Pseudo-Exstrophy of Bladder with Unilateral Renal Agenesis: A Rare Combination of two Anomalies
Abdolhamid Amouei1, Mohammad Baghi Yazdi2, Fatemeh Ehsani3, Mojtaba Babaei Zarch4
1 General Surgeon, Pediateric fellowship, Surgery ward, Shahid Sadoughi University of Medical Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2 School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3 General Surgery Resident, Surgery Ward, Shahid Sadoughi University of Medical Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohammad Baghi Yazdi, School of Medicine, Shahid Sadoughi university of Medical Sciences, Yazd, Iran. Email: drbaghi7272@yahoo.com
Pseudo-exstrophy of bladder is an uncommon condition characterized by the major musculoskeletal defects without urinary system defects. A two-day-old female neonate was presented with pseudo-exstrophy of the bladder and unilateral renal agenesis- A rare combination of two anomalies. She was born at 37 weeks gestational age with caesarean section delivery. The X-ray of hip revealed pubic diastasis. Ultrasonography clearly showed absence of the left kidney with a normal right kidney. The patient was treated successfully with proper surgical management. We, hereby, report a rare variant case of pseudo-exstrophy of bladder with lower set umbilicus and infra-umbilical midline of lower anterior abdominal wall defect in a neonate who was born in Shahid Sadoughi Hospital, Yazd, Iran.
Congenital anomaly, Musculoskeletal defects, Surgical management
Case Report
A two-day-old female neonate, weighing about 2910gms at birth was presented with swelling in the lower abdomen, above the pubic area. She was born at 37 weeks gestational age with caesarean section delivery. There was no evidence of urinary or fecal incontinence. Physical examination revealed a low-set umbilicus, a defect between umbilical and symphysis pubis and widening of the symphysis pubis. On physical examination, spinal alignment was not normal. Labia majora were separated and the anus was in normal site but the patient had widened perineum [Table/Fig-1].
Preoperative view, showing low-set umbilicus, lower wall abdominal defect and labia majora were separated with widened premium.

The vital signs were as follow: pulse rate 138 beats/ min, temperature 36.7°C, respiratory rate 40 breaths/min, and O2 saturation 95%.
The laboratory tests including haemoglobin, White Blood Cell (WBC) count, neutrophils, lymphocytes, platelet count, blood glucose, Blood Urea Nitrogen (BUN), serum creatinine, sodium; potassium, serum albumin, Aspartate Aminotransferase (AST), Alanine Aminotransferase (ALT) and C-Reactive Protein (CRP) all were in normal range. The urine analysis and serum biochemistry were normal. Echocardiography (ECG) revealed a normal heart. The neonate was made NPO and was monitored. The neonate was infused intravenously by dextrose10% with 3meq/kg NaCl. The X-ray revealed widening of the symphysis pubis (more than 4cm) and scoliosis [Table/Fig-2]. Ultrasonography revealed absence of the left kidney with a normal right kidney.
Abdominal X-ray at birth showing wide diastasis of the symphysis pubis, and scoliosis of vertebrae.

Cystography was performed for evaluating bladder volume and vesico ureteral reflux. [Table/Fig-3]. Bladder volume was normal and there was no evidence of vesicoureteral reflux.
Preoperative cystography.

As the pubic diastasis was greater than 4cm, pelvic osteotomy was planned to repair the abdominal wall and pubic diastasis. An Orthopedic surgeon performed osteotomy of innominate bone in the superior part of acetabulum and closed symphysis pubis [Table/Fig-4]. The osteotomy site was fixed by pin. Bladder and urethra was freed from the abdominal wall. Then, the pubic was closed with 0 silk sutures. The abdominal wall was closed successfully. Repairing of perineum and external genitalia was delayed to 3 to 6 month later. The surgeon explained the disease to the parents and noticed them about another surgery next 3 to 6 month. It was informed that patients with this problem usually have normal urinary continence and internal sphincter mechanisms usually are intact. We requested adequate nutrition, use of postoperative antibiotics, ureteral stenting catheter and postoperative immobilization.
Postoperative view after osteotomy and pubic closure.

Discussion
Variants of the bladder exstrophy complex are rare. Pseudo-exstrophy is an exstrophy variant which has all the characteristics of the classical exstrophy without urinary tract defects [1]. The incidence of classic exstrophy is approximately 1 in 40,000 births. Exstrophy variants are less common [2], and pseudo-exstrophy of bladder has been described as an uncommon condition [3]. Hejtmancik et al., described the term “pseudo-exstrophy” in 1954. They reported a case of severe bladder prolapse between divergent abdominal muscles with intact bladder and no evidence of exstrophy [4]. Clinically, pseudo-exstrophy is the most benign form of the exstrophy [5]. This condition is associated with musculoskeletal defect, anteposed anus but the urethra is intact [6].
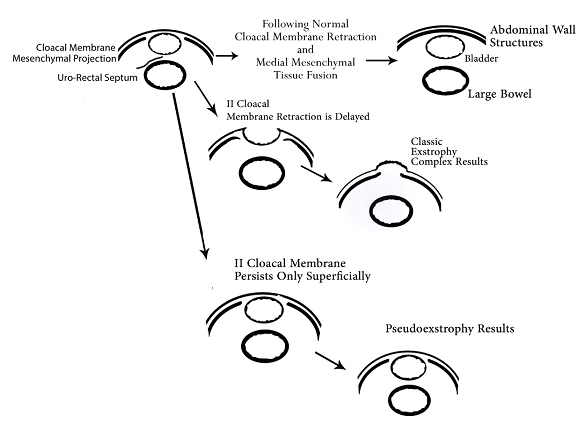
This [Table/Fig-5] which is adopted from William Mitchell et al., shows emberyological events of classic and pseudo-exstrophy of the bladder [7].
Embryologic events occurring during development of layers of lower anterior abdominal wall are diagrammatically depicted for normal fetus (top), classic exstrophy complex (middle), and pseudo-exstrophy (bottom) [7].
Pseudo-exstrophy is characterized by low-set umbilicus, lower rectus diastasis and pubic split pelvic and separated labia majora [8]. The characteristic findings of pseudo-exstrophy on prenatal ultrasonography include a wide communication between cystic mass and bladder, lying the mass below two umbilical arteries, persistent of mass as gestation progress and usually accompanying by a diastasis of the pubic bones [3].
Classic exstrophy is predominant in males. In contrast, variants are usually seen in females [8]. Our patient was a female neonate.
Renal anomalies occur with pseudo-exstrophy in rare cases [8]. Recently, See Min Choi et al., reported a case of pseudo-exstrophy of bladder which was diagnosed prenatally by ultrasonography. In their case, both kidneys and upper urinary tracts were normal [3]. We found unilateral renal agenesis in our case. Previously, only a few cases of pseudo-exstrophy have been reported in the literature and pseudo-exstrophy with unilateral renal agenesis and wide pubic diastasis (greater than 4 cm) has not previously been described. In our case, in addition to pseudo-exstrophy, right kidney was absent. The pubic diastasis was greater than 4 cm and pelvic osteotomy was needed to repair the abdominal wall and pubic diastasis. This case report was the second case of this anomaly which was treated with surgical strategy successfully. This case is interesting because of its rarity and combination of two rare anomalies. There is no standard surgical strategy for pseudoexstrophy with wide pubic diastasis [2]. In patients with bladder exstrophy who have wide pubic diastasis (greater than 4 cm), are older than 72 hour, or are undergoing bladder closure, concurrent osteotomy increases the reliability of pelvic ring closure [9].
To our knowledge, our case is the first report of pseudo-exstrophy with unilateral renal agenesis. This congenital disease is usually diagnosed and treated in neonates. We advocated the surgical management for closing pubic and abdominal wall reconstruction.
Conclusion
Although pseudo-exstrophy with unilateral renal agenesis is the first case in worldwide but this anomaly is clinically important. Surgery was performed successfully in female neonate with this rare condition.
[1]. Mahajan JK, Ojha S, Rao KL, Pseudoexstrophy with epispadiasUrologia internationalis 2005 74(4):365-67. [Google Scholar]
[2]. Otake K, Uchida K, Inoue M, Koike Y, Matsushita K, Oki S, Staged management of pseudoexstrophy with omphalocele and wide pubic diastasisJournal of Pediatric Surgery Case Reports 2014 2(8):388-90. [Google Scholar]
[3]. Choi SM, Park T, Park JK, Shin JK, Choi WJ, Lee SA, Pseudoexstrophy of the bladder diagnosed prenatallyPrenatal Diagnosis 2013 33(10):1002-03. [Google Scholar]
[4]. Hejtmancik JH, King WB, Magid MA, Pseudo-exstrophy of bladderThe Journal of Urology 1954 72(5):829-32. [Google Scholar]
[5]. Lowentritt BH, Van Zijl PS, Frimberger D, Baird A, Lakshmanan Y, Gearhart JP, Variants of the exstrophy complex: a single institution experienceThe Journal of Urology 2005 173(5):1732-37. [Google Scholar]
[6]. Turner WR, Jr., Ransley PG, Bloom DA, Williams DI, Variants of the exstrophic complexThe Urologic Clinics of North America 1980 7(2):493-501. [Google Scholar]
[7]. Mitchell W, Venable D, Patel AJ, PseudoexstrophyUrology 1993 41(2):134-36. [Google Scholar]
[8]. Meisheri IV, Kasat LS, Bahety G, Sawant V, Kothari P, Kumar A, Pseudoexstrophy of the bladder: a rare variantPediatric Surgery International 2001 17(2-3):224-25. [Google Scholar]
[9]. Meldrum KK, Baird AD, Gearhart JP, Pelvic and extremity immobilization after bladder exstrophy closure: complications and impact on successUrology 2003 62(6):1109-13. [Google Scholar]