The marginal fit is of paramount importance for long term success of All ceramic restorations. Discrepancy in marginal fit facilitates, salivary infiltration and microleakage resulting in dissolution of the luting cement; thus, increasing the susceptibility to caries, eventually leading to pulpal damage. Marginal discrepancy also inflicts severe sensitivity due to the exposure of dentinal tubules and favours collection of plaque and food debris around the exposed margins which subsequently initiates periodontal breakdown in abutment teeth [1–3].
Marginal fit can be influenced by several factors like the type of finish lines, thickness of the die spacers, preference of restorative materials, processing techniques for fabrication and the choice of luting agents. Amongst the processing techniques, CAD/CAM technique is becoming increasingly popular due to it’s several advantages over the conventional ceramic processing techniques. This technique offers a great advantage over conventional processing techniques by eliminating clinical steps in impression making and laboratory steps including cast pouring, articulation, die sectioning, casting and subsequent layering thus conserving time and manpower, but the superiority of this system over the conventional ones with effect to marginal discrepancy is not clearly established in the literature [4].
Luting agents occupy the interface between the prepared teeth and the restoration and minimizes the marginal gap to a greater extent. The commonly used luting agents for All ceramic restoration mainly are resin modified glass ionomer and resin cements [1]. Kelly JR et al., and Tan PL et al., have reported that the fracture strength of All ceramic restoration can be improved by using a resin cement and resin cements should be preferred choice for cementing All ceramic restorations [2,3].
Resin cement offer improved properties and is less technique sensitivity than traditional cements [5] when used for cementation of ceramic and metal based restorations. Despite varying reports of marginal discrepancy with luting agents the precise effect of resin bonded luting agents influencing marginal discrepancy in All ceramic complete veneer crowns needs to be investigated further. Hence, this study was carried out to accomplish the above mentioned purpose.
The aim of the study was to estimate and compare the marginal discrepancy in CAD/CAM All ceramic complete veneer crowns prior and following luting with resin bonded luting agents.
Materials and Methods
Extracted human maxillary first premolars satisfying the following criteria were selected for this experimental, in-vitro study. The teeth included in the study were extracted due to orthodontic, orthognathic surgical purposes, aggressive periodontitis, juvenile periodontitis, fenestrations and dehiscence. The teeth excluded from the study were carious, non-vital, attrited, abraded, eroded, endodontically treated, partially fractured and already prepared teeth.
The selected teeth were stored in 10% formalin solution and cleaned thoroughly of all deposits and soft tissue debris with a bristle brush and non-fluoridated pumice paste. Cellophane dies measuring 10x10mm were prepared and lubricated with petroleum jelly and a smooth powder of Type II gypsum was mixed in a vibrator and poured into the moulds.
The specimen teeth were embedded upright with long axis parallel to the height of the cellophane mould with Cemento-Enamel Junction (CEJ) placed 2mm above the plaster. After the plaster was set the cellophane brackets were removed and plaster blocks were finished and polished. The blocks were randomly allocated into four groups of 5 specimens each to receive All ceramic complete veneer crowns to be luted with resin cements and a pilot study was initiated to study marginal discrepancy. Based on the results of pilot study the sample size was estimated to 27 specimens each for the four experimental groups to establish 90% statistical power.
Group I: All ceramic complete veneer retainers luted with resin modified GIC. (RelyX Luting Plus Cement, 3M ESPE Zhengzhou Smile Industrial Co., Ltd., China).
Group II: All ceramic complete veneer retainers luted with Bis-GMA based dual cure resin cement variolink (Variolink II Aesthetic Resin Cement, Ivoclar Vivadent, United States).
Group III: All ceramic complete veneer retainers luted with PMMA based resin cement superbond (Superbond C&B, Sun Medical, Japan).
Group IV: All ceramic complete veneer retainers luted with urethane dimethacrylate resin cement (Calibra esthetic resin cement, Dentsply, Milford, United States).
Measurement of Marginal Adaptation before Cementation:
The teeth were prepared by a single operator to receive All ceramic restorations. A uniform 2mm reduction was done on all the five surfaces and shoulder finish line was placed 1mm above the CEJ with medium grit diamond with a convergence angle of 8-10° verified with a digital surveyor, scanned and All ceramic restoration were milled in CEREC 3 CAD/CAM unit.
The ceramic block used for the present study was PROCAD (Ivoclar Vivadent, Schaar, Lichtenstein) and dimensions are 62X25mm. Cerec spray was used to coat the surface of the prepared tooth surface to receive the All ceramic restoration. The four axis milling device with three spatial axis was used in the study. The sectioned specimen was luted with the resin luting agents according to the manufactures instructions and thermocycled at 5o and 55o at 2500 cycles. Then they were sectioned and seated with the help of the acrylic resin jig fabricated to stabilize the crown and firm pressure was applied till the cement was set.
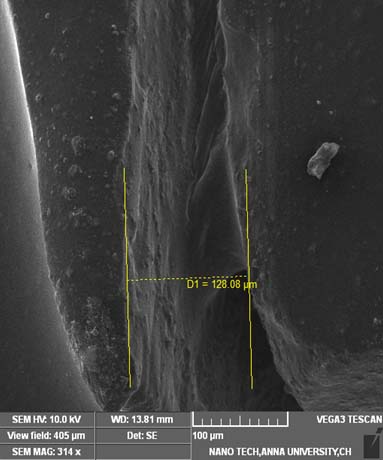
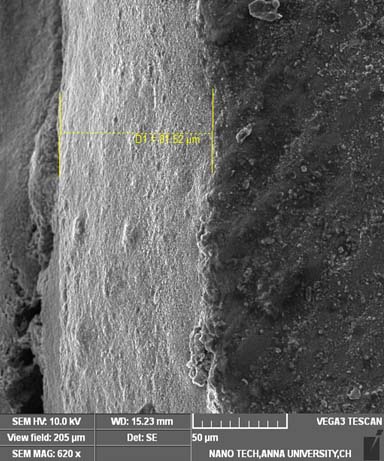
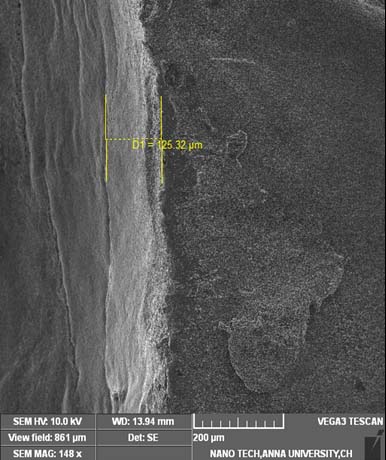
The test specimen is mounted over the prepared teeth was held in position using the resin jig under the scanning electron microscope (TESCAN Model Type: VEGA3 Series: SBU, Czech Republic) with a magnification of 1,00,000x and the marginal discrepancy was estimated. The marginal discrepancy was observed in two dimensions, vertical and horizontal. Horizontal marginal discrepancy is the distance between the axial tooth surface and the intaglio surface of the restoration in the most cervico-apical region, expressed as microns. Vertical marginal discrepancy is the measurement of the space present between the tip of the restoration to the finish line, expressed as microns.
The marginal discrepancy manifesting as vertical and horizontal marginal discrepancy were expressed as micrometers and categorized into prior and after luting groups [Table/Fig-12,3,4,5,6,7 and 8]. The values were tabulated and subjected to statistical analysis to test significance at 5% level. The nature of the data was ratio and hence parametric tests were used. One way analysis of variance was used to compare the mean values between the cements prior and after luting at 5% significance (α=0.05). This was followed by Tukey HSD Post-hoc test for multiple comparison and results were interpreted.
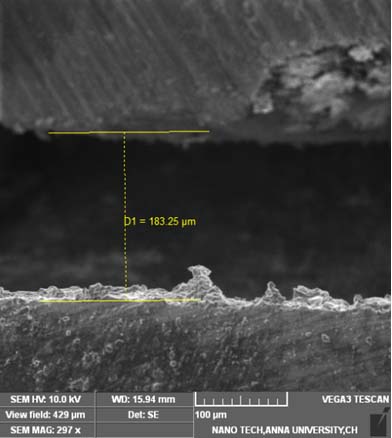
Horizontal marginal discrepancy with resin modified glass ionomer cement (Relyx) Group I.
Horizontal marginal discrepancy with PMMA based resin cement.
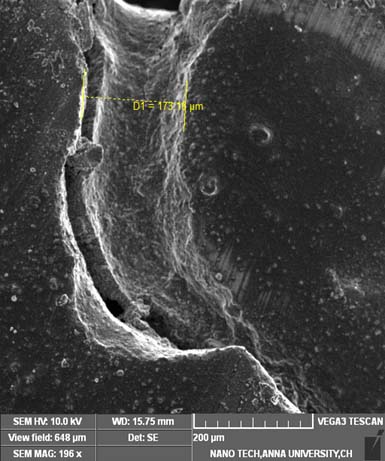
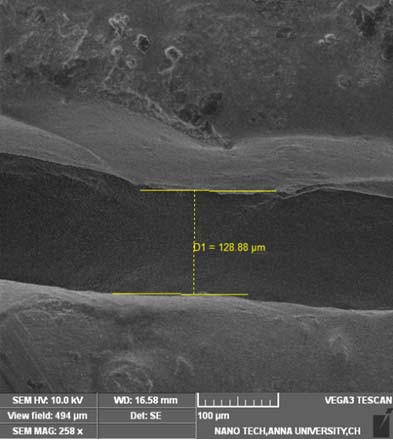
Horizontal marginal discrepancy with Bis-GMA based resin cement.
Horizontal marginal discrepancy with urethane dimethacrylate resin cement (Calibra) Group IV.
Vertical marginal discrepancy with resin modified GIC (Relyx) Group I.
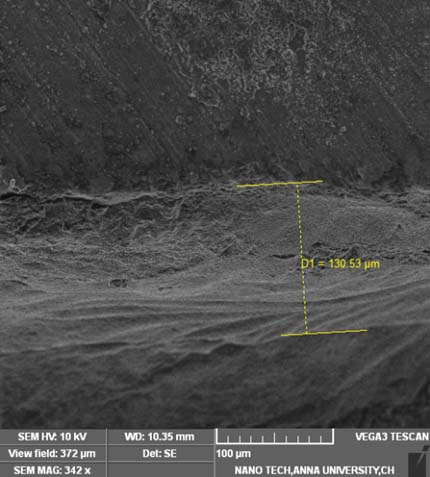
Vertical marginal discrepancy with PMMA based resin cement (Superbond) Group II.
Vertical marginal discrepancy with Bis-GMA based resin cement (Variolink II) Group III.
Vertical Marginal discrepancy with urethane dimethacrylate resin cement (Calibra) Group IV.
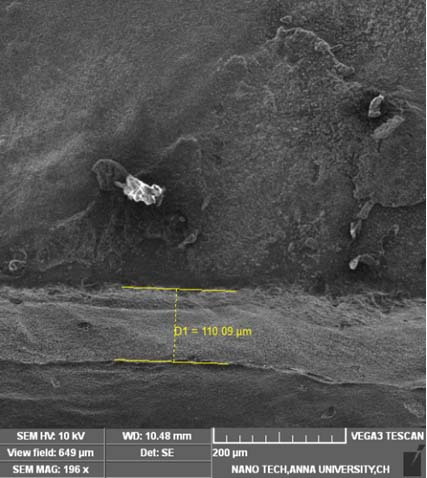
SEM samples for horizontal and vertical marginal discrepancy after cementation.
Results
[Table/Fig-9] shows the vertical marginal discrepancy and horizontal marginal discrepancy before and after cementation.
Marginal discrepancy before and after cementation.
| Variables | Cement | N | Mean | Std.Dev | F-Value | P-Value at 5% sig |
|---|
| Vertical before cementation | Calibra | 27 | 260.28 | 64.81 | 0.275 | 0.843 |
| Superbond | 27 | 272.47 | 86.25 |
| Variolink | 27 | 254.21 | 79.20 |
| Relyx | 27 | 270.08 | 103.10 |
| Total | 108 | 264.26 | 83.61 |
| Horizontal before cementation | Calibra | 27 | 233.08 | 69.44 | 1.309 | 0.275 |
| Superbond | 27 | 251.82 | 62.69 |
| Variolink | 27 | 234.81 | 79.75 |
| Relyx | 27 | 270.86 | 102.70 |
| Total | 108 | 247.65 | 80.44 |
| Vertical after cementation | Calibra | 27 | 116.98 | 17.71 | 9.092 | <0.001 |
| Superbond | 27 | 142.08 | 50.83 |
| Variolink | 27 | 117.75 | 24.29 |
| Relyx | 27 | 165.31 | 53.00 |
| Total | 108 | 135.53 | 43.94 |
| Horizontal after cementation | Calibra | 27 | 116.58 | 21.13 | 10.297 | <0.001 |
| Superbond | 27 | 136.07 | 44.95 |
| Variolink | 27 | 116.89 | 18.22 |
| Relyx | 27 | 166.62 | 54.96 |
| Total | 108 | 134.04 | 42.83 |
Stastical test used : One Way Analysis of Variance
[Table/Fig-10] shows Tukey HSD Post-hoc test for multiple comparison for vertical marginal discrepancy after cementation that there was a high statistical difference between (Calibra) Group IV and (Rely X) Group I and (Variolink II) Group II and (RelyX) Group I (p<0.01) and no statistical difference observed with other cements. For horizontal marginal discrepancy, statistically significant difference was observed between (Calibra) Group IV and (RelyX) Group I and (Variolink) Group II and (RelyX) Group I (p<0.01). No statistically significant difference was observed for the other cements.
Tukey HSD Post Hoc tests for multiple comparisons.
| Outcome Variable | Luting Cement | Mean Difference | P-Value at 5% sig |
|---|
| Vertical discrepancy after Cementation | Calibra | Superbond | -25.10 | 0.099 |
| Variolink | -0.77 | 0.099 |
| RelyX | -48.33 | <0.001 |
| Superbond | Variolink | 24.33 | 0.116 |
| RelyX | -23.33 | 0.144 |
| Variolink | RelyX | -47.56 | <0.001 |
| Horizontal discrepancy after Cementation | Calibra | Superbond | -19.49 | 0.244 |
| Variolink | -0.30 | 0.999 |
| RelyX | -50.04 | <0.001 |
| Superbond | Variolink | 19.19 | 0.257 |
| RelyX | -30.55 | 0.021 |
| Variolink | RelyX | -49.73 | <0.001 |
Discussion
Dissolution of luting cements is an important clinical problem well documented in the literature [6,7] and the primary aetiology constituting this phenomenon include variation in salivary pH, quantity of gingival crevicular fluid and plaque accumulation, microbial colonization which subsequently leads to dissolution of luting cement inducing microleakage and marginal discrepancy.
Resin cements by virtue of their chemical structure are more resistant to dissolution by water, beverages, saliva and gingival crevicular fluid and offers better resistance to plaque accumulation and microbial colonization; whereas, other cements are prone to dissolution and subsequent secondary caries of the abutment could occur with time. Resin cements have been modified to release fluoride to prevent secondary caries.
The commonly used resin cements are Bis-GMA, urethane dimethycrylate and PMMA based cements. The disadvantages associated with resin cements include soft tissue irritation, periodontal breakdown when the cement is not cleaned properly following luting. Since the resin cements are highly resistant to dissolution the cement that remains trapped inter-proximally can induce a marked inflammatory response triggering periodontal breakdown.
There is a possibility of chemical trauma to the pulp from the unpolymerized resin residues.
Rinke S et al., comparatively evaluated the marginal adaptation and fracture resistance of copy-milled and conventional In-Ceram crowns [8]. The marginal accuracy of the copy-milled units ranged from 6 to 153μm, and that of the conventionally fabricated units ranged from 1 to 153μm. Sulaiman F et al., reported the mean marginal discrepancy of All ceramic crowns was, in descending order: In-Ceram (161±46μm, Procera (83±41μm) and IPS Empress (63±46μm). Both Procera and IPS Empress met the criterion for acceptable marginal discrepancy of 120μm [9].
Beschnidt SM et al., reported Empress staining technique crowns showed least marginal discrepancy with median of 47μm, followed by the conventional In Ceram crowns (median 62 μm) and Empress veneer technique crowns (median 62μm) [10].
Nakamura T et al., reported the alumina cores fabricated had mean discrepancies of 30 to 40μm at the margins of the labial and lingual sides, which was significantly smaller than the gaps produced by the conventional method (67 to 130μm) [11]. Suarez MJ et al., studied the influence of two finish line configurations on the marginal accuracy of Procera All Ceram crowns. The marginal gap was within the range of clinical acceptability [12].
Okutan M et al., proposed a study to evaluate the fracture load and marginal accuracy of crowns made from a zirconia based ceramic cemented with glass-ionomer or composite cement and reported similar results with the cements [13]. Lee KB et al., and Martinez Rus et al., reported internal gaps of conventional All ceramic crowns were within the range of 123 to 154μm. Cerec 3D crowns (109.5±4.7μm) showed significantly larger gaps than the procera system (Copings 71.4±5.3μm, crowns 68.8±6.9μm) [14,15].
Results of ANOVA for this present study inferred a statistically significant difference between the four test specimen with regards to vertical and horizontal marginal discrepancy after cementation. (F=9.092 p<0.001) for vertical marginal discrepancy (F=10.97 p<0.001).
The resin based cements exhibited greater reduction in both vertical and horizontal marginal discrepancy than the resin modified GIC in this study. Celik C et al., have reported no significant difference between the resin bonded cements regarding marginal discrepancy when luted for All ceramic restorations [16]. Quintas AF et al., have reported an increase in the marginal discrepancy following luting with resin cements [17]. Borges GA et al., also evaluated in-vitro marginal fit of three All ceramic crown systems before and after cementation have observed both resin modified glass ionomer and resin cements induce increase in marginal discrepancy [18]. Abbate MF et al., reported the marginal openings ranged from 56 to 81μm in their study [19]. The present study observed mean marginal discrepancy of All ceramic restorations were about 200μ, so the cement had enough space to be accommodated facilitating better seating of the restoration, hence reduced the amount of the marginal discrepancy. Clinical conditions like type of finish line placement of margins viz., supra-gingival margin, sub-gingival margin, crestal gingival margin, salivary pH, brushing technique could influence the performance of the luting cements and marginal discrepancy could be altered under such circumstances. Hence, clinicians should judiciously choose the luting cement for All ceramic restorations after evaluating all the parameters to ensure clinical success. The clinical significance in the study include preference of resin cements over the glass ionomer for luting All ceramic restoration by virtue of its greater reduction in the marginal discrepancy between the tooth surface and the restoration.
Limitation
The limitation of the study includes non-measurement of marginal adaptation in the entire intaglio surface of the restoration tooth surface. Specialized digital imaging techniques [20,21] and optical coherence tomography [22] can be used to study this phenomenon further in the future.
Conclusion
This study inferred a significant difference in the amount of marginal discrepancy between All ceramic restoration luted with the resin cements and resin modified GIC. Resin cements exhibited a greater reduction in the marginal discrepancy than the resin modified glass ionomer following luting. No significant difference in marginal discrepancy was observed between the experimental resin cements. Hence resin cements are more suitable for luting All ceramic complete veneer crowns.
Stastical test used : One Way Analysis of Variance