Colocolic Intussusception in a Child with Pathologic Lead Point Along with Intestinal Malrotation-A Rare Case Report and Brief Review
Prasanta Kumar Tripathy1, Pradeep Kumar Jena2
1 Assistant Professor, Department of Pediatric Surgery, SVP Post Graduate Institute of Pediatrics, Cuttack, Odisha, India.
2 Professor, Department of Pediatric Surgery, SVP Post Graduate Institute of Pediatrics, Cuttack, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prasanta Kumar Tripathy, Arunodaya Nagar, Link Road, Cuttack -753012, Odisha, India.
E-mail: drpktripathy555@gmail.com
Intestinal obstruction in children is frequently caused by intussusception and intestinal malrotation and when these two conditions co-exist, it is called Waugh’s syndrome. Intussusception cases in children are mostly ileocolic, whereas, the colocolic variety is a rare entity and very few cases have been reported in literature. In all the reported cases of Waugh’s syndrome, the intussusceptions were ileocolic type except one case, where colocolic type was mentioned with lymphangoima as Pathological Lead Point (PLP). We report a seven-year-old child of colocolic intussusception with juvenile polyp being the PLP along with intestional malrotation. It is an extremely rare association which has not been reported previously.
Bilious vomiting, Juvenile polyp, Ladd’s procedure, Waugh’s syndrome
Case Report
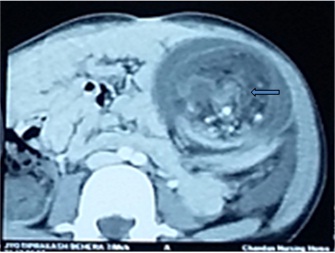
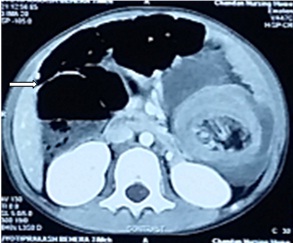
A seven-year-old boy presented to us with complaints of pain abdomen, bilious vomiting and bleeding per rectum, since five days. Pain was colicky in nature; more marked in left lower abdomen initially and thereafter, became generalized. He was referred from a private hospital with CT scan of abdomen. At admission patient was dehydrated and having bilious nasogastric aspirate. Although he had tachycardia, his respiratory rate was normal. Abdomen was distended, tender and an irregular lump was palpable in left lower quadrant. Bowel sounds were absent. Digital rectal examination revealed an intra-luminal mass and blood stained fingers. Abdominal CT scan with contrast suggested left sided colocolic intussusceptions [Table/Fig-1] and associated malrotation [Table/Fig-2].
CT scan axial image showing left sided colocolic intusussception (arrow); soft tissue mass with alternate areas of low and high attenuation in left side of abdomen.
CT scan with contrast showing intestinal malrotation with dilated small bowel loops (arrow) on right side.
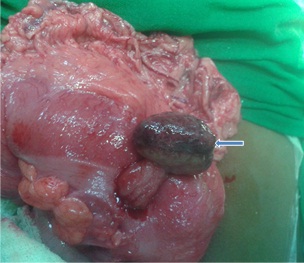
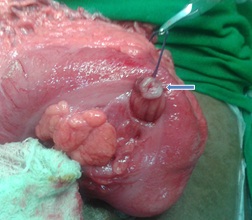
After resuscitation, emergency laparotomy was done. A long left sided colocolic intussusceptions was detected, where the transverse colon was invaginated into descending colon with apex at the distal sigmoid colon. Intussusception was reduced successfully. The intussuscepted colon was looking congested, for which warm saline-soaked laparatomy pad was applied for five minutes. The normal pink colour of bowel returned. After ensuring the viability, bowel was looked for any lead point and we palpated an intra-luminal mass in mid-transverse colon. Transverse colon was opened above the mass by longitudinal incision and a pedunculated polyp of 4cm diameter was found [Table/Fig-3]. The polyp was excised and colotomy incision was closed [Table/Fig-4]. Histopathology report suggested juvenile polyp with extensive inflammatory cell infiltration and haemorrhage. Further, we noted features of malrotation, the right colon and cecum being mobile and duodeno-jejunal junction on right side of midline. Therefore, Ladd’s procedure was performed. Post-operative recovery was uneventful. Nasogastric tube was removed after the output became non-bilious and minimal. The child was discharged after suture removal on oral diet and in good condition. During follow-up of six months, the child had no further problems related to gastrointestinal tract and was gaining weight.
Large pedunculated polyp (arrow) in mid-transverse colon acting as a pathologic lead point for colocolic intussusceptions.
Polyp excised through ligation of stump (arrow) through longitudinal colotomy incision.
Discussion
Both intussusception and malrotation are common occurrence in infants and children. The association between them was first reported by George E Waugh in 1911 and thereafter, authors continue to describe it as “Waugh’s syndrome” [1]. However, this association is rarely reported in literature [2]. In children, ileocolic intussusception is the most common type of intussusception comprising of 95% of cases followed by ileoileocolic type [3,4]. Colocolic intussusceptions are usually seen in adults along with a pre-existing colonic pathology which acts as a lead point [5]. They are very rare in paediatric population and no studies have been documented to know the exact prevalence of the disease [5,6].
Likewise among all the reported cases of Waugh’ syndrome, the intussusception are of ileocolic type except one report of colocolic variety in which lymphangioma was the Pathological Lead Point (PLP) [7]. Again 95% of intussusceptions in children are idiopathic without pathologic lead point. PLP is detected in only few patients, with Meckel’s diverticulum being the most common finding [3]. Our case is extremely rare because, it was a colocolic intussusception in a seven-year-old child where transverse colon bearing a large polyp as PLP was invaginated into descending and sigmoid colon along with malrotation. All these unusual findings prompted us towards extensive search of literature. Colocolic intussusception with juvenile polyp as PLP has been reported in children [6].
But, the association of colocolic intussusception with a large juvenile polyp in transverse colon being the PLP along with intestinal malrotation has not been reported in children. Some authors suspect intestinal malrotation pre-disposes to intussusception, as a mobile right colon may be a pre-requisite for intussusceptions [8,9]. Although juvenile polyps are not uncommon, a large polyp in transverse colon causing colocolic intussusception in children is uncommon. Again associated malrotation made our case report typical. Although both the bowel pathology was present from infantile period it became clinically apparent and acute at the age of seven years. Intussusception is uncommon at 7 years of age as 90% of cases of intussusceptions are found below 3 years of age and occur in the region of ileocecal valve [3,4]. The classical triad of crampy abdominal pain, palpable mass and bloody stool is seen in only 21% of intussusceptions [4], but, it was clearly manifested in our patient. Because of a gradual and distal obstruction and not a very young age of patient, bowel necrosis did not occur even after five days.
One prospective study indicated strong association between intussusception and malrotation [10]. But the association is rarely published, thereafter, leading to its disappearance. Many cases of intussusceptions are reduced non-surgically by air or contrast enema, leaving malrotation unrecognized, if present. Many authors feel a higher incidence of Waugh’s syndrome than actually reported [9,11]. Non-operative management of intussusceptions may not be adequate in Waugh’s syndrome as associated malrotation can lead to volvulus in the future. After operation obstructive symptoms secondary to malrotation may be misdiagnosed as recurrent intussusceptions. Surgeons and radiologists must have high index of suspicion in diagnosing both the pathology if associated. A prospective study is required to find out actual incidence of malrotation in patients with intussusception during ultrasonography.
Conclusion
Intestinal malrotation may co-exist with intussusception. If obstruction persists after reduction of intussusception, an associated malrotation may be misdiagnosed as recurrent intussusception. PLP should be searched for, when operating on a child with colocolic intussusception. Waugh’s syndrome should be kept in mind during operative and non-operative management of intussusception.
[1]. Waugh GE, Referred penile pain in intussusception with notes of three casesThe Lancet 1911 I:1492-94. [Google Scholar]
[2]. Al-Momani H, Waugh syndrome: A report of 7 patients and review of the published reportsAnn Saudi Med 2014 34(6):527-31. [Google Scholar]
[3]. Columbani PM, Scholz S, Intussusception In: Coran AG, Adzick NS, Krummel TM, Laberge JM, Shamberger RC, Caldamone AA. EditorsPaediatric Surgery 2012 7th edElsevier Saunders:1093-1110. [Google Scholar]
[4]. Mahumudloo R, Gheibi S, Vahed SN, Colocolic Intussusception without lead point; A case report and literature reviewIran J Paediatr 2008 18(4):373-76. [Google Scholar]
[5]. Shalaby MS, Rollo DD, Adikibi B, Brindley N, Left sided colo-colic intussusceptions in a child with acute lymphoblastic leukemiaJ Paediatr Surg Case Reports 2014 2:228-31. [Google Scholar]
[6]. Abrahams RB, Franco A, Lewis KN, Paediatric colocolic intussusception with pathologic lead point: A case reportJ Med Cases 2012 3(1):84-88. [Google Scholar]
[7]. Al-Jahdali A, Lees GM, Gay DP, Al-Sairafi R, Colocolic intussusceptions in a preterm infant with intestinal malrotationJ Paediatr Surg 2009 44(12):e17-18. [Google Scholar]
[8]. Chirdan LB, Uba AF, Association of midgut malrotation with intussusceptionsNigeria J Surg Res 2005 7:159-61. [Google Scholar]
[9]. Breckon VM, Hadley GP, Waugh’s syndrome: A report of six patientsPaediatr Surg Int 2000 16(5-6):370-73. [Google Scholar]
[10]. Brereton RJ, Taylor B, Hall CM, Intussusception and malrotation in infants: Waugh’s syndromeBritish Journal of Surgery 1986 73:55-57. [Google Scholar]
[11]. Baltazar G, Sahyoun C, Sime J, Bitar M, Bitar J, Rao AC, Discovery of a case of Waugh’s syndrome during a mission to HaitiInt J Surg Case Rep 2012 3(1):22-24. [Google Scholar]