Rare Site of Parasitic Dermoid Cyst at Uterovesical Fold of Peritoneum with Absent One-Sided Adnexa
Sunita Dubey1, Alka Sehgal2, Puneeti Ballega3, RPS Punia4
1 Assistant Professor, Department of Obstetrics and Gynaecology, Government Medical College and Hospital, Chandigarh, India.
2 Professor, Department of Obstetrics and Gynaecology, Government Medical College and Hospital, Chandigarh, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, Government Medical College and Hospital, Chandigarh, India.
4 Professor, Department of Pathology, Government Medical College and Hospital, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunita Dubey, Government Medical College and Hospital, Sector 32, Chandigarh-160030, India.
E-mail: Sunitas504@gmail.com
Teratomas are the most common type of germ cell tumour. It can be congenital or acquired and are usually found in gonads (testes and ovaries). Parasitic dermoid cysts are rare and their actual incidence is unknown. We are reporting a case of 25-year-old gravida two, para one and one living child, who underwent emergency cesarean section in view of symptomatic placenta previa. A parasitic dermoid cyst was found incidently in front of uterus which was attached to uterovasical fold of bladder. This cyst did not show any connection to uterus or adnexa. Uterus, uterine cavity, right side tube and ovary were normal. Her left sided fallopian tube and ovary was completely absent. She did not have any symptoms related to the dermoid cyst. Histopathology confirmed parasitic mature dermoid cyst.
Adnexal mass, Germ cell tumour, Placenta previa
Case Report
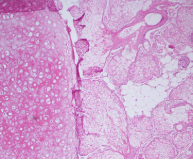
A 25-year-old pregnant women gravida two, para one with one living child came with complaints of painless, excessive bleeding from vagina. She underwent emergency cesarean section at 32+4 weeks period of gestation in view of symptomatic placenta previa. Her first baby was delivered vaginally. There were no predisposing factors for placenta previa in present pregnancy except multiparity. Intraoperatively, baby was lying in vertex presentation and there were no adhesions in the pelvis or in the abdomen. Uterus, uterine cavity, right sided tube and ovary were normal but her left sided fallopian tube and ovary was completely absent [Table/Fig-1]. A 6x4x1cm bluish coloured cystic mass was found incidently in front of uterus and that was attached to uterovesical fold of bladder. It was easily separated and didn’t show any connection to the uterus or any of the adnexae [Table/Fig-2]. During separation, it was ruptured, dark brown coloured thick fluid with hairs were visible in it. On microscopic examination, cystic mass was composed of mature tissue from all the three germ layers. The most common elements of ectoderm were stratified squamous epithelial cells with hairs and attached pilosebaceous units. The solid part was composed of well differentiated structures like mature adipose tissue and mature cartilage. Few bits of corpus luteum were seen. Final diagnosis of mature cystic teratoma was made [Table/Fig-3].
Intraopertive findings revealed normal shape of the uterus, Presence of Parasitic dermoid cyst lying over the peritoneum of uterovesical fold with brownish discharge coming out of it.
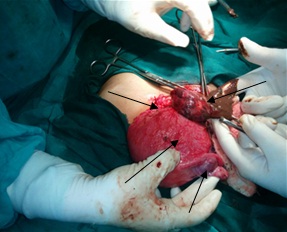
Separated dermoid cyst over the peritoneum of uterovesical fold.

Mature dermoid cyst (H&E stains, magnification 40X). Main components of the cyst are pilosebaceous unit, cartilage and adipose tissue cells.
Postoperatively, patient was asked for any symptoms in relation to the presence of this parasitic dermoid cyst; but she was totally asymptomatic. Her baby was died few hours after birth due to birth asphyxia. Autopsy of the baby was not done. She was discharged on day 4 of cesarean section and she was lost on follow-up.
Discussion
Dermoid cysts accounts for 5-25% of all ovarian cell neoplasms and usually occurs during reproductive period between 20–30 years of age [1]. Dermoid cyst arising from germ cell sources are mostly found in paraxial and midline locations, they can be congenital or acquired when found in gonads but they are always congenital when found at extragonadal locations like intracranial, cervical, retroperitoneal, mediastinal and sacrococcygeal site. Parasitic dermoid cysts are extremely rare entities and their actual incidence is unknown.
Several theories exist to explain their occurrence. Torsion of the dermoid cyst may be the cause of autoamputation and reimplantation of the dermoid cyst at rare sites. This is probably extrapolated from the fact that torsion of the pedicle is the most frequent complication of ovarian teratomas. The incidence of torsion is more common during pregnancy and puerperium and it has been reported in 16% of cases [1]. An ectopic ovary may occurs congenitally or following pelvic inflammatory disease and after a surgical procedure [2]. This patient had no history of laparotomy and there were no evidence of adhesions in the pelvis. So, ectopic ovary may not be the cause of parasitic dermoid cyst in this case. Abnormal arrest of germinal cells in the dorsal mesentery during their embryonic migration to the genital ridge may lead to development of multiple ovary and subsequently formation of parasitic dermoid cyst at various sites [3].
Few similar cases of parasitic dermoid cysts which are reported in the literature are summarized [Table/Fig-4] [2,4-13]. Here in the present case, parasitic dermoid cyst was present along with absent left fallopian tube and ovary. With intraoperative findings precluding any uterine malformation in present case, the above postulations failed to explain the absence of left fallopian tube as well the viability of the cyst in absence of any obvious vascular pedicle.
Descriptions of parasitic dermoid cyst at different locations [2,4-13].
| Author name (year),Ref. number | Presenting complaints | Site of parasitic dermoid cyst | Diagnosis | Prognosis |
|---|
| Ushakov FB et al., (1998) [4] | Pain abdomen | Omentum | Parasitic mature dermoid cyst | good |
| CK khoo et al., (2008) [5] | Incidentally found during right ovarian dermoid cystectomy | Pouch of douglas | Parasitic mature dermoid cyst with right ovarian dermoid | good |
| Bartlett CE (2009) [6] | Incidental finding during vaginal exaination | Pouch of douglas | Parasitic dermoid cystBilateral ovaries and fallopian tubes were present | good |
| Sinha R et al., (2009) [2] | Pain abdomen | All over the abdominal wall, omentum, pouch of douglas and dermoid cyst in the ovary | Multiple parasitic mature dermoid cysts with re-ocurrence in same ovary | good |
| Peitsidou A et al., (2009) [7] | Incidental finding during cesarean section | Pouch of douglas | Parasitic mature dermoid cyst with absent one ovary. | good |
| Wahba AH (2010) [8] | Chronic pelvic pain with recent complained of perception of something moving inside her abdomen | Median umbillical fold of peritoneum | Parasitic mature dermoid cyst with absent one ovary | good |
| Cucinella G et al., (2011) [9] | Pain lower abdomen | Anterior abdominal wall | Parasitic mature dermoid cyst with absent one ovary | good |
| Shetty NS et al., (2013) [10] | Incidental finding | Indirect inguinal hernia | Parasitic mature dermoid cyst with absent one ovary | good |
| NS. Chitrakar et al (2015) [11] | Pain and swelling in lower abdomen | Parasitic dermoid cyst in hepatorenal space and left twisted dermoid cyst in situ | Parasitic mature dermoid cyst with absent right side fallopian tube and ovary | good |
| Saini SR et al., (2016) [12] | Incidentally found & presented with obstructed labour at term | Pouch of douglas | Parasitic mature dermoid cyst with bilateral normal ovaries | good |
| Lee KH et al., (2016) [13] | Pain abdomen | Omentum | Benign mature teratoma left ovary, with absent right ovary and parasitic mature dermoid at omentum | good |
| Present case (2016) | Incidental finding during cesarean section | Uterovesical fold of peritoneum | Parasitic mature dermoid cyst with absent one sided adnexa | good |
Clinically, most women with dermoid cysts are asymptomatic as in this patient. Torsion is not uncommon. Rupture of dermoid cysts with spillage of sebaceous material can occur, but is uncommon. Shock and haemorrhage are the sequelae of rupture; dense adhesions may form secondary to marked granulomatous reaction. Literature also reveals rupture of intracranial and spinal dermoid that leads to scattering of fat droplets within the ventricles and cerebrospinal fluid space. Rare complication like fistula with the urinary bladder has also been reported. Incidence of risk on the same ovary is about 3–4% after cystectomy. Sinha et al., reported postsurgical recurrence all over the abdominal wall and in the ovary as well in a patient who had undergone an excision of ovarian dermoid cyst earlier [2]. Contrarily a rare condition associated with either mature or immature teratomas is Anti-N-Methyl-Daspartate (NMDA) receptor encephalitis [14]. Patients develop a multistage illness that progresses from psychosis, memory deficits, seizures, and language disintegration into a state of unresponsiveness with catatonic features. Though malignancy rates is 0.2 to 2%, the factors linked to malignant transformation include age over 45 years, tumour diameter greater than 10cm, rapid growth, and low resistance intra-tumour flow on doppler imaging [15]. Histopathologically specimen should be evaluated for Rokitansky’s protuberance which is a solid prominence located at the junction between the teratoma and normal ovarian tissue. This area draws its significance for having peak cellular variety, hence important for excluding immature/malignant components. Ultrasound has a low sensitivity and high specificity in the diagnosis of dermoid cyst. Due to high sensitivity of MRI for the presence of fat, even the rare lesion that contains microscopic fat can be well differentiated.
Conclusion
Assessment of adnexal mass should be done by transvaginal ultrasonography along with tumour markers to establish the risk of malignancy. Magnatic resonance imaging should be done whenever there is difficulty in making diagnosis. Parasitic dermoid cysts are ideally managed laproscopically by simple resection. The risk of granulomatous peritonitis can be reduced by decompression of the cyst within an impermeable bag prior to removal. To increase the likelihood of detecting recurrent disease, frequent follow-ups after cystectomy are also necessary in young patients who are at high risk of recurrence.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
[1]. Peterson WF, Prevost EC, Edmunds FT, Handley JM, Morris FK, Benign cystic teratoma of the ovary: a clinico-statistical study of 1007 cases with review of the literatureAm J Obstet Gynecol 1955 70:368-82. [Google Scholar]
[2]. Sinha R, Sundaram M, Lakhotia S, Multiple intraabdominal parasitic cystic teratomasJ Minim Invasive Gynecol 2009 169(6):789-91. [Google Scholar]
[3]. Oosterhuis JW, Stoop H, Honecker F, Looijenga LH, Why human extragonadal germ cell tumours occur in the midline of the body: old concepts, new perspectivesInt J Androl 2007 30:256-63. [Google Scholar]
[4]. Ushakov FB, Meirow D, Prus D, Libson E, Ben Shushan A, Rojansky N, Parasitic ovarian dermoid tumour of the omentum: A review of the literature and report of two casesEur J Obstet Gynecol Reprod Biol 1998 81:77-82. [Google Scholar]
[5]. Khoo CK, Chua I, Siow A, Chern B, Parasitic dermoid cyst of the pouch of Douglas: a case reportJ Minim Invasive Gynecol 2008 15(6):761-63. [Google Scholar]
[6]. Bartlett CE, Khan A, Pisal N, Parasitic dermoid cyst managed laparoscopically in a 29-year-old woman: a case reportJ Med Case Reports 2009 3:63 [Google Scholar]
[7]. Peitsidou A, Peitsidis P, Goumalatsos N, Papaspyrou R, Mitropoulou G, Georgoulias N, Diagnosis of an autoamputated ovary with dermoid cyst during a Cesarean sectionFertil Steril 2009 91(4):1294 [Google Scholar]
[8]. Wahba AH, Unreported location and presentation for a parasitic ovarian dermoid cyst: A case reportMiddle East Fertility Society Journal 2010 15:216-18. [Google Scholar]
[9]. Cucinella G, Granese R, Venezia R, Mangione D, Calagna G, Perino A, Parasitic dermoid cyst coexisting with absence of an adnexaActa Obstet Gynecol Scand 2011 90(6):677-78. [Google Scholar]
[10]. Shetty NS, Vallabhaneni S, Patil A, Babu MM, Baig A, Unreported location and presentation for a parasitic ovarian dermoid cyst in an indirect inguinal herniaHernia 2013 17:263-65. [Google Scholar]
[11]. Chitrakar NS, Suwal S, Neupane S, Bilateral ovarian teratoma: one parasitic twisted in-situ and another parasitic at the hepato renal spaceJ Nepal Health Res Counc 2015 13:166-68. [Google Scholar]
[12]. Saini SR, Jindal P, Pachauri P, Gupta R, Parasitic dermoid cyst: obstructed laborThe New Indian Journal of OBGYN 2016 3(1):58-60. [Google Scholar]
[13]. Lee KH, Song MJ, Jung IC, Lee YS, Park EK, Autoamputation of an ovarian mature cystic teratoma: a case report and a review of the literatureWorld Journal of Surgical Oncology 2016 14:217 [Google Scholar]
[14]. Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodiesLancet Neurol 2008 7:1091-98. [Google Scholar]
[15]. Hackethal A, Brueggmann D, Bohlmann MK, Franke FE, Tinneberg HR, Münstedt K, Squamous-cell carcinoma in mature cystic teratoma of the ovary: systematic review and analysis of published dataLancet Oncol 2008 9:1173 [Google Scholar]