Simultaneous Transabdominal Hysterectomy and Cystolithotomy in an Augmented Urinary Bladder: Challenges and Outcome
Vijay Sharma1, Rakesh Kapoor2, Priyank Yadav3, Pankaj Gaur4, Deepa Kapoor5
1 Senior Resident, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raibareli Road, Lucknow, Uttar Pardesh, India.
2 Consultant, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raibareli Road, Lucknow, Uttar Pardesh, India.
3 Senior Resident, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raibareli Road, Lucknow, Uttar Pardesh, India.
4 Senior Resident, Department of Urology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raibareli Road, Lucknow, Uttar Pardesh, India.
5 Consultant, Department of Gynaecology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raibareli Road, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deepa Kapoor, Consultant, Department of Gynaecology, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raibareli Road, Lucknow-226014, Uttar Pradesh, india.
E-mail: dekapoor2002@yahoo.co.in
Augmentation cystoplasty is a procedure to increase the anatomical as well as functional capacity of the urinary bladder using a segment of bowel or ureter. Upto half of these patients develop complications but most of them are minor and managed easily. Urolithiasis, especially bladder calculi are seen in upto half of the cases and are removed endoscopically or by open approach. Hysterectomy is an uncommon procedure in patients with augmentation cystoplasty and is complicated by the altered anatomy of the pelvis. We describe a rare case of simultaneous abdominal hysterectomy and cystolithotomy in a patient with augmentation cystoplasty and discuss the relevant surgical anatomy.
Augmentation cystoplasty, Surgical anatomy, Vesical calculus
Case Report
A 64-year-old lady with no comorbidity presented to our OPD with history of ileal augmentation cystoplasty 20 years back for small capacity bladder secondary to vesicocutaneous fistula. The fistula had been formed following open repair of bladder injury sustained during dilation and curettage. After that she was on Clean Intermittent Catheterization (CIC).
She had complaint of high grade fever, intermittent haematuria, occasional vomiting and pyuria along with difficulty in catheterization for the last 1 month. There was past history of incisional hernia repair 12 years back for midline infraumbilical hernia.
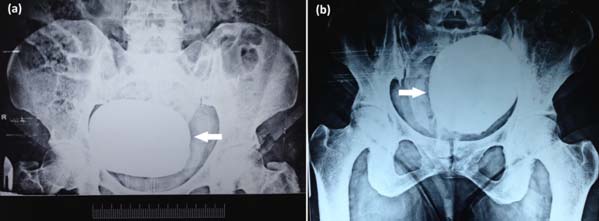
On examination an ill defined lump was seen arising from the pelvis extending 4 cm above symphysis pubis. There was complete uterine prolapse (procidentia). Ultrasonography revealed (12.5x10.3x10.1 cm) echogenic mass in the augmented bladder suggestive of vesical calculus. Urine microscopy showed 4-5 pus cells per high power field and urine culture was sterile. Urinary pH was 7.6. The abdominal and pelvic X-ray showed a large round radio-opaque shadow in pelvis [Table/Fig-1].
Preoperative abdominal and pelvis X-ray in: (a) erect and (b) supine position, showing the presence of a large radio-opaque shadow in the pelvis (arrow).
The patient underwent open cystolithotomy and total abdominal hysterectomy with bilateral salpingo-oophorectomy. Careful dissection was done to avoid injury to the pedicle of the augmented bladder. It was identified by mesenteric vessels which were going superiorly from the surface of the urinary bladder. In this case, ileum was used and the pedicle was found on the left side of the bladder. The left uterine pedicle was adhered to the ileal pedicle. It was identified by the ureter medially and ovary laterally. Careful dissection was done in this area for separation of the pedicle. The bladder was opened through the ileal patch avoiding injury to the mesenteric vessels. A large calculus (12.5x10.5x10.0 cm) weighing 745 grams was removed [Table/Fig-2].
(a) Intraoperative image after removal of the calculus from the augmented bladder (*). Clamp is placed at the medial end of the right fallopian tube (arrow); (b) Resected specimen showing uterus with fallopian tubes and the vesical calculus.
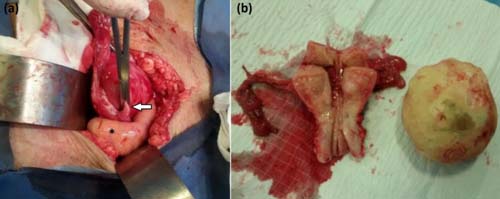
Chemical analysis of the calculus revealed calcium phosphate. Postoperative period was uneventful and patient was discharged in satisfactory condition. At 22 months of follow up, she was asymptomatic and continuing on CIC.
Discussion
Lemoine reported the first use of sigmoid colon to augment the urinary bladder in 1912. Goodwin et al., in 1959 described the use of ileum for the same purpose [1]. Augmentation cystoplasty is most commonly done for a poorly functioning neuropathic bladder although it may be done for any case where bladder volume or pressure is inappropriate to protect the upper urinary tracts. In the present case the patient had history of bladder injury during dilatation and curettage. She underwent bladder repair but developed a vesicocutaneous fistula. Following the repair of the fistula she was left with a small capacity bladder that led to severe urinary frequency, requiring an augmentation cystoplasty. The formation of vesical calculi is a common long term complication with reported prevalence as high as 52.5% [2]. It is thought to be secondary to mucus production, recurrent infection with urea splitting organisms [3], continent diversions [4] and metabolic derangements such as hypercalciuria, hypocitraturia, hyperoxaluria, hyperuricosuria, decreased urinary magnesium excretion and decreased urinary volume [2]. The treatment includes cystolithotomy or endoscopic cystolithotripsy. In the present case, owing to the size of the calculus, an open cystolithotomy was done.
Augmented bladder has some anatomical differences compared to the normal bladder. Entero-cystoplasty is fixed cranially by the mesentery, laterally by ureter and caudally by the trigone and urethra [5]. Augmentation is done at the intraperitoneal part of bladder (dome) and the cystotomy extends anteriorly upto the bladder neck [6]. During laparotomy for subsequent surgery, after incising the rectus sheath, it is not uncommon to find ileal loops adhered to the peritoneum just underneath the rectus sheath. After mobilization of the ileum and exposure of the urinary bladder, access to the posterior wall of the urinary bladder is also difficult as the mesentery of the augmentation patch fans out from the dome of the bladder to the posterior abdominal wall which means that mobilization must begin lateral to the bladder. Surgical manipulation has to be done carefully as the structures tethering the entero-cystoplasty are at risk of injury. In the initial months, the vascularisation of the ileal patch is only from the mesentery with no contribution from the urinary bladder so the division of the mesenteric pedicle may lead to devascularisation of the patch. A basic requisite for pelvic surgery in an augmented bladder therefore, is a deep understanding of the anatomy of the pelvis and the changes after augmentation cystoplasty [7].
A key factor in performing hysterectomy in a patient with augmented bladder is the identification of uterine pedicles. After the pelvic dissection that occurs during augmentation cystoplasty, adhesions cause distortion of the uterine pedicles and they can be located more anteriorly than otherwise. Likewise, special care must be taken during dissection near the cervix in patients who have also undergone bladder neck reconstruction or artificial urinary sphincter as they are particularly at risk of damage to the continence mechanism [8].
Bladder neck reconstruction at the time of augmentation cystoplasty has also been identified as a factor increasing the complexity of surgery as well as increasing the hazard of future procedures in paediatric population [9]. Although the use of augmentation cystoplasty in overactive bladder is declining, poor capacity bladder still forms an indication for augmentation and a fraction of these patients would be re-operated for urological and non-urological reasons, underlining the importance of a knowledge of the pelvis anatomy in such patients [10].
Conclusion
Patients with augmented bladder with indications for hysterectomy can be candidates for abdominal hysterectomy especially when indications for open bladder surgery are also present. The operating surgeon must be well versed with the pelvic anatomy. The dissection must be meticulous and should be preferably done in the presence of urologist who is familiar with anatomy of the augmented bladder. The previous operative notes of the augmentation cystoplasty are desirable.
[1]. Goodwin WE, Winter CC, Barker WF, “Cup-patch” technique of Ileocystoplasty for bladder enlargement or partial substitutionSurg Gyencol Obstet 1959 108:240-44. [Google Scholar]
[2]. Kisku S, Sen S, Karl S, Mathai J, Thomas RJ, Barla R, Bladder calculi in the augmented bladder: A follow-up study of 160 children and adolescentsJ Paediatr Urol 2015 11(2):66.e1-6. [Google Scholar]
[3]. Mathoera RB, Kok DJ, Nijman RJ, Bladder calculi in augmentation cystoplasty in childrenUrology 2000 56(3):482-87. [Google Scholar]
[4]. Shekarriz B, Upadhyay J, Demirbilek S, Barthold JS, Gonzalez R, Surgical complications of bladder augmentation: comparison between various enterocystoplasties in 133 patientsUrology 2000 55(1):123-28. [Google Scholar]
[5]. Hautmann RE, Volkmer BG, Pregnancy and urinary diversionUrol Clin N Am 2007 34:71-88. [Google Scholar]
[6]. Rackley R, Abdelmalak J, Ross J, In AC Novick, JC Jones, Operative Urology at the Cleveland Clinic 2006 1st edTotowa, NJHumana Press Inc:265 [Google Scholar]
[7]. Cameron A, Cespedes R, Mcguire E, Bladder Augmentation. In S. Graham Jr. & T. KeaneGlenn’s Urologic Surgery 2010 7th edPhiladelphiaLippincott Williams & Wilkins:124 [Google Scholar]
[8]. Kapoor D, Chipde SS, Agrawal S, Chipde S, Kapoor R, Delivery after augmentation cystoplasty: Implications and precautionsJ Nat Sci Biol Med 2014 5(1):206-09. [Google Scholar]
[9]. Schlomer BJ, Copp HL, Cumulative incidence of outcomes and urologic procedures after augmentation cystoplastyJ Paediatr Urol 2014 10(6):1043-50. [Google Scholar]
[10]. Biers SM, Venn SN, Greenwell TJ, The past, present and future of augmentation cystoplastyBJU Int 2012 109(9):1280-93. [Google Scholar]