Delayed Uterine Necrosis: Rare Cause of Nonhealing Wound
Aruna Nigam1, Neha Gupta2, Arifa A Elahi3, Zeeba S Jairajpuri4, Swaraj Batra5
1 Professor, Department of Obstetrics and Gynaecology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
2 Associate Professor, Department of Obstetrics and Gynaecology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
3 Assistant Professor, Department of Obstetrics and Gynaecology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
4 Associate Professor, Department of Pathology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
5 Professor, Department of Obstetrics and Gynaecology, Hamdard Institute of Medical Sciences and Research, Jamia Hamdard, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aruna Nigam, Flat No 6, Type 4 Quarters, Lady Hardinge Medical college campus, Shaheed Bhagat Singh Marg, New Delhi 110001, India.
E-mail: prakasharuna@hotmail.com
Uterine necrosis is a very rare condition and most of the reported cases occurred after pelvic arterial embolization for post-partum haemorrhage, embolization of fibroid uterus or application of B–Lynch sutures. A case of delayed myometrial necrosis is reported in post-cesarean patient where no embolization or uterine compression sutures have been applied. Patient presented with foul smelling discharge from the gaped abdominal wound following caesarean section. Abdomen was closed after exploration and lavage. Patient did not have complete healing and area of unhealed wound remained through which subinvoluted uterus was peeping out. Patient was taken for resuturing again but the uterus was found to be completely necrotic and hysterectomy was performed. Patient responded to treatment.
Caesarean section, Postpartum, Necrosis, Non-healing wound, Obstructed labour
Case Report
A 22-year-old primiparous woman presented with foul smelling discharge from the abdominal stitchline for 4 days and fever for 2 days. She delivered a dead male foetus of 3.4 Kg by lower caesarean section for prolonged second stage of labour after 2 days of labour trial and failed forceps application 15 days back. There was no history of post-partum haemorrhage or uterine artery ligation in the operative notes.
General examination revealed severe pallor with a pulse rate 100/ minute, blood pressure 120/86mmHg and temperature 102OF. Cardiovascular and respiratory examination was normal. Abdominal examination revealed a 26 week size uterus with gaped transverse stitch line through which copious purulent discharge was coming and a part of uterus was visualized. Thus a provisional diagnosis of burst abdomen was made. Investigations revealed haemoglobin of 6.1gm/dl and Total Leukocyte Count (TLC) 18,200/dl. Ultrasonography of abdomen revealed subinvoluted uterus with collection in abdomen.
Intravenous broad spectrum antibiotics (Injection ceftriaxone, Metronidazole and Gentamycin) were started and two units packed Red Blood Cells (RBCS) were transfused. In view of burst abdomen and collection in abdomen, patient was undertaken for re-exploration. Peroperatively uterus was subinvoluted and its lower segment caesarean section scar was dehisced. There was no lochiometra/pyometra or retained foreign body. Lavage of the abdominal cavity was done along with uterine repair. Abdomen was closed in layers along with tension sutures. She received two packed RBCS after laparotomy. Post-operatively antibiotics were changed according to culture sensitivity. The stitch removal was done on 12th Post-operative day after which the T-shaped scar gaped in the lower part having some serosanguinous discharge. The gaped wound was triangular (3cm x 3cm x3cm) in shape with mild slough at base [Table/Fig-1]. Uterine height was still at 18 weeks.
Gaped non-healing anterior abdominal wound.

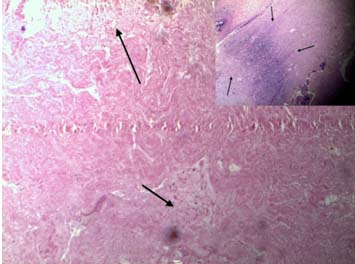
Patient was afebrile and was discharged with advice of daily dressing and planned resuturing once the wound is healthy. She was given doxycycline for two weeks although her wound discharge came to be sterile. Although she was afebrile and had no bladder or bowel complaints, wound remained unhealthy with increase in discharge. The tissue prolapsing through the gaped wound was necrotic, pale and fragile. She was taken for wound debridement and it was realized that necrotic tissue was the anterior wall of uterus which was gangrenous. Sub-total hysterectomy was done in view of gangrenous anterior wall of uterus. Histopathological examination of tissue sent confirmed necrosed myometrial tissue with no granuloma [Table/Fig-2].
Photomicrograph showing large areas of necrosis and degeneration with collection of neutrophils. (Arrows) Inset shows scanner view of necrosis.
On post-operative day 14 stitch removal was done. She was given antibiotic (Amoxicillin + Clavulanic acid) for 5 days during post-operative period. Her wound healed completely and the patient was discharged in satisfactory condition.
Discussion
Uterine necrosis is a very rare condition and only few cases have been reported till date. Most of these cases have been reported after pelvic artery embolization [1,2] or rarely after B-Lynch sutures [3,4]. There are few cases where the uterine necrosis has been reported after group A Streptococcus infection [5,6].
Indications for caesarean sections are still being defined and every effort is being made to regulate the ever increasing numbers of caesarean sections. Medical facilities have improved over the last century and emphasis is laid on control of infections by clean operating techniques, prophylactic antibiotics and supervised and institutional delivery. Despite these efforts from the scientific community and governments in this regards, lack of standardized training and inadequate operating and labour room environment in many third world countries is still a major factor for post-partum infections. The major independent factors for puerperal infections are the anaemia and un-supervised deliveries conducted by midwives in developing countries.
Protocols suggested for infections of non-healing abdominal wound include adequate debridement and antibiotics covering the spectrum of infection [7,8].
Necrosis of uterus is a serious complication after caesarean section. Occasional case reports and series exist where most common reason for necrosis has been ligation of uterine artery to control post-partum haemorrhage. Use of B-Lynch sutures or arterial embolization by interventional radiologists has been reported as a cause of uterine necrosis after caesarean sections. All cases described have involved either rectus sheath or partial thickness of uterine wall [9,10]. Investigative modalities such as Magnetic Resonance Imaging (MRI) or pelvic Computed Tomography (CT) may aid in forming a diagnosis but management essentially remains total or sub-total hysterectomy.
The persistent uterine infection might be the reason of subinvoluted uterus and necrosis in this case. Severe infection that had spread to the abdominal cavity after the first surgery may have persisted in the uterine wall despite lavage and antibiotic cover during re-exploration. Hence, it is important to prevent infections by taking adequate steps before and during surgery.
Conclusion
Surgeons should be aware of the possibility of uterus being involved in cases of persistent infection. All efforts should be made to improvise the substandard care provided at the primary centres and institutional deliveries should be promoted to decrease the maternal morbidity.
[1]. Poujade O, Ceccaldi PF, Davitian C, Amate P, Chatel P, Khater C, Uterine necrosis following pelvic arterial embolization for post-partum haemorrhage: review of the literatureEur J Obstet Gynecol Reprod Biol 2013 170(2):309-14. [Google Scholar]
[2]. Belghiti J, Tassin M, Raiffort C, Zappa M, Poujade O, Bout H, Uterine necrosis after arterial embolization for post-partum haemorrhageGynecol Obstet Fertil 2014 42(2):126-28. [Google Scholar]
[3]. Lodhi W, Golara M, Karangaokar V, Yoong W, Uterine necrosis following application of combined uterine compression suture with intrauterine balloon tamponadeJ Obstet Gynaecol 2012 32(1):30-31. [Google Scholar]
[4]. Price N, Lynch C, Uterine necrosis following B-Lynch suture for primary postpartum haemorrhageBJOG 2006 113(11):1341 [Google Scholar]
[5]. Lurie S, Vaknine H, Izakson A, Levy T, Sadan O, Golan A, Group A. Streptococcus causing a life-threatening postpartum necrotizing myometritis: a case reportJ Obstet Gynaecol Res 2008 34(4 Pt 2):645-48. [Google Scholar]
[6]. Satia MN, Vibha S, Uterine necrosis in a case of B-Lynch brace sutureInt J Reprod Contracept Obstet Gynecol 2016 5(7):2466-69. [Google Scholar]
[7]. Bharatam KK, Sivaraja PK, Abineshwar NJ, Thiagarajan V, Thiagarajan DA, Bodduluri S, The tip of the iceberg: Post caesarean wound dehiscence presenting as abdominal wound sepsisInt J Surg Case Rep 2015 9:69-71. [Google Scholar]
[8]. Liu ZF, Wang JH, Cui BQ, Fan QB, Wang XJ, Zhao R, Resection and repair of large abdominal wall lesions in gynecologic patientsChin Med J (Engl) 2013 126(9):1673-77. [Google Scholar]
[9]. Matsubara S, Uterine necrosis after B-Lynch suture in a classical caesarean sectionAust N Z J Obstet Gynaecol 2013 53(6):595-96. [Google Scholar]
[10]. Akoury H, Sherman C, Uterine wall partial thickness necrosis following combined B-Lynch and Cho square sutures for the treatment of primary postpartum haemorrhageJ Obstet Gynaecol Can 2008 30(5):421-24. [Google Scholar]