An Unusual Occurrence of Methicillin Resistant Staphylococcal Endocarditis with Vancomycin Creep Phenomenon – A Therapeutic Challenge
S Sneha1, Shanthan Venishetty2, Shubha Seshadri3, M Sudhakar Rao4, Chiranjay Mukhopadhyay5
1 Assistant Professor, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
2 Junior Resident, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
3 Professor, Department of Internal Medicine, Kasturba Medical College, Manipal, Karnataka, India.
4 Registrar, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Professor, Department of Microbiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. M Sudhakar Rao, Department of Cardiology, Kasturba Medical College, Manipal University, Manipal - 576104, Karnataka, India.
E-mail: msudhakar88@gmail.com
Infective endocarditis by Methicillin Resistant Staphylococcus aureus (MRSA) bacteraemia is a common association and carries a high mortality. However, rising Minimum Inhibitory Concentrations (MICs) for vancomycin amongst MRSA strains is an emerging threat which carries poor prognosis and higher mortality. Here, we report a case of 41-year-old young non-addict gentleman presenting with fever of 3 days duration following recovery from an acute kidney injury necessitating haemodialysis. Systemic examination revealed signs of mitral regurgitation and left sided cerebellar signs. Laboratory investigations revealed anaemia, MRSA bacteraemia and transthoracic echocardiogram showed a mitral valve vegetation. He was diagnosed with MRSA mitral valve endocarditis with acute left cerebellar infarct. He was initially treated with intravenous vancomycin based on MIC at the dose of one gram every twelfth hourly. As the MRSA strain was shown to demonstrate a vancomycin creep phenomemon along with worsening clinical condition of the patient, treatment was changed to intravenous daptomycin at dose of 9mg/kg as per blood culture and sensitivity pattern which was administered for 6 weeks. Following initiation of daptomycin patient became afebrile and vegetations reduced in size and finally disappeared.
Daptomycin, Minimum inhibitory concentration, Mitral valve endocarditis
Case Report
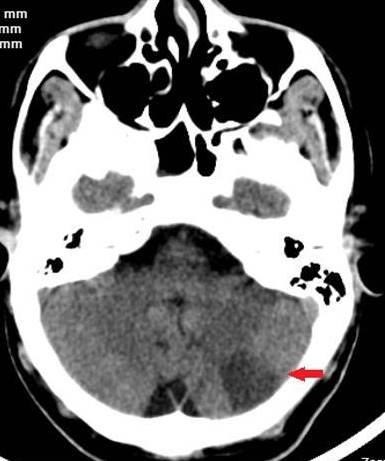
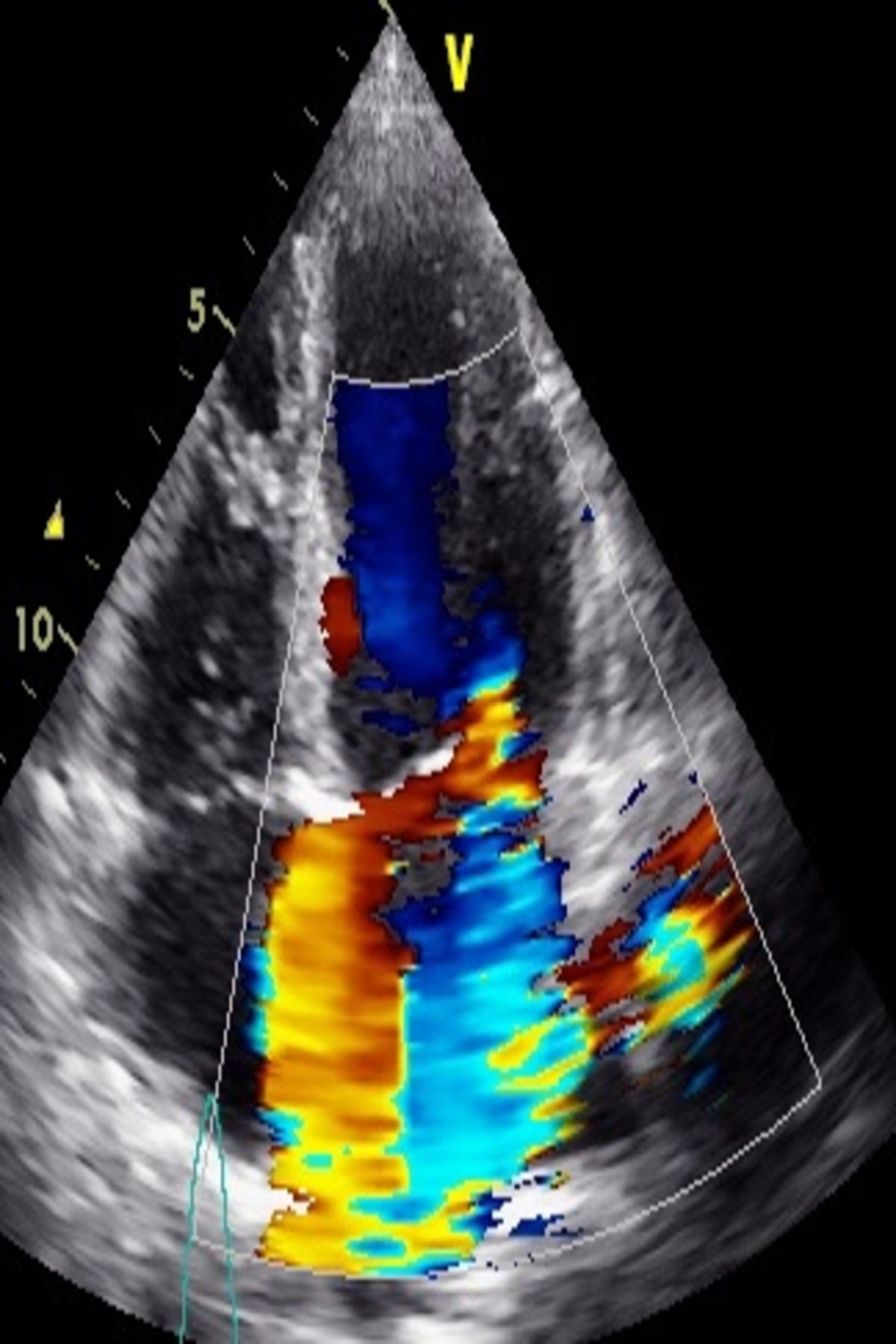
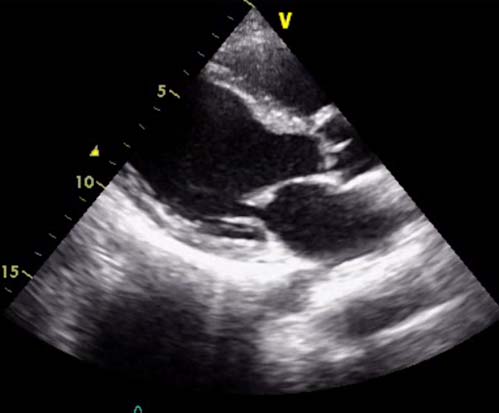
A 41-year-old healthy gentleman sustained a fall following which he developed a fibular fracture and compartment syndrome requiring fasciotomy. He subsequently developed acute kidney injury secondary to rhabdomyolysis and was admitted under Department of Nephrology. Patient underwent eight sessions of haemodialysis via right internal jugular venous access and over few days recovered from acute kidney injury and was discharged home. Ten days later patient was brought to internal medicine department with fever of 3 days and altered sensorium. On arrival to hospital he was drowsy. General examination revealed tachycardia (130/min) and hypotension (systolic blood pressure of 90 mmHg in right hand supine position). Systemic examination revealed grade 4 pansystolic murmur in the mitral area radiating to axilla and left sided cerebellar signs. Patient did not report any history of prior cardiac disease nor any history of IV drug abuse. Laboratory investigations on arrival showed anaemia (Haemoglobin 8.8mg/dl), leukocytosis (Total leucocyte count 14,400cells /cu.mm) and normal renal and hepatic functions. Computed tomography of the brain showed an acute left cerebellar infarct [Table/Fig-1]. Two dimensional echocardiogram showed a 0.8cm x 1.0cm dangling structure on Posterior mitral leaflet of mitral valve,1.0cm x 0.8cm vegetation on anterior mitral leaflet with severe eccentric mitral regurgitation, normal bi-ventricular systolic function with an ejection fraction of 68% [Table/Fig-2,3]. Three sets of blood cultures were drawn 2 hours apart from peripheral venipuncture sites. Using the Biomerieux BacT/ALERT 3D method, Methicillin Resistant Staphylococcus aureus (MRSA) sensitive to vancomycin, linezolid and resistant to rifampicin, doxycycline, co-trimoxazole was isolated. Patient was in addition tested negative for MRSA carrier status.
Non-Contrast Computed tomography of the brain depicting hypodensity in the left cerebellar hemisphere suggestive of acute infarct.
Trans-thoracic echocardiogram in parasternal long axis view showing vegetation of size 0.8cm x 1.0cm on the posterior mitral leaflet on left atrium side.

Trans-thoracic echocardiogram in apical four chamber view showing eccentric regurgitant jet (in blue colour) reaching to full length of the left atrium wall suggesting severe mitral regurgitation.
Treatment was initiated with intra-venous Vancomycin at dosage of 30mg/kg body weight in two divided doses. Vancomycin was given for a total of 14 days. A pair of blood culture repeated on 5th, 10th and 14th day of therapy showed MRSA to be persistent and the MIC of Vancomycin determined by Biomerieux VITEK 2 method increased from 0.5 to 2.0. Patient continued to be febrile. Repeated transthoracic echocardiograms showed increase in the size of vegetation suggesting treatment failure. In view of MRSA demonstrating vancomycin creep phenomenon (with increasing MICs from 0.5 to 2), treatment was switched over from vancomycin to daptomycin with regular monitoring of renal parameters including serum urea, serum creatinine and serum potassium and serum creatinine kinase. Daptomycin was initiated intravenously with 6mg/kg body weight every 24th hourly and increased to 9mg/kg body weight once a day on third day as patient tolerated the drug. Following initiation of Daptomycin, fever spikes reduced and patient became afebrile on day 3. Subsequent blood cultures drawn on 5th day of therapy was sterile. Frequent two dimensional transthoracic Echocardiogram performed on 10th, 20th, 26th day of Daptomycin therapy, demonstrated gradual decrease in vegetation size with disappearance of vegetation on 26th day of therapy [Table/Fig-4].
Trans thoracic echocardiogram in parasternal long axis view showing disappearance of vegetation after six weeks of antibiotic therapy.
Thus, patient with virulent Staphylococcus aureus demonstrating vancomycin creep phenomenon was successfully treated with Intravenous Daptomycin.
On follow-up after four weeks of treatment completion, patient’s general condition improved. Repeat two dimensional echocardiogram revealed severe mitral regurgitation and no residual vegetations. Patient was referred to Cardiothoracic department for mitral valve repair which was done successfully and is doing well on follow-up.
Discussion
Staphylococcus aureus is one of the most common causes of infective endocarditis including prosthetic valve endocarditis, acute infective endocarditis and intra-venous (IV) drug abuse associated endocarditis and health care associated infective endocarditis [1,2]. Right sided endocarditis is common in IV drug addicts and left sided infective endocarditis is primarily seen in non addicts [1]. Left sided Staphylococcus aureus endocarditis has worse prognosis compared to right sided endocarditis in terms of morbidity and mortality [3,4]. The rising incidence of MRSA further complicates the management of endocarditis [5]. Vancomycin has been the standard treatment of MRSA infections including endocarditis [6,7]. However, vancomycin has high failure rates in MRSA infective endocarditis due to poor penetration of valvular tissue and weak bactericidal action [8].
Vancomycin resistance in MRSA could be due to thickened and poorly cross-linked cell wall or due to acquisition of vanA resistance operon from Enterococcus species [9]. MRSA isolates are inhibited by vancomycin at MICs of 0.5 to 2 μg/ml typically. However, MRSA isolates which demonstrate MICs between 4 and 8 μg/ml have been termed as vancomycin intermediate Staphylococcus aureus and those with MICs >16 μg/ml as vancomycin resistant Staphylococcus aureus [10]. Gradual rise in MICs for vancomycin in susceptible Staphylococcus aureus isolates has been termed as vancomycin creep phenomenon and this has been a known occurrence [11–15]. In our case, MICs for vancomycin increased steadily from 0.5 μg/ml to 2 μg/ml suggestive of treatment failure. MRSA blood stream infections with strains demonstrating higher MICs (>1.5mg/l) have been associated with significantly higher mortality.
As per IDSA guidelines, in adult patients with MRSA bacteraemia and vancomycin treatment failure, high dose daptomycin in combination with other agents like linezolid, rifampicin, doxycycline, trimethoprim- sulfamethoxazole, gentamicin is recommended as alternative therapy [16]. However, recent studies emphasise daptomycin and ceftaroline combination (Salvage therapy) for MRSA strains with reduced susceptibility to glycopeptides and lipopeptides [17–19]. In our case, daptomycin alone was administered at a higher dose (9mg/kg) for total duration of 6 weeks and patient responded to therapy.
MRSA endocarditis demonstrating vancomcyin creep phenomenon is a very rare entity. The first reported case of VRSA endocarditis was a Eustachian valve endocarditis in a 33-year-old lady with a history of IV drug abuse [20]. Pranathi Rao et al., described a case of tricuspid and mitral valve endocarditis due to MRSA exhibiting vancomycin creep phenomenon [17].
Valve replacement therapy in native valve MRSA endocarditis is recommended in following scenarios: (a) large vegetation (more than 10 mm in diameter); (b) occurrence of more than 1 embolic event during the first 2 weeks of therapy; (c) severe valvular insufficiency; (d) valvular perforation or dehiscence; (e) decompensated heart failure; (f) perivalvular or myocardial abscess; (g) new heart block; or (h) persistent fevers or bacteraemia [16]. In this case, patient had severe mitral regurgitation with increasing vegetation size and an embolic event (left sided cerebellar infarct). Hence, he underwent mitral valve replacement with mechanical prosthesis following clearance of bacteraemia. Thus, MRSA infective endocarditis with vancomycin creep phenomenon was successfully treated with daptomycin.
Conclusion
MRSA left sided endocarditis is a rare entity with higher rates of embolic phenomenon. Vancomycin has been used as a standard first line agent for treatment of MRSA infections. With the occurrence of vancomycin creep phenomenon, MRSA bacteraemia with infective endocarditis carries a poor prognosis and high mortality. Daptomycin can be used as a good alternative in such patients to improve outcomes.
Thus, we would like to emphasise the occurrence of vancomycin creep phenomenon and alert the clinicians of such virulent strains.
[1]. Miro JM, Anguera I, Cabell CH, Chen AY, Stafford JA, Corey GR, International Collaboration on Endocarditis Merged Database Study Group. Staphylococcus aureus native valve infective endocarditis: report of 566 episodes from the International Collaboration on Endocarditis Merged DatabaseClin Infect Dis 2005 41(4):507-14. [Google Scholar]
[2]. Fowler VG, Miro JM, Hoen B, Cabell CH, Abrutyn E, Rubinstein E, Staphylococcus aureus Endocarditis: A consequence of medical progressJAMA 2005 293(24):3012-21. [Google Scholar]
[3]. Slabbekoorn M, Horlings HM, van der Meer JT, Windhausen A, van der Sloot JA, Lagrand WK, Left-sided native valve Staphylococcus aureus endocarditisNeth J Med 2010 68(11):341-47. [Google Scholar]
[4]. Fernández Guerrero ML, González López JJ, Goyenechea A, Fraile J, de Górgolas M, Endocarditis caused by Staphylococcus aureus: A reappraisal of the epidemiologic, clinical, and pathologic manifestations with analysis of factors determining outcomeMedicine (Baltimore) 2009 88(1):1-22. [Google Scholar]
[5]. Garau E, Bouza J, Chastre F, Gudiol S, Harbarth Management of methicillin-resistant Staphylococcus aureus infectionsClinical Microbiology and Infection 2009 15:125-136. [Google Scholar]
[6]. Boucher H, Miller LG, Razonable RR, Serious infections caused by methicillin-resistant Staphylococcus aureusClin Infect Dis 2010 51(Suppl 2):S183-97. [Google Scholar]
[7]. Mermel LA, Farr BM, Sherertz RJ, Raad II, O’Grady N, Harris JS, Infectious Diseases Society of America; American College of Critical Care Medicine; Society for Healthcare Epidemiology of America. Guidelines for the management of intravascular catheter-related infectionsClin Infect Dis 2001 32(9):1249-72. [Google Scholar]
[8]. Akinosoglou K, Apostolakis E, Marangos M, Pasvol G, Native valve right sided infective endocarditisEur J Intern Med 2013 24(6):510-19. [Google Scholar]
[9]. Foucault ML, Courvalin P, Grillot-Courvalin C, Fitness cost of VanA-type vancomycin resistance in methicillin-resistant Staphylococcus aureusAntimicrob Agents Chaemother 2009 53(6):2354-59. [Google Scholar]
[10]. Walters M, Lonsway D, Rasheed K, Albrecht V, McAllister S, Limbago B, Investigation and Control of Vancomycin-resistant Staphylococcus aureus: A Guide for Health Departments and Infection Control Personnel 2015 Atlanta, GA [Google Scholar]
[11]. Steinkraus G, White R, Friedrich L, Vancomycin MIC creep in non-vancomycin-intermediate Staphylococcus aureus (VISA), vancomycin-susceptible clinical methicillin-resistant S. aureus (MRSA) blood isolates from 2001-05J Antimicrob Chaemother 2007 60(4):788-94. [Google Scholar]
[12]. Chang W, Ma X, Gao P, Lv X, Lu H, Chen F, Vancomycin MIC creep in methicillin-resistant Staphylococcus aureus (MRSA) isolates from 2006 to 2010 in a hospital in ChinaIndian J Med Microbiol 2015 33:262-66. [Google Scholar]
[13]. Wang G, Hindler JF, Ward KW, Bruckner DA, Increased vancomycin MICs for Staphylococcus aureus clinical isolates from a university hospital during a 5-year periodJ Clin Microbiol 2006 44(11):3883-86. [Google Scholar]
[14]. Ho PL, Lo PY, Chow KH, Lau EH, Lai EL, Cheng VC, Vancomycin MIC creep in MRSA isolates from 1997 to 2008 in a healthcare region in Hong KongJ Infect 2010 60(2):140-45. [Google Scholar]
[15]. Kehrmann J, Kaase M, Szabados F, Gatermann SG, Buer J, Rath PM, Vancomycin MIC creep in MRSA blood culture isolates from Germany: a regional problem?Eur J Clin Microbiol Infect Dis 2011 30(5):677-83. [Google Scholar]
[16]. Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Infectious Diseases Society of America. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and childrenClin Infect Dis 2011 52(3):e18-55. [Google Scholar]
[17]. Sundaragiri PR, Vallabhajosyula S, Haddad TM, Esterbrooks DJ, Tricuspid and mitral endocarditis due to methicillin-resistant Staphylococcus aureus exhibiting vancomycin-creep phenomenonBMJ Case Rep 2015 2015:211974 [Google Scholar]
[18]. Sakoulas G, Moise PA, Casapao AM, Nonejuie P, Olson J, Okumura CY, ntimicrobial salvage therapy for persistent staphylococcal bacteraemia using daptomycin plus ceftarolineClin Ther 2014 36(10):1317-33. [Google Scholar]
[19]. Barber KE, Werth BJ, Rybak MJ, The combination of ceftaroline plus daptomycin allows for therapeutic de-escalation and daptomycin sparing against MRSAJ Antimicrob Chaemother 2015 70(2):505-09. [Google Scholar]
[20]. Alreja G, Lotfi A, Eustachian valve endocarditis: Rare case reports and review of literatureJournal of Cardiovascular Disease Research 2011 2(3):181-85. [Google Scholar]