Central Telangiectatic Osteosarcoma of the Mandible in a Paediatric Patient: A Rarity
Divya Tomar1, Manu Dhillon2, Muhamad Nishad Thayath3, Iram Zaidi4, Shikha Singh5
1 Senior Lecturer, Department of Pedodontics and Preventive Dentistry, SBB Dental College and Research Centre, Ghaziabad, Uttar Pradesh, India.
2 Reader, Department of Oral Medicine and Radiology, ITS Centre for Dental Studies and Research, Ghaziabad, Uttar Pradesh, India.
3 Professor and Head, Department of Pedodontics and Preventive Dentistry, SBB Dental College and Research Centre, Ghaziabad, Uttar Pradesh, India.
4 Reader, Department of Pedodontics and Preventive Dentistry, SBB Dental College and Research Centre, Ghaziabad, Uttar Pradesh, India.
5 Reader, Department of Pedodontics and Preventive Dentistry, SBB Dental College and Research Centre, Ghaziabad, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manu Dhillon, Department of Oral Medicine and Radiology, ITS Centre for Dental Studies and Research, Delhi-Meerut Road, Ghaziabad-201206, Uttar Pradesh, India.
E-mail: drmanudhillon@yahoo.co.in
Osteosarcoma (OS) involving the head and neck region is rare and is a diagnostic challenge due to its aggressive nature and varied presentations. Although OS constitute 40% to 60% of all bone tumours, only 10% of these occur in the head and neck region, most commonly in the maxilla and mandible. OS of the jaw bone has a different pattern and behaviour when compared to OS at other anatomic location. It occurs in a more elderly population, less aggressive and usually spreads locally rather than distant metastases. Telangiectatic Osteosarcoma (TOS) of jaws in a paediatric patient is still a very rare variant and till date only two cases have been reported in literature. Radiographic evaluation plays an important role as the clinical symptoms are not specific to the condition. Conventional radiography should always be supplemented by advanced imaging modalities for the diagnosis, which gives a three dimensional assessment and also prevents superimposition of surrounding structures. Early diagnosis and radical surgery are the keys to high survival rates. Herein, we present a third ever reported case of TOS occurring in mandible of a nine-year-old male patient.
Bone neoplasm, Child, Radiology
Case Report
A nine-year-old male patient reported to the Department of Oral Medicine and Radiology with chief complaint of swelling on left side of the lower jaw since, one month [Table/Fig-1]. The onset of the swelling was gradual in duration. Over the ensuing month, it increased in size and became painful. Pain was dull, gnawing and continuous in nature which aggravated on applying pressure. The swelling was not associated with hypoesthesia or mobility of associated teeth. The patient was otherwise healthy with no significant medical or dental history. Extra oral examination revealed facial asymmetry due to the swelling and left submandibular and cervical lymph nodes were palpable, firm in consistency, mobile and tender on palpation.
Extra-oral photograph showing the swelling in the left lower part of the mandible.

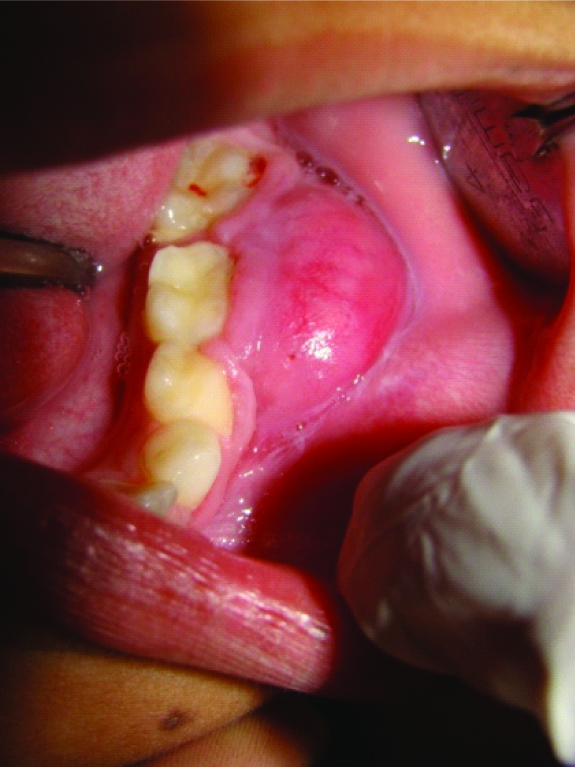
Intra-oral examination revealed an oval swelling on the left mandibular buccal gingiva and vestibule with normal overlying mucosa. The swelling was on the attached gingiva measuring approximately 38 mm antero-posteriorly extending from the distal aspect of tooth #73 to the distal aspect of tooth #36 and approximately 24 mm superior-inferiorly extending from the marginal gingiva to the buccal vestibule [Table/Fig-2]. The swelling was causing vestibular obliteration and was exophytic, sessile and well defined. On palpation the swelling was non-mobile, non-compressible, hard in consistency and tender. Considering the age of the patient and based on clinical examination a provisional diagnosis of benign fibro-osseous lesion and differential diagnosis of Osteosarcoma (OS) was made.
Intra-oral photograph showing extension of the lesion and complete obliteration of buccal vestibule.
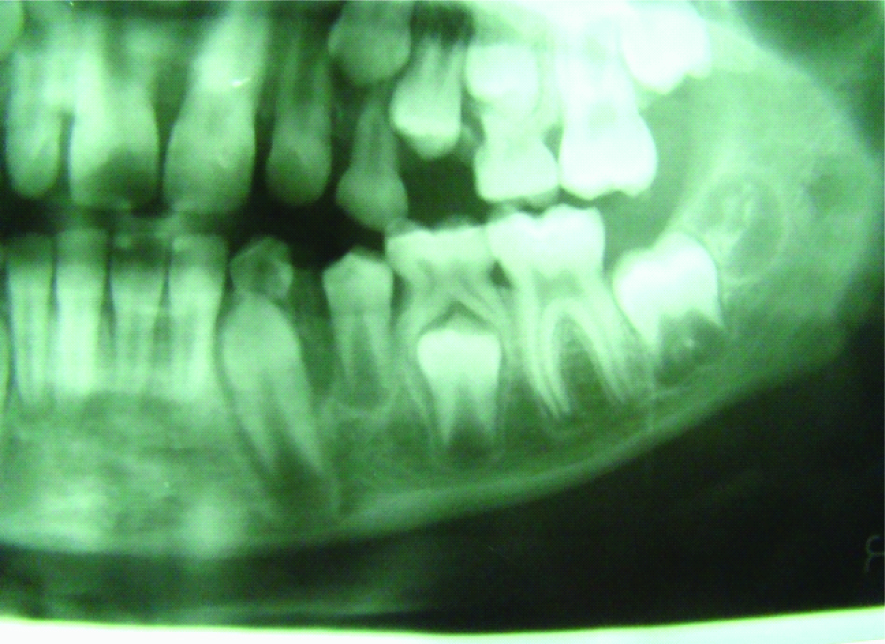
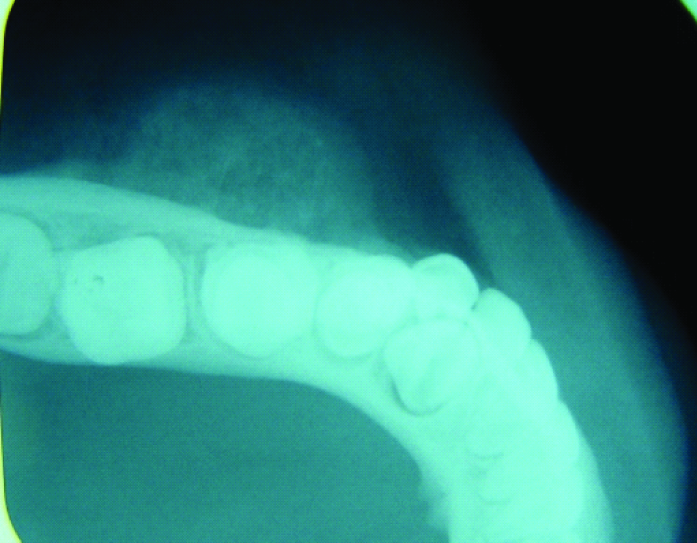
The radiographic evaluation included the Intra-Oral Periapical Radiograph (IOPA), mandibular lateral occlusal radiograph and panoramic radiograph. The IOPA and panoramic radiograph revealed mixed dentition stage. There was widening of the Periodontal Ligament Space (WPLS) with an irregular absence or attenuation of the lamina dura in relation to 74, 75 and 36. The disruption of follicular space and lining in relation to unerupted 35 was evident [Table/Fig-3]. The mandibular lateral occlusal radiograph was taken with reduced exposure parameters which showed the presence of fine radial spicule and mild erosion of the cortex in relation to 75 [Table/Fig-4].
Cropped panoramic radiograph showing widening of periodontal ligament space and disruption of follicular space.
Lateral occlusal radiograph with reduced exposure revealed fine radial spicule on buccal aspect.
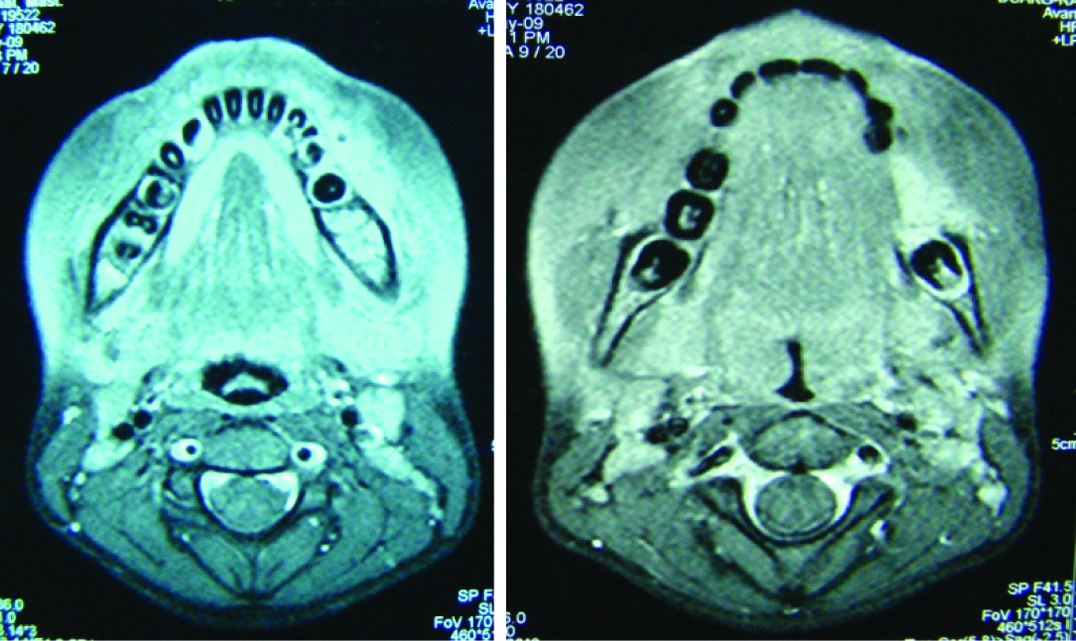
Computed Tomography (CT) confirmed the conventional radiological findings. It revealed hypodense lesion involving the body of the mandible with soft tissue component. Magnetic Resonance Imaging (MRI) revealed patchy altered marrow in the body of left half of the mandible with erosion of the alveolar margins which appeared hypointense on T1, hyperintense on T2 weighted images and showed heterogenous enhancement [Table/Fig-5]. There were also multiple enlarged lymph nodes at levels 1a, 1b and 2 of the neck bilaterally.
Axial MRI section revealed altered marrow on left body of mandible which appears hyperintense on T2 weighted image.
(a) H&E stain-10X, (b) H&E stain-40X showing blood filled spaces with delicate calcified osteoid like areas and anaplastic tumour cells.
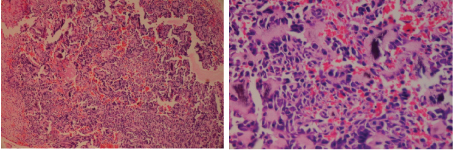
Incisional biopsy was performed under local anesthesia. Histopathological examination revealed large and small blood filled spaces with delicate calcified osteoid like areas with atypical and pleomorphic tumour cells. Anaplastic tumour cells were also seen frequently [Table/Fig-6a,b]. Based on the histopathological features a diagnosis of osteogenic sarcoma telangiectatic type was made.
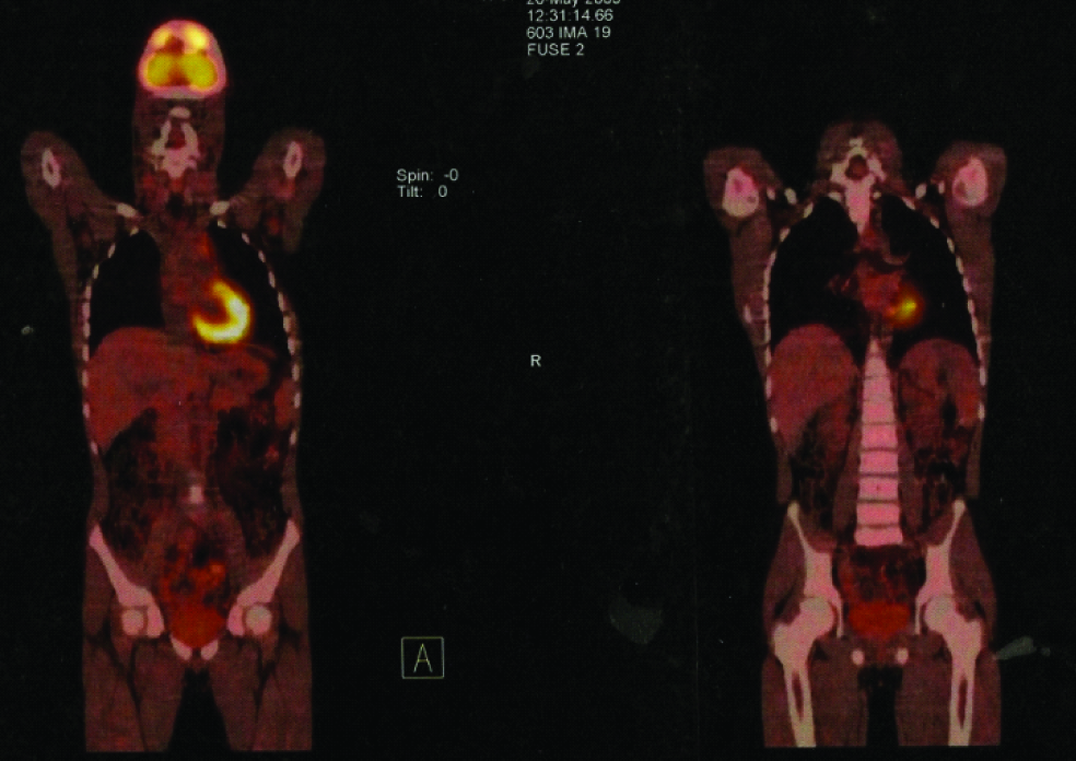
The patient was referred to higher center for further treatment. Whole body PET-CT scan was also performed for the evaluation of any metastasis which showed no area of abnormal isotope uptake [Table/Fig-7].
PET-CT scan showing no area of abnormal isotope uptake.
Discussion
OS of the head and neck region are relatively rare and aggressive tumours accounting for only 1% of all head and neck malignancies [1]. Although OS represent the most common non-haematopoietic primary malignant bone tumour with an overall incidence of 1:100,000 per year [2], OS of the head and neck region represent only 6% to 10% of all cases [3]. OS of head and neck occur somewhat later in life, most commonly in the third and fourth decades when compared to OS of long bones which usually occurs in young patients and have equal sex pre-disposition [4,5].
Till date only two cases of TOS has been reported in literature. The first case was of a 15-year-old Chinese girl who died 16 months after the diagnosis with direct cerebral invasion [6]. The second case was reported in a 13-year-old girl who underwent aggressive hemi-mandibulectomy and was free of disease after 7 years follow-up [7]. This is a first ever reported case of TOS affecting the mandible in a very young male patient.
Telengiactatic OS (TOS) was first described by Paget in the year 1854. Originally, it was considered to be a malignant bone aneurysm. Ewing considered this entity as a variant of OS [8]. OS usually occurs as a secondary tumour, following radiation therapy to other tumours. Association of OS with syndromes and pre-existing benign tumours has been established in literature [2]. In our case as the patient was only nine-year-old, the possibility of pre-existing disease is unlikely and there was no associated syndrome present. Our case is unique and rare in a way that the patient was only 9 years unusually young for OS of jaw bones but this age is expected age for TOS occurring elsewhere in the body [8]. Most of the cases of OS are asymptomatic but in symptomatic patients the common symptoms includes pain, swelling, parasthesia, mobility of teeth and facial asymmetry [4]. Swelling was the only complaint in the present case.
Matsuno T et al., has given a diagnostic criterion for TOS [8]. The criterion suggests, presence of lytic or destructive lesion on a radiograph without sclerosis, gross cavity with little solid tumour tissue and single or multiple blood contained cystic cavities or necrosis with presence of anaplastic cells histopathologically. In the present case radiographs showed poorly defined irregular destructive bone lesion. On the occlusal radiograph, there was presence of sun burst or sun ray appearance in the form of thin radio opaque whips, which were reported to be seen in OS and central haemangioma. The formation of codmans triangle was also evident. This appearance was due to periosteal reaction and indicates that the neoplasm has penetrated the cortex and extended into soft tissue. There was no lesional sclerosis on CT.
Radiological diagnosis of OS of the jaw can be difficult because of its variable appearance. Bianchi SD et al., classified radiological appearance of OS of the jaw into three categories [9]. The first type shows diffuse, irregular destruction of bone resembling bony erosion evident on conventional radiography. The second type shows small amount of calcification which is better evident on a CT than conventional radiography. The bone formation resembles the initial phases of fibrous dysplasia and ossifying fibroma. The third type which was most common in the case series was with lamellar ossification. Conventional radiography was found to be equally effective when compared with CT in diagnosing lamellar type [9].
TOS is a distinct entity and many other lesions are there which needs to be differentially diagnosed from TOS histopathologically. In the present case, the tumour was differentiated from Aneurysmal Bone Cyst (ABC) and giant cell granuloma. ABC is an expansive destructive, hemorrhagic, tumour like condition, thought to represent a benign reactive vascular process [7]. Both ABC and TOS resemble histopathologically, but unlike TOS, mesenchymal stromal cells in ABC are benign in nature. ABC may form as a secondary component in few benign bony lesions and OS [7]. Central giant cell granuloma and central giant cell tumour does not show large sinusoidal spaces. In the present case, there was presence of blood filled spaces with delicate calcified osteoid like areas and anaplastic tumour cells.
The treatment of choice in OS is wide surgical resection with adequate margin. Improved results with adjuvant chemotherapy for OS of extremities are documented. However, controversies for using radiotherapy and chemotherapy as a treatment modalities for OS of jaws exists [4]. These modalities are recommended for the patients, if the surgical margins of the lesion are questionable or positive. The prognosis of OS of the jaws remains poor because of the local recurrences and distant metastasis. Matsuno T et al., in the case series documented that, most of the patients of TOS (92%) developed metastasis and died within an average of 10 months after diagnosis [8].
Conclusion
TOS of the jaw bones are very rare and may give varied presentations both clinically and radiographically. Histopathologically, the differentiation between TOS and ABC is very important because of the similar microscopic features. Early diagnosis and prompt aggressive surgical intervention is the key for better prognosis.
[1]. Weber RS, Benjamin RS, Peters LJ, Ro JY, Achon O, Goepfert H, Soft tissue sarcomas of the head and neck in adolescents and adultsAm J Surg 1986 152:386-92. [Google Scholar]
[2]. Sturgis EM, Potter BO, Sarcomas of the head and neck regionCurr Opin Oncol 2003 15:239-52. [Google Scholar]
[3]. Caron AS, Hajdu SI, Strong EW, Osteogenic sarcoma of the facial and cranial bones. A review of forty-three casesAm J Surg 1971 122:719-25. [Google Scholar]
[4]. Laskar S, Basu A, Muckaden MA, D’Cruz A, Pai S, Jambhekar N, Osteosarcoma of the head and neck region: lessons learned from a single-institution experience of 50 patientsHead Neck 2008 30:1020-26. [Google Scholar]
[5]. Clark JL, Unni KK, Dahlin DC, Devine KD, Osteosarcoma of the jawCancer 1983 51:2311-16. [Google Scholar]
[6]. Chan CW, Kung TM, Ma L, Telangiectatic osteosarcoma of the mandibleCancer 1986 58:2110-15. [Google Scholar]
[7]. Naik LK, Shetty P, Teerthanath S, Jagadeesh HM, Telengiectaic osteosarcoma affecting the mandibleJ Oral Maxillofac Pathol 2014 18(Supply S1):143-46. [Google Scholar]
[8]. Matsuno T, Unni KK, McLeod RA, Dahlin DC, Telangiectatic osteogenic sarcomaCancer 1976 38:2538-47. [Google Scholar]
[9]. Bianchi SD, Boccardi A, Radiological aspects of osteosarcoma of the jawsDentomaxillofac Radiol 1999 28:42-47. [Google Scholar]