Multilocular Mesothelial Cyst of the Spleen Mimicking Hydatid Cyst on Imaging
Asmita Parihar1, Usha Rani Singh2, Vineeta Rathi3, Vivek Agrawal4
1 Senior Resident, Deparment of Pathology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
2 Professor, Deparment of Pathology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
3 Professor, Deparment of Radio-diagnosis, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
4 Professor, Deparment of Surgery, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asmita Parihar, 8/3 Gulmohar Road, Shipra Sun City, Indirapuram, Ghaziabad-201014, Uttar Pradesh, India.
E-mail: dr.asmitaparihar@gmail.com
Splenectomy, Splenic hydatidosis, Unilocular anechoic lesions
A 38-year-old, previously healthy lady presented to our hospital with complaints of pain in the left upper abdomen for the past two years. There was associated nausea and mild decrease in appetite. She had no past history of trauma and there were no other complaints. Abdominal examination did not reveal any organomegaly. Systemic examination and laboratory investigations were within normal limits.
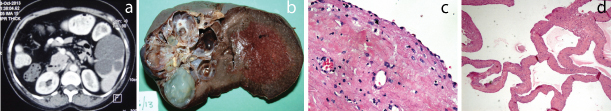
Contrast Enhanced Axial Computerized Tomography (CECT) scan of the abdomen revealed a large, oval, multilocular, non-enhancing, cystic lesion in the anterior part of the spleen. There was no calcification in the lesion and the rest of the spleen was normal in attenuation. No other cysts were seen in the abdomen. A diagnosis of splenic hydatid cyst was made in view of presence of a cystic lesion showing multiple thin internal septations [Table/Fig-1a].
(a) CECT shows a multilocular, non-enhancing cystic lesion in the spleen; (b) Gross specimen of the spleen with multilocular cyst filled with gelatinous material; (c) Microscopy shows cyst lined by mesothelial cells (H&E stain, 400X); (d) Low power view of mesothelial cyst (H&E stain, 40X).
Per-operatively, spleen had a cyst at the antero-inferior aspect with splenic vein dilatation. Splenectomy was done and the surgical specimen was sent to the Department of Pathology for histopathological examination.
On gross examination, the spleen measured 10x9x4.5 cm. The external surface showed lobulations at one pole. The cut surface showed a multilocular cyst measuring 6x5.5x4 cm at the anterior pole. The cysts were variably sized ranging from 0.5 to 2.5 cm in diameter. They were filled with gelatinous material and inner wall was smooth. The adjacent splenic parenchyma appeared unremarkable [Table/Fig-1b]. Microscopy revealed a true multilocular cyst lined by mesothelial cells [Table/Fig-1c&d]. There was no other type of lining or evidence of squamous metaplasia on thorough sampling of the lesion. Surrounding splenic parenchyma showed mild congestion. Thus, a diagnosis of multilocular mesothelial cyst of the spleen was made. Postoperatively, patient is doing well at 6 months follow-up.
Cysts in the spleen are rarely encountered in clinical practice. Splenic cysts can be classified as parasitic or non-parasitic [1]. Parasitic cysts constitute a major fraction [2]. They are caused by the cestode Echinococcus granulosus, resulting in hydatid disease [2]. Histopathologically, hydatid cyst shows characteristic three layered cyst- germinal layer with daughter cysts and protoscolices, laminated membrane and outer fibrovascular layer. The non-parasitic ones can be either true cysts, with an epithelial or endothelial lining; or false cysts which are devoid of any lining and are usually, a result of trauma. Epithelial cysts, the rarest amongst all the types of splenic cysts, can be epidermoid, dermoid or mesothelial, depending upon their lining [1]. These epithelial cysts are usually unilocular [3]. Vijayaraghavan R et al., have described unilocular mesothelial cyst in spleen [4]. Manoj MG et al., have reported a multilocular epithelial cyst [5]. Their exact aetio-pathogenesis is still unknown. It has been suggested that these develop from invagination of the surface mesothelium with subsequent fluid accumulation [6].
The epithelial cysts occur predominantly in the second and third decade of life [3]. They grow slowly, may present as left upper quadrant abdominal pain, organomegaly or as an incidental finding, diagnosed on ultrasonography. They are usually unilocular [3]. Our case had a multilocular splenic cyst, which is an infrequent finding.
The characteristic radiologic picture of epithelial splenic cysts has been described as unilocular anechoic lesions with smooth, well defined margins [3]. However, these findings are not specific. The further sub-categorization of epithelial cysts into epidermoid, dermoid and mesothelial can only be done on histopathological examination.
Splenic hydatidosis, the most common splenic cystic lesion can have similar appearance as that of epithelial splenic cysts on Computed Tomography (CT) and Ultra Sonography (USG) examination [7]. Hydatid cysts can be classified into four types based on their radiological appearance. Type 1 is simple cyst with no internal architecture. Type 2 is cyst with accompanying daughter cyst and matrix. Type 3 is calcified cyst and type 4 is complicated cyst which has ruptured or become infected [8]. In our case, the CT findings were suggestive of Type 2 hydatid disease as the cystic lesion comprised of multiple small locules, which mimicked daughter cysts in appearance. Radiologically it would be almost impossible to differentiate between the rare entity of a multilocular mesothelial cyst and a splenic hydatid cyst with multiple daughter cysts.
Recent studies have shown that Magnetic Resonance Imaging (MRI) is more helpful in differentiating between parasitic and non-parasitic cysts. T2-weighted MRIS characteristically show a low intensity rim in cases of hydatid disease [8]. In our patient, MRI was not done.
The present case shows that there can be diagnostic confusion on radiologic examination. Thus, the final diagnosis can only be provided on histopathological examination. Microscopy of true cysts show a fibro-collageneous wall lined by an epithelium, which can be either low cuboidal or squamous. Some consider this squamous epithelium to be a metaplastic response and thus prefer the term mesothelial cysts with focal squamous metaplasia [6]. Our case showed only a mesothelial lining.
In recent years, there has been a change in the treatment modalities of splenic cysts. The focus has shifted from complete splenectomy to more conservative approaches [1]. Partial splenectomy is increasingly being done, trying to preserve as much of the splenic parenchyma as possible. The decision regarding the exact surgical procedure depends upon the size of the cyst and the type of cystic lesion. Complete splenectomy in cases of hydatid disease ensures complete removal of cyst, avoidance of cyst fluid spillage and related complications, and reduction in the chances of recurrence. Partial splenectomy is preferred in cases of small, non-parasitic cysts, as it preserves the immunological function of spleen. Therefore, an accurate pre-operative diagnosis can prevent serious post-splenectomy complications. In our case, as hydatidosis was suspected, complete splenectomy was performed to prevent spillage of cystic fluid and to ensure complete removal of germinative membranes.
Conclusion
Multilocular splenic epithelial cysts are uncommon lesions. They may mimic the appearance of a parasitic cyst on imaging studies, i.e., sonography and CT scan. Therefore, it is important to keep the possibility of epithelial cyst in mind when dealing with cystic lesions of spleen. Histopathological examination is required to confirm the subtype of splenic cyst.
[1]. Schlittler LA, Dallagasperina VW, Non-parasitic splenic cystsRev Col Bras Cir 2010 37:442-46. [Google Scholar]
[2]. Morgenstern L, Nonparasitic splenic cysts: pathogenesis, classification, and treatmentJ Am Coll Surg 2002 194:306-14. [Google Scholar]
[3]. Palmieri I, Natale E, Crafa F, Cavallaro A, Mingazzini PL, Epithelial splenic cystsAnticancer Res 2005 25:515-21. [Google Scholar]
[4]. Vijayaraghavan R, Chandrashekar R, Aithal S, Rashmi MV, Belagavi CS, Mesothelial cyst of the spleen in an adult: a case reportBMJ Case Rep 2010 2010 [Google Scholar]
[5]. Manoj MG, Misra P, Kakkar S, Multilocular epithelial cyst of spleen: a rare occurrenceIndian J Pathol Microbiol 2012 55:602-04. [Google Scholar]
[6]. Bürrig KF, Epithelial (true) splenic cysts. Pathogenesis of the mesothelial and so-called epidermoid cyst of the spleenAm J Surg Pathol 1988 12:275-81. [Google Scholar]
[7]. Adas G, Karatepe O, Altiok M, Battal M, Bender O, Ozcan D, Diagnostic problems with parasitic and non-parasitic splenic cystsBMC Surg 2009 9:9 [Google Scholar]
[8]. Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A, Hydatid disease from head to toeRadiographics 2003 23:475-94. [Google Scholar]