Third molar surgery is one of the most common surgical procedures performed in general dentistry. The third molar surgery has following benefits like, relief of pain, prevention of periodontal disease and caries, prevention of dentigerous cyst formation, root resorption of the adjacent second molar and to facilitate orthognathic surgery and orthodontic treatment [1]. Third molar surgery has intra-operative and post-operative complications among which pain, swelling and trismus are the most common [2]. These complications after third molar surgery largely depend upon various surgical and patient related factors. Surgical factors include angulations and depth of the impacted tooth, the type of suture technique and duration of the surgical intervention [3], while patient related factors include age of the patient, compliance of post-operative instructions following surgery, obesity, smoking and use of oral contraceptives [4]. Various methods are used to minimize the post-operative sequelae which include administration of antibiotics like amoxicillin-clavulanic acid 2000mg/125mg, [5] Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), steroids [6] and enzymes and submucosal injections of dexamethasone and triamcinolone [7]. Each of the medications has their own side-effects and also depends largely on patient’s compliance factor.
Recently various studies have been conducted to analyze the use of a drain in association with the suture procedure in an attempt to alleviate or minimize post-operative sequelae, with mixed results [8–10]. The hypothesis behind use of drain in adjunct to suturing after third molar surgery is that a drain allows the patient to experience a more comfortable post-operative period in relation to the pain, swelling, and trismus, because it permits the drainage of the fluids located in the tissue spaces and could therefore be a technique recommended to minimize the post-operative sequelae [11]. Thus, the current study was undertaken to comparatively evaluate post-operative swelling, pain and trismus in patients after surgical removal of mandibular third molars with and without tube drain.
Materials and Methods
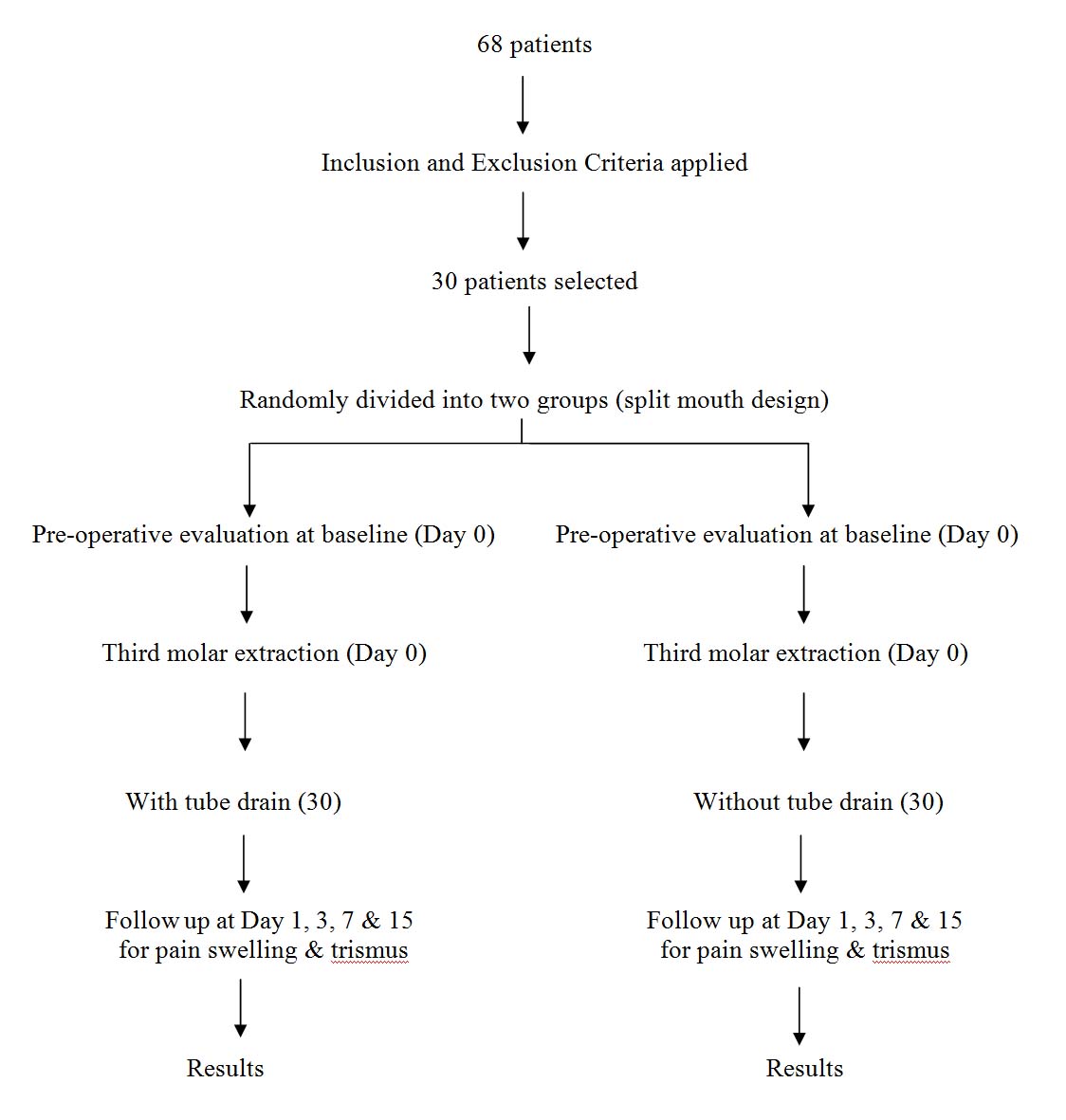
This prospective, split mouth study was conducted in the Department of Oral and Maxillofacial Surgery, Dr. D. Y. Patil Dental College and Hospital, Pune, Maharashtra, India. A total of 30 patients (18 males and 12 females), with bilateral impacted mandibular third molars were selected and before the beginning of active therapy, left and right mandibular quadrants of each individual were randomly allocated by means of a tossing coin into two groups, test (with tube drain, n=30) and control (without tube drain, n=30) groups. The eligible individuals were informed of the nature, possible risks, and benefits of their participation in the study and a written informed consent was obtained from each participant. Pre-surgical measurements were made. The surgical removal of impacted mandibular third molar of one side was executed. Evaluation was done on the 1st, 3rd, 7th and 15th post-operative days. Following the complete resolution of post-operative sequelae the second surgical procedure of other side with tube drain was carried out in the same patient. Similar post-operative evaluation was done on the second side [Table/Fig-1].
Sample Size: The ideal sample size calculation was done using G* Power software version 3.0.10 to ensure adequate power for the study. Thirty individuals per group were necessary to provide an 80% power with α of 0.05 and effect size of 0.582 calculated after obtaining the data from previous study [12].
Inclusion Criteria and Exclusion Criteria: Systemically healthy subjects between 18 to 50 years (both genders) and having bilaterally completely impacted mandibular third molars indicated for surgical removal were included.
Subjects having medical conditions that can complicate surgical extraction, obese subjects (BMI ≥ 30kg/m2), current smokers, pregnant or lactating females, those taking oral contraceptive drugs and those under any antibiotic coverage were excluded.
All potential participants were explained the need and design of the study. The details about the surgical procedure and possible complications associated with the same were also informed. An informed written consent accordingly was obtained from the patients before the study.
Pre-operative Evaluation: An intra-oral periapical radiograph was taken for assessment of third molar condition. For inclination and angulation of impacted mandibular third molars to the adjacent second molar an Orthopantogram (OPG) was obtained. Pre-surgical measurements were made for swelling, pain and maximum inter-incisal opening of mouth. All measurements were taken pre-operatively and post-operatively on days 1, 3, 7, and 15 for both procedures. Medications (capsule amoxicillin 500 mg TID, daily for 5 days and tablet diclofenac sodium 50mg TID, daily for 5 days) were prescribed 72 hours before the procedure. Pre-operative pain was measured using a Visual Analogue Scale (VAS) [Table/Fig-2] [13]. Routine laboratory investigations were carried out.
VAS to evaluate pain: Reference values given to patients.
| No pain | The patient feels well |
| Slight pain | If the patient is distracted he or she does not feel the pain |
| Mild pain | The patient feels the pain even if concentrating on some activity |
| Severe pain | The patient is very disturbed but nevertheless can continue with normal activities |
| Very severe pain | The patient is forced to abandon normal activities |
| Extremely severe pain | The patient must abandon every type of activity and feels the need to lie down |
Swelling was measured with the help of flexible ruler. Reference points for measurement of swelling were two lines, horizontal and vertical. Horizontal line corresponds to the distance between the commisure (corner of lip) and the ear lobe. The vertical line corresponds to the distance between the outer canthus of eye and angle of mandible [Table/Fig-3] [14]. Arithmetic mean of these two lines gave the final facial measure. The maximum incisal opening was calculated from the mesioincisal angle of the maxillary central incisor to the mesioincisal angle of the ipsilateral mandibular central incisor [Table/Fig-4].
Image showing how to measure swelling.
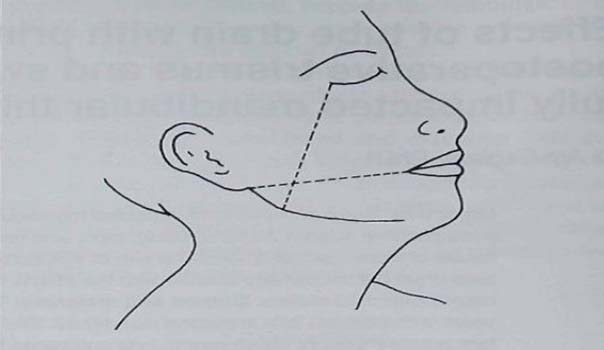
Image showing how to measure maximum inter-incisal opening.

Surgical Procedure: Routine blood and urine examination of patient were done pre-operatively. Before the procedure patient was asked to rinse the mouth with 0.2% chlorhexidine and normal saline in equal ratio (5%). Betadine was used for extra-oral painting and sterile drape was used for draping. Lignocaine (2%) with 1:2,00,000 adrenalin were used in all procedures.
Incision: Bard Parker blade no.15 was used for standard Terence ward’s incision (vertical incision made from gingiva just below the disto-buccal cusp of 2nd molar to mesiobuccal cusp of 2nd molar, incision line joined by gingival sulcular incision then was extended posterior laterally parallel to external oblique ridge 1 to 1.5cm then finishing the incision just mucosal). Mucoperiosteal flap was reflected, adequate bone removal was done using micromotor handpiece and bur, and tooth was delivered.
Preparation of Wound for Closure: Gentle sterile saline irrigation was done after tooth was delivered from socket. Wound toileting was done with removal of bone dust, granulation tissue, broken tooth fragments with cross-cut vulcanite bur. Sharp irregular bony margins were trimmed and smoothened. Wound was again irrigated with sterile saline and pressure packs given.
Closure of Surgical Wound: Before suturing, excess tissue was trimmed from the flap margins with scissor. Primary closure was accomplished using 3-0 silk suture in the control group. In second group (experimental group), tube drain was sutured by a circumferential suture tethered with the buccal flap through the releasing incision [Table/Fig-5]. The tube drain used in these cases was an infant feeding tube; size no. 6 (2.00mm lumen). The total duration (in minute) of surgery was noted.
Wound closure with tube drain.

Patients were advised antibiotics and analgesics for five days. The patients were also advised to avoid smoking, exertion and limit activity for at least rest of the day. The patients were recalled for follow-up on post-operative days 1, 3, 7 and 15. Sutures were removed on the seventh post-operative day. Post-surgical all measurements were done for pain, swelling and Maximum inter-incisal opening. Both surgical procedures (with and without tube drain) were done by single operator.
Statistical Analysis
The data were analyzed using the computer software SPSS statistics-16.0. Chi-square test was used to compare the frequency and t-test was used to compare the means to the level of significance was set at p≤0.05.
Results
The statistical analysis of pain showed statistically insignificant differences in the intensity between both groups. Although difference was noted between both groups on post-operative days 3 and 7, but the difference was statistically insignificant (p>0.05) and on post-operative day 15, assessments of pain were similar in both groups [Table/Fig-6]. Swelling data analysis showed that, on post-operative days 3 and 7, swelling value was much lesser in test group as compared to controls (p≤0.05) and similar in both groups on post-operative day 15 [Table/Fig-7,8]. MIIO in test group at post-operative day 1 was less as compared to control group and more at post-operative day 3 and 7. MIIO was reduced to normal on post-operative day 15 [Table/Fig-9,10]. But the differences between both the groups were not statistically significant (p>0.05). Mean operating time for suturing with tube drain was 39.48 minutes and for without tube drain was 38 minutes. Statistically there was no significant difference (p = 0.387) [Table/Fig-11].
The measurements of pain pre-operatively and on post-operative day 1,3,7 and 15 in both groups.
| VAS | Without tube drain | With tube drain | p-value |
|---|
| Preoperative Day | 0 | 96% | 60% | p>0.05 |
| 1 | 4% | 30% |
| 2 | 0% | 10% |
| 3 | 0% | 0% |
| Day 1 | 0 | 0% | 0% | p>0.05 |
| 1 | 52% | 52% |
| 2 | 46% | 46% |
| 3 | 2% | 2% |
| Day 3 | 0 | 0% | 0% | p>0.05 |
| 1 | 16% | 32% |
| 2 | 82% | 66% |
| 3 | 2% | 2% |
| Day 7 | 0 | 4% | 12% | p>0.05 |
| 1 | 72% | 72% |
| 2 | 24% | 16% |
| 3 | 0% | 0% |
| Day 15 | 0 | 98% | 98% | p>0.05 |
| 1 | 2% | 2% |
| 2 | 0% | 0% |
| 3 | 0% | 0% |
The measurements of swelling in the group with tube drain pre-operatively and post-operatively on days 1, 3, 7 and 15.
| Mean | N | Std. Deviation | p-value |
|---|
| Pair 1 | SWEL_PR | 102.90 | 30 | 5.370 | 0.000 |
| SWEL1 | 108.31 | 30 | 4.860 |
| Pair 2 | SWEL_PR | 102.90 | 30 | 5.370 | 0.000 |
| SWEL3 | 110.250 | 30 | 5.9420 |
| Pair 3 | SWEL_PR | 102.90(a) | 30 | 5.370 | - |
| SWEL7 | 102.90(a) | 30 | 5.370 |
| Pair 4 | SWEL_PR | 102.90(a) | 30 | 5.370 | - |
| SWEL15 | 102.90(a) | 30 | 5.370 |
Paired t-test;
Swel_pr- Swelling pre-operative
The measurements of swelling in the group without tube drain pre-operatively and post-operatively on days 1, 3, 7 and 15.
| Mean | N | Std. Deviation | p-value |
|---|
| Pair 1 | SWEL_PR | 102.90 | 30 | 5.370 | 0.000 |
| SWEL1 | 108.44 | 30 | 5.271 |
| Pair 2 | SWEL_PR | 102.90 | 30 | 5.370 | 0.000 |
| SWEL3 | 113.388 | 30 | 5.8039 |
| Pair 3 | SWEL_PR | 102.90 | 30 | 5.370 | 0.000 |
| SWEL7 | 108.00 | 30 | 5.834 |
| Pair 4 | SWEL_PR | 102.90(a) | 30 | 5.370 | - |
| SWEL15 | 102.90(a) | 30 | 5.370 |
Paired t test.
Swel_pr- Swelling preoperative
Maximum inter-incisal opening (MIIO) in the group with tube drain pre-operatively and post-operatively on days 1, 3, 7 and 15.
| Mean | N | Std. Deviation | p-value |
|---|
| Pair 1 | IIO_PR | 47.18 | 30 | 3.658 | 0.000 |
| IIO1 | 38.75 | 30 | 5.564 |
| Pair 2 | IIO_PR | 47.18 | 30 | 3.658 | 0.000 |
| IIO3 | 36.90 | 30 | 5.032 |
| Pair 3 | IIO_PR | 47.18 | 30 | 3.658 | 0.000 |
| IIO7 | 42.25 | 30 | 4.834 |
| Pair 4 | IIO_PR | 47.18(a) | 30 | 3.658 | - |
| IIO15 | 47.18(a) | 30 | 3.658 |
Paired t test;
IIO pr – Interincisal opening Pre-operative
Maximum inter-incisal opening (MIIO) in the group without tube drain pre-operatively and post-operatively on days 1, 3, 7 and 15.
| Mean | N | Std. Deviation | p-value |
|---|
| Pair 1 | IIO_PR | 47.18 | 30 | 3.658 | 0.000 |
| IIO1 | 39.53 | 30 | 4.857 |
| Pair 2 | IIO_PR | 47.18 | 30 | 3.658 | 0.000 |
| IIO3 | 35.03 | 30 | 4.282 |
| Pair 3 | IIO_PR | 47.18 | 30 | 3.658 | 0.000 |
| IIO7 | 40.23 | 30 | 4.828 |
| Pair 4 | IIO_PR | 47.18(a) | 30 | 3.658 | - |
| IIO15 | 47.18(a) | 30 | 3.658 |
Paired t test;
IIO pr – Interincisal opening Preoperative
Operative time (in minute) – comparison between groups.
| Group | N | Mean | Std. Deviation | t value | p value |
|---|
| With Tube Drain | 30 | 39.48 | 8.038 | 0.870 | 0.387 NS |
| Without Tube Drain | 30 | 38.00 | 7.100 |
Unpaired t-test
Discussion
Surgery of impacted third molars is one of the most frequent procedures in oral and maxillofacial surgery and can lead to immediate and post-operative discomfort [10,11]. Pain, swelling, and trismus are well known sequelae after third molar surgery and lead to a transitory functional alteration in the mastication function [15–17].
Pain in this study was evaluated using a Visual Analog Scale (VAS) of 10mm. The degrees of intensity were mild, moderate, and severe. There are various ways of measuring facial swelling as described in literature: facial bow [3], cephalostat [18], ultrasound [19], photographs [20] and measurement of craniometric points [21]. In this study we choose to measure the facial swelling using cranio-metric points in soft tissue with a flexible ruler, where the measures were recorded in centimeters and converted into relative values. Trismus was measured recording the pre-operative and post-operative maximum opening in centimeters [22,23]. Pain, swelling, and trismus are well known and lead to a transitory functional alteration in the mastication function [15,16].
Various modalities are considered in order to reduce post-operative sequelae. Medicinal modalities include administration of antibiotics like amoxicillin-clavulanic acid 2000mg/125 mg [5], Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), steroids [6] and enzymes and submucosal injections of dexamethasone and triamcinalone [7]. Other modalities include use of suture techniques that lead to a primary intention healing [16,17] or secondary closure [24] furthermore it is reported that the use of a drain in the surgery of impacted third molars improves the quality of life by reducing post-operative discomfort. Use of drain permits the drainage of the fluids located in the tissue spaces and could therefore be a technique recommended to minimize the post-operative sequelae [11].
The statistical analysis of pain showed statistically insignificant differences in the intensity between both groups. Although difference was noted between both groups on post-operative days 3 and 7, but the difference was statistically insignificant (p>0.05) and on post-operative day 15, assessments of pain were similar in both groups. These results are in agreement with the literature [25], which states that the pain is more severe in the immediate post-operative period and its reduction occurs progressively.
Swelling data analysis showed that, on post-operative days 3 and 7, swelling value was much lesser in test group as compared to controls (p≤0.05) and similar in both groups on post-operative day 15. Our results were in agreement with Cerqueira PR et al., [9] and Saglam AA [26] whereas Brabander EC and Cattaneo G [27] found no significant differences in swelling in both groups.
MIIO in test group at post-operative day 1 was less as compared to control group and more at post-operative day 3 and 7. MIIO was reduced to normal on post-operative day 15. But the differences between both the groups were not statistically significant (p>0.05). The results obtained were in agreement with those of Cerqueira PR et al., [9] and Saglam AA [26] according to them there was no statistically significant difference in trismus between two groups. Thus, the use of tube drain improves the quality of life.
Limitation
The limitations of putting tube drain are; the surgeon has to handle it carefully while putting tube drain, patient has to clean intra-orally after every meal otherwise there are chances of food lodgment around the tube drain.
Future Prospect
It is very useful procedure to reduce the swelling after surgical extraction of mandibular impacted tooth.
Conclusion
The tube drain group (experimental group) had significant reduction in post-operative swelling (facial oedema) as compared to control group on 3rd and 7th post-operative day. There were no differences in pain and IIO in both groups. Thus, the use of tube drain may be used to reduce post-operative swelling in mandibular third molar surgery. Further longitudinal studies with larger sample size should be carried out to affirm the outcomes of the study.
Paired t-test;
Swel_pr- Swelling pre-operative
Paired t test.
Swel_pr- Swelling preoperative
Paired t test;
IIO pr – Interincisal opening Pre-operative
Paired t test;
IIO pr – Interincisal opening Preoperative
Unpaired t-test