Percutaneous Nephrolithotomy (PCNL) is the most frequently performed surgical procedure for complex upper renal tract calculi. Although the skin incision for PCNL appears small, the intensity of intraoperative and postoperative pain is significant owing to soft tissue injury [1,2]. Most of these patients have compromised renal function. A technique which reduces the requirement of intraoperative anaesthetic and analgesic drugs and provides excellent postoperative analgesia is desirable as NSAIDs are relatively contraindicated.
Paravertebral Block (PVB) is a simple and effective technique for unilateral procedures with minimal incidence of hypotension and urinary retention [3]. Bupivacaine is the most commonly used local anaesthetic drug in PVB. Clonidine, an α2 agonist has been effectively used in various regional blocks in adult as well as paediatric patients [4,5] including PVB [6,7]. It was hypothesized that PVB could reduce the pain associated with PCNL and thus improve patient comfort and patient outcome. The present study was conducted to compare the efficacy of Bupivacaine (0.5%) alone or Bupivacaine (0.5%) with Clonidine (1ug/kg) versus control in a single level PVB for intra-operative and post-operative analgesia in patients undergoing PCNL procedure.
Materials and Methods
This randomized, prospective, observer blind study was carried out over a period from January 2013 to July 2015 after obtaining approval from hospital ethics committee and written, informed consent from the participants.
A pilot study was conducted in 18 patients to test the hypothesis. Sample size was calculated from this pilot study of 18 patients on the basis of anticipated difference in the duration of analgesia between the Control group (Group C) and PVB with Bupivacaine group (Group A). During the pilot study the duration of postoperative analgesia was 7.47±2.26 hours in Group A and 5.01±1.16 hours in Group C. Assuming Type I error of 5% and Type II error of 20% (power of study 80%) with allowable difference (Difference of mean for duration of post-operative analgesia between control group and Bupivacaine group) of 2.46 hours and population variance of 11.69, the sample size calculated for each group was 30. The Mean and Standard deviation data was obtained from the pilot study and the following formula was used for sample size calculation {n1=n=n3= 2(Zα/2±Zβ)2 σ2 / (μ2-μ1)2}, where σ2 is population variance, μ2-μ1 is allowable difference between means of both groups, Zα/2 is 1.96 and Zβ is 0.84.
The study included ASA Class I and II patients of both sexes, between 18 to 60 years of age and weighing 40 to 80 kg undergoing PCNL procedure. The study excluded patients with controlled and uncontrolled hypertension, coagulopathy, any contraindication to regional block, cerebrovascular accidents, raised ICT, space occupying lesion and patients who refused to give consent.
All patients underwent thorough medical evaluation and investigations. Intraoperative monitoring included Cardioscope, NIBP monitor, Pulse oximeter, ETCO2 monitor and temperature monitor. In the operating room, patients were administered oxygen by nasal prongs. IV access was established with 18G angiocath on the dorsum of hand and Ringer’s lactate infusion was started at 10ml/kg/hr.
With patient in sitting position and under proper aseptic precautions, paravertebral block was performed in Group A and B. After negative aspiration for blood, appropriate drug was injected. Patient was then turned in the supine position.
Group A received 0.5% Bupivacaine in PVB, Group B received 0.5% Bupivacaine±1μg/kg of Clonidine in PVB while Group C did not receive PVB. Maximum dose of Bupivacaine was not more than 2mg/kg. The total drug volume was 15ml in patients weighing less than 60kg and 18ml in patients weighing more than 60kg.
All patients were preoxygenated with 100% Oxygen and pre-medicated with IV Glycopyrrolate (0.004mg/kg), I.V Ranitidine (1mg/kg) and IV Ondansetron (0.008mg/kg).
Anaesthesia induction was with I.V Fentanyl (2μg/kg), I.V Midazolam (0.03 mg/kg), I.V Thiopentone Na (5-7 mg/kg) and muscle relaxation with I.V Atracurium (0.5 mg/kg). Intubation was done with appropriate size cuffed endotracheal tube. Ryle’s tube was inserted. Throat was packed. Eyes and pressure points were well padded. A cystoscopic ureteric catheter was passed by the surgeon in lithotomy position and then patients were turned prone on bolsters.
Anaesthesia was maintained with O2±N2O (50:50)±I.V infusion of propofol (10→8→6→4-5mg/kg/hr) to maintain haemodynamic parameters within 20% of baseline value±intermittent I.V Atracurium (0.1mg/kg).
At the end of the surgery, neuro-muscular blockade was reversed with I.V Glycopyrrolate (0.008mg/kg) +I.V Neostigmine (0.05mg/kg). Group C patients received IV Paracetamol (10mg/kg) 20 minutes prior to reversal for postoperative analgesia.
An observer who was not part of study made all intraoperative and postoperative observations in operating room and post anaesthesia care unit. The observer entered the operating room after the patient was given in supine position before induction of anaesthesia and left the operating room once the drain was inserted by the surgeon (around 20 minutes before extubation) till reversal of anaesthesia. Thus, this observer was blind to the group allocation of patients.
Intraoperative analgesia was assessed by stability of haemodynamic parameters. Heart Rate (HR), Systolic Blood Pressure (SBP)/Diastolic Blood Pressure (DBP), SPO2 and ETCO2 were monitored every 5 minutes for first half hour, every 10 minutes for next half hour and every 15 minutes till the end of surgery. A ‘0’ minute was taken as the reading taken after making the patient supine following the performance of block. Heart rate of < 60 beats/min was defined as bradycardia and was treated with IV Atropine (0.01mg/kg). Blood pressure < 30% of the baseline value was defined as hypotension and treated with IV fluid bolus and /or Ephedrine 6mg bolus IV.
Post-operative analgesia was assessed by monitoring of Visual Analog Score (VAS) at regular interval till rescue analgesia was given. Rescue analgesia was given with I.V Tramadol (1mg/kg) at the VAS of >4. Time to 1st rescue analgesia and duration of analgesia was noted. Ramsay sedation score was monitored for 24hours.
Results
A total of 90 patients were included in this prospective, randomized, observer blind study with 30 patients in each group. The groups were comparable with regard to age, weight, sex, ASA grade, baseline haemodynamic parameters and duration of surgery [Table/Fig-1].
Comparison of demographic data and baseline parameters.
| Variables | Groups | Male | Female | p-value |
|---|
| Sex | A | 20 | 10 | 0.721Not Significant |
| B | 17 | 13 |
| C | 18 | 12 |
| Variables | Groups | Mean | Standard Deviation | p-value |
| Age (Years) | A | 44.07 | 9.85 | 0.220Not Significant |
| B | 40.17 | 11.93 |
| C | 38.70 | 11.89 |
| Weight (Kgs) | A | 64.40 | 7.06 | 0.407 Not Significant |
| B | 62.87 | 5.46 |
| C | 62.23 | 5.39 |
| ASA Grade | A | 1.23 | 0.43 | 0.490 Not Significant |
| B | 1.13 | 0.35 |
| C | 1.13 | 0.35 |
| Duration of Surgery (Hours) | A | 1.63 | 0.58 | 0.082 Not Significant |
| B | 1.62 | 0.54 |
| C | 1.78 | 0.22 |
| PreoperativePulse Rate(Beats/minute) | A | 80 | 9.66 | 0.082Not Significant |
| B | 78.33 | 6.39 |
| C | 78.20 | 5.02 |
| Preoperative Systolic BP(mm of Hg) | A | 119.33 | 6.914 | 0.866Not Significant |
| B | 119.33 | 12.576 |
| C | 118.33 | 5.306 |
| Preoperative Diastolic BP(mm of Hg) | A | 74 | 7.98 | 0.914Not Significant |
| B | 74.33 | 5.02 |
| C | 74.33 | 6.79 |
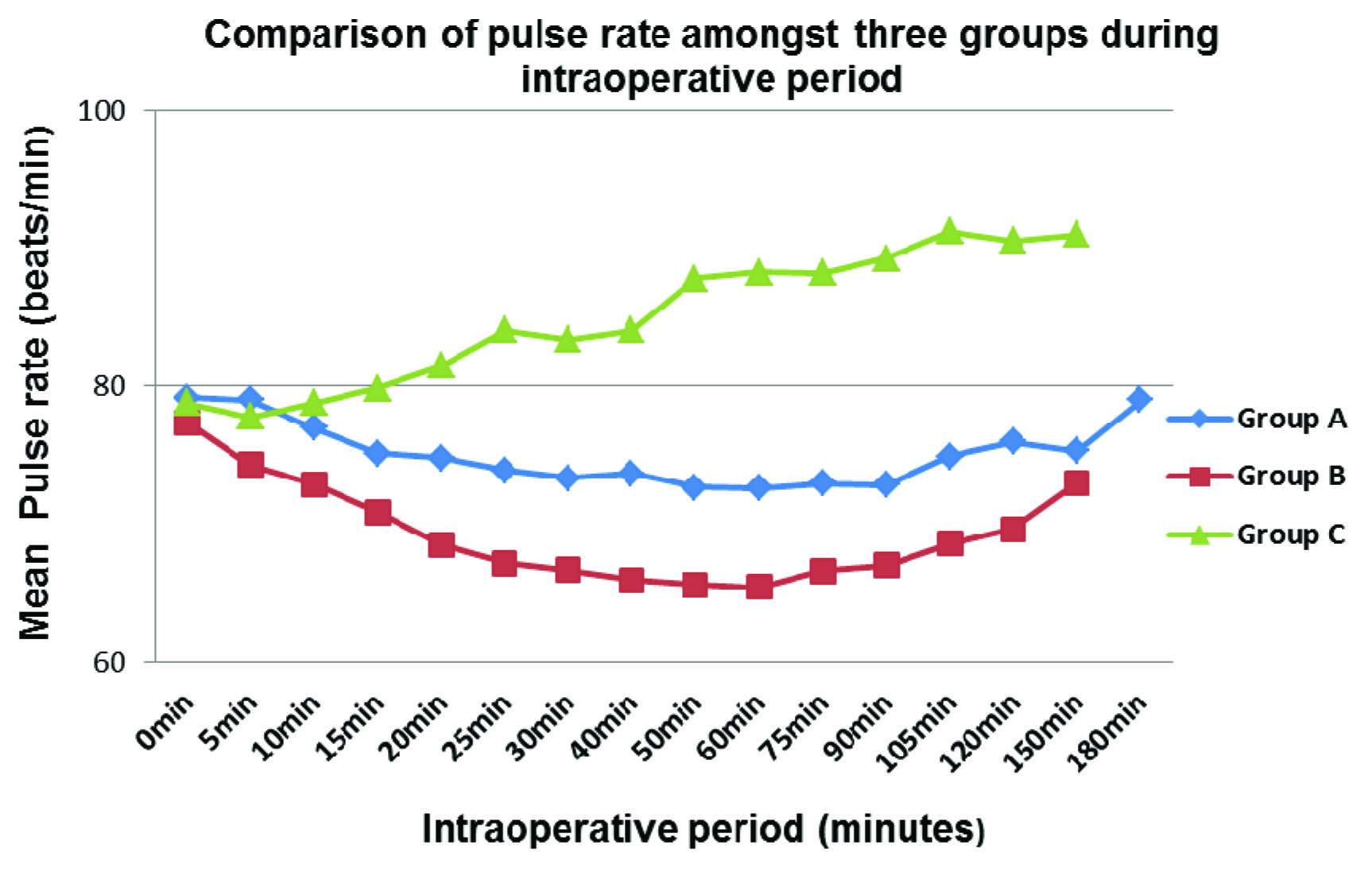
The mean intraoperative Pulse Rate (PR) was statistically lower in Group A (PVB with Bupivacaine only) and B (PVB with Bupivacaine±Clonidine) as compared to the mean intraoperative pulse rate in patients from Group C (Control group) from 10 minutes post block to upto 120 minutes. The mean intraoperative PR in Group B was statistically lower than in Group A between 15 minutes to 50 minutes post block while comparable during the rest of the surgery [Table/Fig-2].
Intraoperative pulse rate.
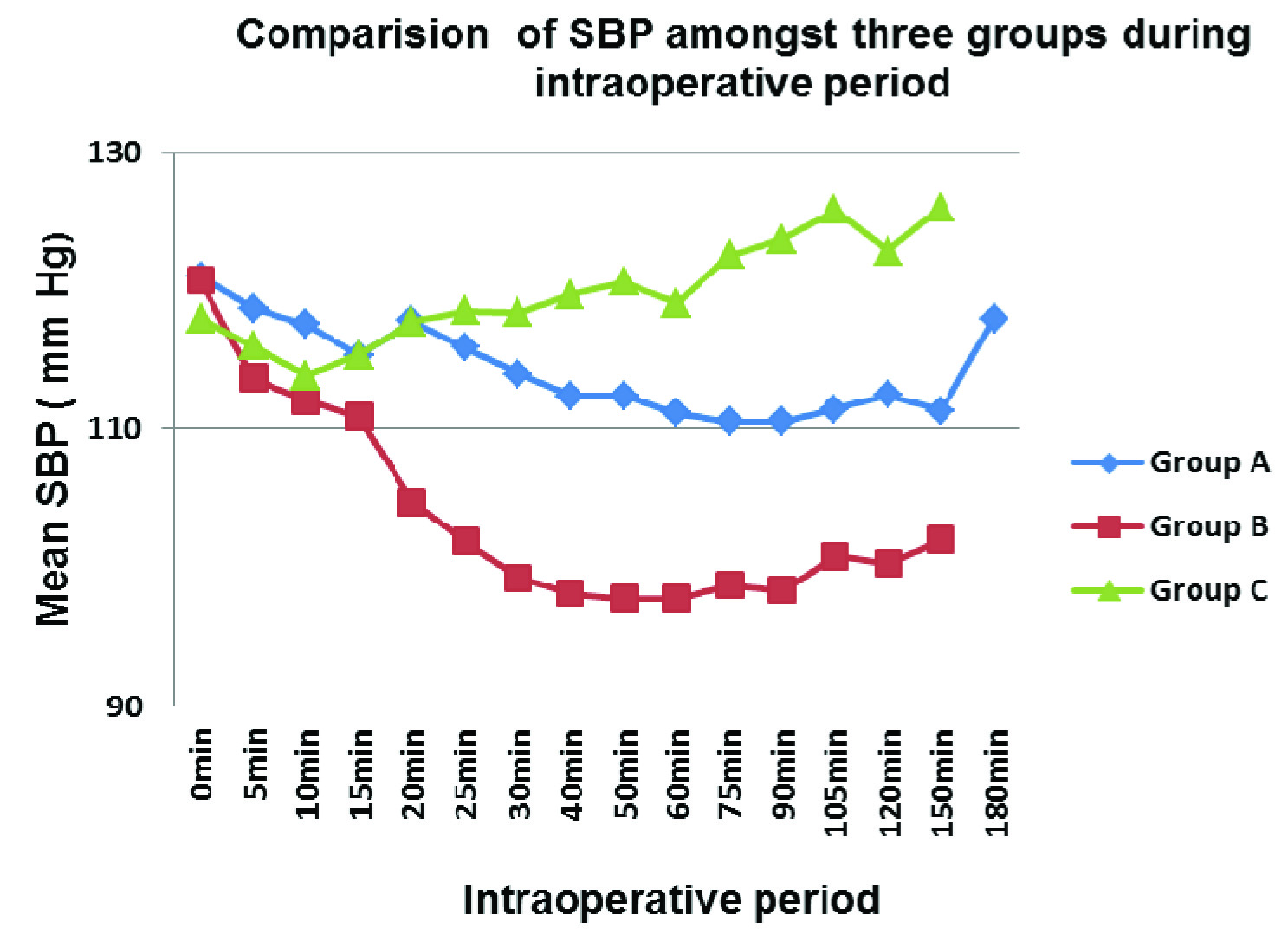
The mean intraoperative Systolic Blood Pressure (SBP) in Group B was statistically lower than the mean intraoperative SBP observed in Group A and Group C from 20 minutes to 60 minutes post block. During the intraoperative period of 60 minutes to 120 minutes the mean intraoperative SBP was statistically lower in Group A and Group B than in Group C [Table/Fig-3].
Intraoperative systolic blood pressure.
The mean intraoperative Diastolic Blood Pressure (DBP) in Group B was statistically lower than the mean intraoperative DBP observed in Group A and Group C from 10 minutes till 120 minutes post block. There was no incidence of bradycardia or hypotension.
Thus, patients with PVB maintained stable intraoperative haemodynamics and this can be attributed to effective analgesia and anaesthesia in the surgical area without significant sympathetic blockade.
The mean total amount of propofol required to maintain the haemodynamic parameters within 20% of the baseline preoperative value was 15.17±3.43ml in Group B, 29.33±12.6ml in Group A and 64.5±6.07ml in Group C. This difference was statistically significant. The requirement of propofol was statistically higher in Group C as compared to Group A and Group B [Table/Fig-4].
Intra-operative propofol requirement, mean propofol dose, duration of analgesia.
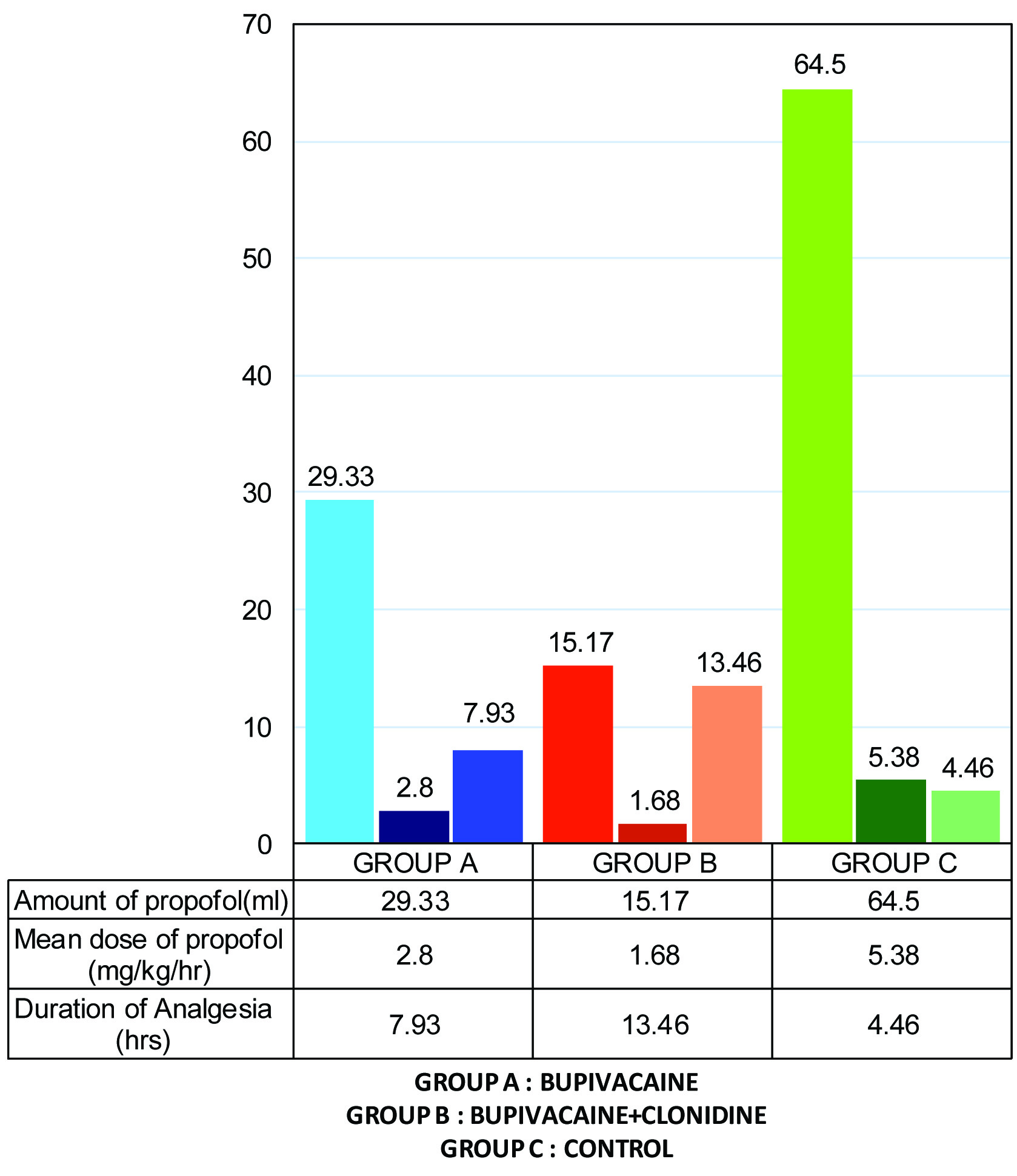
The mean dose of Propofol was 5.38±1.11mg/kg/hr in Group C, which was significantly higher than dose required in Group A and Group B which was 2.81±0.69mg/kg/hr and 1.68±0.46mg/kg/hr respectively [Table/Fig-4].
This shows that PVB reduced the requirement of Propofol and addition of Clonidine reduced it further.
The duration of postoperative analgesia was taken from the time of extubation to the time of administration of rescue analgesia. The mean of duration of analgesia in Group A was 7.93±1.44 hours, in Group B 13.46±1.38 hours and in Group C 4.46±0.86 hours [Table/Fig-4]. The mean duration of analgesia in Group B was almost double the duration of analgesia in group A and three times the duration in control group. This difference was statistically significant.
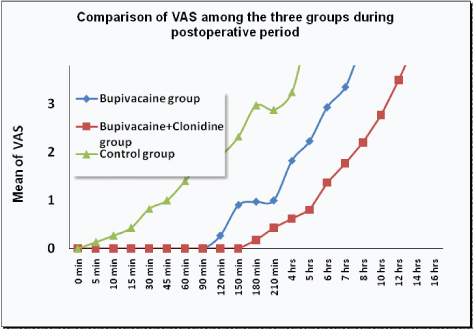
The mean VAS score was ‘0’ for a period of 150 minutes in Group B and remained <1 till five hours. The mean of VAS Score was ‘0’ for a period of 90 minutes in Group A and remained <1 till 3½ hours. In group C the VAS score remained <1 only for 45 minutes [Table/Fig-5]. The mean VAS score in group B was lower than the mean VAS score in Group A and C at all times during the postoperative period while the mean VAS score in group A was lower than the mean VAS score in Group C at all times during the postoperative period. This difference was statistically significant. Thus patients in Group A and B had excellent postoperative analgesia. The Ramsay Sedation Score (RSS) was statistically comparable in all groups and no patient from any group had excessive sedation or respiratory depression. We monitored the patients for complications such as nausea, vomiting, bradycardia, hypotension, respiratory depression, urinary retention, sweating, pruritis and hallucinations. In our study we did not observe any incidence of these complications in any of our patients.
Discussion
PCNL is the most frequently performed surgical procedure for renal calculi. Although the skin incision for PCNL is small, the intensity of intraoperative and postoperative pain is quite significant. Since most of these patients have compromised renal function, a technique which will reduce the requirement of intraoperative anaesthetic and analgesic drugs along with provision of excellent postoperative analgesia is desirable as systemic analgesics are relatively contraindicated. Regional anaesthesia provides both intraoperative and postoperative analgesia and is without side effects of systemic analgesics. Spinal, epidural and paravertebral blocks have been used for PCNL [8-10]. Since PCNL is unilateral procedure, a regional technique that blocks pain sensations from kidney and surgical site is preferable.
With this as background, we selected PVB for intra-operative and postoperative analgesia in patients undergoing PCNL procedure. PVB is a simple, safe and effective technique for unilateral procedures with minimal incidence of hypotension, urinary retention, and postoperative nausea vomiting [3].
The present study included 90 ASA Class I & II patients randomly divided into three groups of 30 patients each. Group A received PVB with Bupivacaine (0.5%) only, Group B received PVB with Bupivacaine (0.5%) plus Clonidine (1μg/kg) and Group C was control group.
Maximum dose of Bupivacaine was not more than 2mg/kg. Clonidine 1μg/kg [4,11] is effective for intra and postoperative analgesia without bradycardia and hypotension, so this dose was chosen for PVB. The total volume of drug in PVB was decided from literature review as 0.3ml/kg [4,6] and the maximum volume was fixed at 15ml for patients weighing less than 60kg and 18ml for more than 60kg.
All PVB were performed at T11-T12 level. The sensory input from the kidney travels to the T10-T11 level of spinal cord and is sensed in the corresponding dermatome. Thus, the kidney pain is referred to the T10 and T11 dermatome. In PCNL, a nephrostomy track is created between T10- L2 levels. Therefore for adequate pain relief, PVB should block T10 to L2 dermatomes. The factors affecting spread of Bupivacaine in the thoracic paravertebral space have been studied by Cheema and colleagues [12]. They found mean sensory level to spread 2.2 segments above and 1.4 segments below the level of injection. This is sufficient to block pain sensation of PCNL surgery if a block is performed at T11-T12 level.
The period between PVB and skin incision was about 20 minutes in all patients. In studies conducted by Weltz CR et al., and by Mandal MC et al., the PVB had an onset time of 17.2 minutes and 15 minutes respectively [13,14]. Thus in our study, sufficient time interval was present for onset of block action. We defined ‘failed block’ as presence of sympathetic response to skin incision (i.e., the haemodynamic parameters just after the skin incision were > 20% of the haemodynamic parameters noted before the skin incision). The treatment was additional doses of IV Propofol.
The mean intraoperative pulse rate was statistically higher in control group (Group C) as compared to the mean intraoperative PR in Group A and B from 10 minutes post block to upto 120 minutes [Table/Fig-2]. This can be attributed to PVB providing effective intraoperative analgesia in Group A and B.
The mean intraoperative PR in Group B was statistically lower than in Group A for the time interval between 15 minutes to 50 minutes due to Clonidine.
The mean intraoperative SBP in the Group B was statistically lower than the mean intraoperative SBP observed in Group A and Group C from 20 minutes to 60 minutes post block.
During the rest of the intraoperative period (60 to 120 minutes) the mean intraoperative SBP in Group A and Group B was statistically lower than in Group C and the mean intraoperative SBP in Group B was statistically lower than in Group A.
The mean intraoperative Diastolic Blood Pressure (DBP) in Group B group was statistically lower than the mean intraoperative DBP observed in Group A and Group C from 10 minutes till 120 minutes post block .
The mean intraoperative DBP in Group A was comparable to the mean intraoperative DBP of Group C for first 20 minutes. After 20 minutes the mean intraoperative DBP in Group A was statistically lower than the mean intraoperative DBP noted in Group C [Table/Fig-3].
Thus PVB with Bupivacaine as well as Bupivacaine±clonidine was effective in providing stable intraoperative haemodynamic profile. It was also effective in providing excellent surgical anaesthesia and analgesia. There was no incidence of bradycardia or hypotension.
Elbealy E et al., compared Epidural Anaesthesia, Lumbar PVB and General Anaesthesia for PCNL in 57 patients and concluded that lumbar PVB with 0.5%. Bupivacaine was associated with more significant intraoperative haemodynamic stability compared to epidural anaesthesia and general anaesthesia in patients undergoing PCNL [15]. In our study too, significant intraoperative haemodynamic stability was observed in patients from Group A and B who received 0.5% Bupivacaine in paravertebral block with or without Clonidine.
The mean total Propofol required to maintain the haemodynamic parameters within 20% of the baseline preoperative value was 15.17±3.43 ml in Group B, 29.33±12.6ml in Group A and 64.5±6.07 ml in Group C. This difference was statistically significant.
The mean dose of Propofol was 5.38±1.11 mg/kg/hour in Group C, which was significantly higher than in Group A and Group B which was 2.81±0.69mg/kg/hour and 1.68±0.46mg/kg/hour respectively. This difference was statistically significant.
This shows that PVB reduced the requirement of Propofol by providing effective surgical anaesthesia and analgesia in Group A and Group B patients. Addition of Clonidine reduced the propofol requirement further due to its analgesic effects.
Klein SM et al., compared thoracic PVB plus general anaesthesia to general anaesthesia alone in a single-blinded [16], prospective, randomized study of 60 women for unilateral or bilateral breast augmentation or reconstruction. Patients were assigned (n = 30/group) to receive a standardized General Anaesthetic (GA) with or without Thoracic Paravertebral Block (TPVB). They concluded that, TPVB Group required less amount of propofol compared to GA groups with improved postoperative analgesia from PVB at 30 minutes (p = 0.0005), 1 hour (p= 0.0001), and 24 hours (p = 0.04) and may last as long as 72 hours, when compared with GA alone [16].
We have found similar results in that the requirement of propofol was significantly reduced in patients from group A and B who received PVB and these patients also had prolonged postoperative pain relief.
Borle AP et al., evaluated the efficacy of bupivacaine administered in PVB for perioperative pain relief after percutaneous nephrolithotomy (PCNL) [10]. This was an observer blinded randomized controlled study in 50 ASA Grade I and II adults, aged 18 to 65years, undergoing PCNL under general anaesthesia. PVB group patients received preinduction 20mL of 0.5% bupivacaine in the T9-10 paravertebral space and a catheter in addition to general anaesthesia. Control group patients received only general anaesthesia. They found that intraoperative fentanyl requirement was higher in the control group (2.74±0.75 μg/kg {95% confidence interval (CI) 2.42, 3.05}) than the PVB group (2.07±0.26 μg/kg {95 % CI 1.96, 2.18}), (p=0.0001). In our study too, the intraoperative requirement of the anaesthetic agent Propofol was significantly decreased in patients of paravertebral block groups [10].
The duration of postoperative analgesia was taken from the time of extubation to the time of administration of rescue analgesia. The mean of duration of analgesia in Group A was 7.93±1.44 hours, Group B 13.46±1.38 hours and of Group C 4.46±0.86 hours during postoperative period. Thus, the mean duration of analgesia in Group B was almost double the duration of analgesia observed in group A and three times the duration of analgesia obseved in control group.
Kairaluoma PM et al., conducted a study in 60 patients to assess the effect of Bupivacaine in PVB on opioid consumption in post anaesthesia care unit [17]. Patients were randomly given single-injection PVB at T3 level with Bupivacaine 0.5% (1.5 mg/kg) or saline before general anaesthesia. The result showed that in patients with TPVB with Bupivacaine, the IV opioid medication requirement (primary outcome variable) was 40% less than the control patients. They also had a longer latency to the first opioid dose as well as less pain at rest after 24 hour (p < 0.01) [17].
Our study results are similar in that we observed longer latency for the first dose of tramadol in groups who received PVB.
Dabbagh A et al., studied the effect of TPVB for postoperative pain relief following breast surgery [18]. Thirty patients were given TPVB (study) and were compared with 30 patients who received general anaesthesia (control). The study recommended PVB as a suitable alternative to general anaesthesia in selected breast surgical patients for postoperative pain reduction [18].
In the study conducted by Borle AP et al., time to first postoperative analgesic requirement was longer in the PVB group (120 min {30-570}) than the control group (30 min {0-180}), (p=0.0000) [10]. Our results are similar to this study.
Thus PVB can be used as an effective alternative method for providing intraoperative and postoperative analgesia for select unilateral surgeries in thoracolumbar region.
The mean VAS score was ‘0’ for a period of 150 minutes in Group B and remained < 1 till five hours. The mean of VAS score in group B was lower than the mean of VAS score in Group A and C at all times during the postoperative period. The mean of VAS Score was ‘0’ for a period of 90 minutes in Group A and remained < ‘1’ till 3 ½ hours. The VAS score in group A was lower than the VAS score in Group C at all times during the postoperative period. In group C the VAS score remained less than ‘1’ only for 45 minutes.
The difference in the mean VAS score between Group A and Group B was not significant for up to 120 minutes; however the VAS scores in these two groups A and B were significantly lower compared to Group C. This difference was statistically significant.
In the study by Borle AP et al., VAS on rest (0, 1, 2, and 12 h) and movement (all time points) were significantly lower in the PVB group which is similar to results of our study [10].
The effect of Clonidine has been studied as an adjuvant to Bupivacaine in various regional blocks [8,19,20]. These studies conclusively show that Clonidine significantly enhances the quality of regional block by a faster onset and prolonged duration of sensory and motor block as well as enhancing postoperative analgesia. These benefits are not associated with any haemodynamic complications, sedation or other adverse effects and hence Clonidine added to Bupivacaine is an attractive option for improving the quality and duration of regional block.
Although we did not get any reference of Clonidine used in single level PVB, we found results similar to all the above mentioned studies.
Thus PVB provided more effective and prolonged analgesia and addition of Clonidine significantly prolonged and improved the analgesia as assessed by VAS Score.
Limitation
The limitation of this study is the small sample size. A larger prospective randomized trial will help establish further conclusive evidence and determine the cost effectiveness of this technique.
Conclusion
The study results show PVB to be an effective method for providing intra and postoperative analgesia for PCNL surgery. It reduced the requirement of intraoperative Propofol, maintained stable intra and postoperative haemodynamics without any adverse effects or complications. Addition of Clonidine as an adjuvant to Bupivacaine enhanced the quality of PVB and provided much better haemodynamic stability, further reduced the dose of intraoperative propofol and provided significantly longer post-operative analgesia without any incident of bradycardia, hypotension, sedation or respiratory compromise. Thus PVB may be considered as a valuable technique in patients posted for PCNL especially in patients with compromised renal function.