel volvulus is a rare clinical entity. Herein, we are reporting a 16-year-old adolescent girl who presented to Emergency Department (ED) with the features of acute bowel obstruction with septicemia. Patient underwent exploratory laparotomy which revealed dilated, twisted, gangrenous bowel due to a cystic lesion adjacent to the mesenteric side. Resection of the cystic lesion along with the affected gangrenous segment of bowel with an end to end anastomosis performed.
Bowel obstruction, Exploratory laparotomy, Gangrenous bowel
Case Report
A 16-year-old girl presented to the ED with diffuse intermittent abdominal pain, vomiting, and not able to pass stool for two days associated with progressive abdominal distention. On examination, she was dehydrated, with a blood pressure of 90/60 mmHg, pulse rate of 134 beat/min and temperature of 38.6°C. The abdomen was diffusely distended with generalized guarding and sluggish bowel sounds. Digital and proctoscopic examinations were normal with empty rectum. Immediate resuscitation in the ED was started with intravenous infusion of crystalloid fluids through large bore intravenous cannulae.
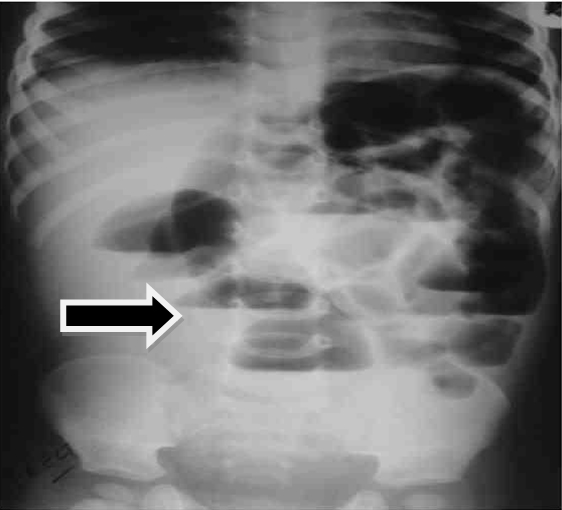
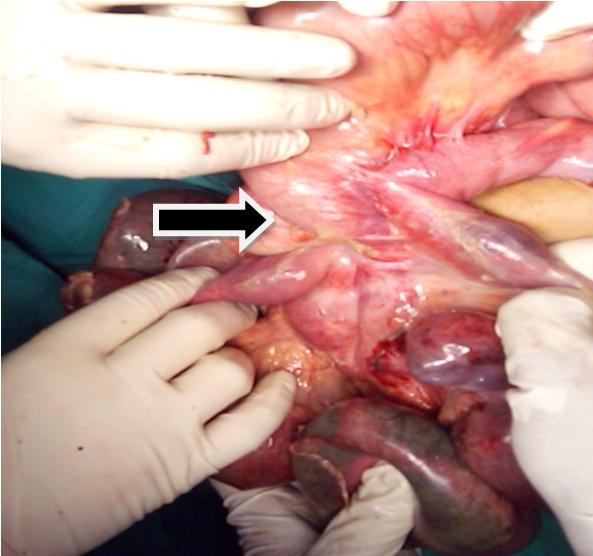
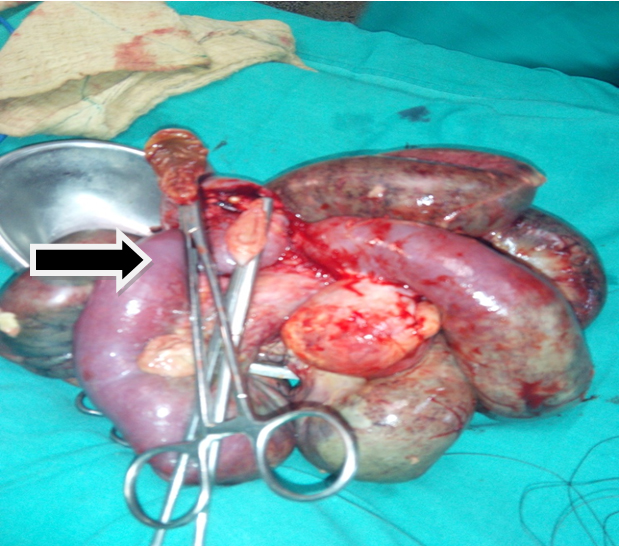
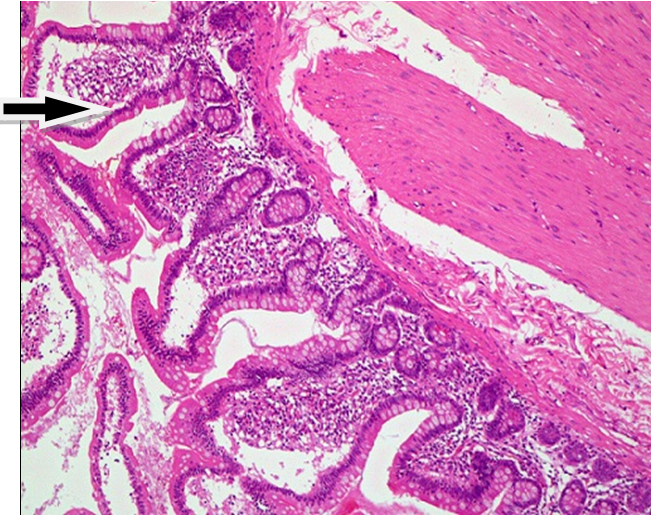
Laboratory values revealed a white blood cell count of 22.6 × 109/L, haemoglobin 9g/dL, urea 70mg/dl, creatinine 1.2mg/dl and normal coagulation profile. Plain abdominal X-ray revealed multiple air fluid level [Table/Fig-1]. After taking informed consent, she underwent exploratory laparotomy with a provisional diagnosis of acute small bowel obstruction. Abdominal exploration revealed dilated, twisted, gangrenous small bowel loops around 120cm about 15cm from ileo-caecal junction and cystic lesion measuring about 4cm in diameter was located adjacent to the mesenteric side [Table/Fig-2] was noted. Resection of the cystic lesion along with the affected gangrenous segment of intestine [Table/Fig-3], with an end to end anastomosis was performed. The histopathology showed a blind cystic structure with well preserved muscle wall lined by mucosal epithelium suggestive of intestinal duplication cyst ([Table/Fig-4], Hematoxylin and Eosin, 40X). The patient was discharged from the hospital on 8th day post-operatively with an uneventful post-operative course. The patient was followed-up after a month and she remained asymptomatic.
Plain abdominal X-ray erect posture showing multiple air-fluid level.
Duplication cyst with twisted gangrenous small bowel loop.
Resected specimen of gangrenous small bowel loop.
Histopathology examination showing intestinal duplication cyst lined by enteric mucosa (H&E, 40X).
Discussion
EDC is a rare congenital malformation, first coined by Fiorani C et al., [1]. It can occur anywhere in the GIT from the mouth to the anus with majority of the cases reported in ileum. Ladd AP et al., defined EDC as a tubular or spherical shaped anomaly that is attached or adherent to the normal alimentary tract and shared the similar phenotypic characteristics [2]. It is a separate entity from GIT with their own lumen, which occur either on the mesenteric or the anti-mesenteric side [1]. Several theories exist regarding the origin of these cysts, like abortive twinning theory, split notochord theory, intra-uterine vascular accident theory, but most accepted explanation is that duplication of the gut occurs due to pinching off of a diverticulum during embryological development [3]. The majority of cases have been reported in infants with estimated incidence of 1 in 4500 births [4].
Once EDC is functional, mucosa secrete fluids, expands and become symptomatic. As patients present with non-specific symptoms the diagnosis of EDC in the neonatal and infant periods can be quite difficult. Clinically patients with EDC present with passage of bright red blood per rectum due to ulceration of ectopic gastric mucosa and intestinal obstruction is either due to adjacent pressure on the bowel wall, intussusceptions or rarely due to volvulus [5]. However, rarely it has reported in adults as well, with complication like cyst torsion, cystic rupture, infection of the cyst, urinary obstruction or malignancy as epithelial instability is seen in long-standing duplication cysts [4,5]. EDCs may be suspected pre-natally by sonographic demonstration of an intra-abdominal cystic mass. Sonographic findings suggestive of an intestinal origin of the cyst are peristaltic muscular contractions of the cyst wall, double layered wall and close contact with the mesenteric border [4]. However, in adults multiple diagnostic tools are reported to be useful in the investigation of EDC including abdominal ultrasonography, gastrointestinal endoscopy and contrast-enhanced CT scan [6].
Surgical management of completely secluded cyst from intestine is resection without disturbing the bowel [7]. But resection of the duplication cyst along with the adjacent bowel is recommended due to the potential complication like malignant changes, ulceration and haemorrhage due to ectopic gastric mucosa [5]. However, resection of large duplication cyst is precluded owing to the risk of short-bowel syndrome. Mucosal stripping offers alternative surgical option in these cases, eliminating the possibility of subsequent peptic ulceration or carcinogenesis [8]. But in our case as twisted gangrenous small bowel loops was not possible to separate from the duplication cyst located in the mesenteric side of the bowel, the affected bowel was resected with the cystic lesion and end to end bowel anastomosis was performed.
Conclusion
Enteric duplication cysts are a rare congenital clinical entity of gastrointestinal system. Even though, it’s a congenital malformation, clinicians should be aware of this rare cause as differential diagnosis in patients presenting with feature of small bowel obstruction in adolescent population.
[1]. Fiorani C, Scaramuzzo R, Lazzaro A, Biancone L, Palmieri G, Gaspari AL, Intestinal duplication in adulthood: A rare entity, difficult to diagnoseWorld J Gastrointest Surg 2011 3:128-30. [Google Scholar]
[2]. Ladd AP, Grosfeld JL, Gastrointestinal tumors in children and adolescentsSemin Pediatr Surg 2006 15:37-47. [Google Scholar]
[3]. Tamvakopoulos GS, Sams V, Preston P, Stebbings WS, Iron-deficiency anaemia caused by an enterolith-filled jejunal duplication cystAnn R Coll Surg Engl 2004 86:W49-W51. [Google Scholar]
[4]. Basany L, Aepala R, Bellary MMR, Chitneni M, Intestinal obstruction due to ileal duplication cyst and malrotation in a preterm neonateJ Neonat Surg 2015 4(4):48 [Google Scholar]
[5]. Shah N, Lizardo-Escaño T, Shaaban H, Dhadham G, Karki A, Spira R, Enterogenous cyst of the small bowel causing intussusception in an adult: Case report and review of literatureJ Nat Sci Biol Med 2015 6:208-10. [Google Scholar]
[6]. Puligandla PS, Nguyen LT, St-Vil D, Flageole H, Bensoussan AL, Nguyen VH, Gastrointestinal duplicationsJ Pediatr Surg 2003 38:740-44. [Google Scholar]
[7]. Sinha A, Ojha S, Sarin YK, Completely isolated, non-contiguous duplication cystEur J Pediatr Surg 2006 16:127-29. [Google Scholar]
[8]. Azzie G, Beasley S, Diagnosis and treatment of foregut duplicationsSemin Pediatr Surg 2003 12:46-54. [Google Scholar]