Chronic Osteomyelitis of Skull due to Pseudomonasaeruginosa: A Delayed Uncommon Complication Following Craniotomy
Swati Khullar1, Poodipedi Sarat Chandra2, Ramesh Sharannappa Doddamani3, Arti Kapil4, Benu Dhawan5
1 Junior Resident, Department of Microbiology, All India Institute of Medical Sciences, Ansari Nagar, Delhi, India.
2 Professor, Department of Neurosurgery, All India Institute of Medical Sciences, Ansari Nagar, Delhi, India.
3 Assistant Professor, Department of Neurosurgery, All India Institute of Medical Sciences, Ansari Nagar, Delhi, India.
4 Professor, Department of Microbiology, All India Institute of Medical Sciences, Ansari Nagar, Delhi, India.
5 Professor, Department of Microbiology, All India Institute of Medical Sciences, Ansari Nagar, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Benu Dhawan, Department of Microbiology, All India Institute of Medical Sciences, Ansari Nagar, Delhi, India.
E-mail: dhawanb@gmail.com
Craniofacial skeleton, Delayed infection, Multidisciplinary management
Dear Editor,
Delayed infection leading to osteomyelitis of the craniofacial skeleton is one of the most serious complications of cranial surgery. Though the prevalence of osteomyelitis is decreasing because of the use of broad-spectrum antibiotics, it is still a significant and challenging issue in developing countries. We report a case of temporal bone osteomyelitis in a child due to Pseudomonas aeruginosa, which occurred as a delayed infection following craniotomy.
A non-diabetic nine-year-old boy presented to the neurosurgical outpatient department of our hospital with a 6 months history of purulent discharge from the left temporal region of the skull with no documented fever or other associated systemic manifestations. A detailed history revealed that the patient was an operated case of Dysembryoplastic Neuroepithelial Tumour (DNET) diagnosed at 4-years of age. The patient underwent left temporal craniotomy and partial removal of tumor with anterior temporal lobectomy in January 2011 at a private hospital. Postoperatively, the patient remained seizure free for 3-4 months, following which seizures recurred. The patient was reoperated at our Institute in December 2014. Gross total excision of the residual DNET/gliotic area with left temporal lobectomy was done. The patient remained seizure free on follow up. However, since past six months he was having purulent discharge from his scalp at the surgical site.
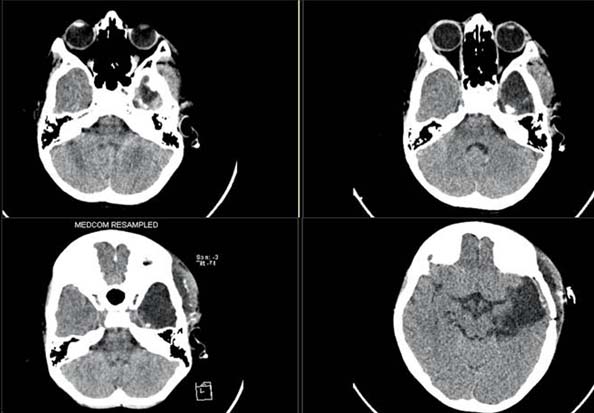
Computed tomography scan of the brain showed extradural enhancing soft tissue mass along with sclerosed irregular edges of the temporal bone [Table/Fig-1]. A diagnosis of osteomyelitis of left temporal bone was made.
Plain CT brain image showing temporal craniotomy defect with operative cavity, suggestive of temporal lobectomy. There is iso to hyperdense, extradural as well as subgaleal tissue indicating granulation tissue.
At time of admission, his body temperature was normal. Initial laboratory investigations showed total leucocyte count of 8600/mm3. Three consecutive blood samples and pus sample were sent for bacterial culture. One of the blood samples grew coagulase negative staphylococci which were considered a skin contaminant. Pus culture grew a mixture of gram negative bacteria. Empirical treatment with parenteral piperacillin-tazobactum (3.375 gm IV 8 hourly) was started. Clinically, there was no response to the therapy, as the discharge from the wound persisted. The patient underwent exploration and debridement. On exploration, the bone flap was found to be infected, hence was removed along with the miniplates and screws. Rhomboid flap reconstruction was done.
Bone, tissue and miniplates were sent for bacterial culture. Culture of all three samples yielded pure growth of Pseudomonas aeruginosa susceptible to ceftazidime, cefoperazone-sulbactum, piperacillin-tazobactum, imipenem, meropenem and resistant to amikacin and ciprofloxacin. Parenteral ceftazidime (1.5 gm IV 8 hourly) was added and continued for 3 weeks and piperacillin- tazobactum was eventually withdrawn. The patient had an uneventful recovery. On follow-up the wound had healed well.
The spectrum of complications of cranial surgery ranges from delayed infection, subgaleal fluid accumulation to resorption of preserved autografts, with delayed infection leading to osteomyelitis being the most serious complication of all. There may be an interval of 1 to 12 months between craniotomy and the onset of the infection [1]. Systemic signs might be mild despite the local signs of infection [2]. Our case also describes a similar presentation with minimal systemic signs and symptoms.
Distinguishing chronic osteomyelitis from acute osteomyelitis clinically may be difficult but presence of a chronic draining fistula suggests a long standing pathology, as was observed in this case. Chronic osteomyelitis is a serious condition and requires aggressive surgical treatment and antibiotic therapy.
Although, it is important to obtain blood cultures in all patients of osteomyelitis especially in whom haematological spread is suspected, the importance of tissue and other relevant samples collected at the time of the surgery cannot be underscored. The bacteria may be introduced from the scalp (furunculosis, infected wounds) or from a previous infection, trauma or bone surgery often leaving a residual focus. This may be further influenced by decreased host defenses ranging from decreased vascularity of the bone, diabetes, anaemia, malnutrition etc. Introduction of foreign body is another risk factor. Bacteria can remain alive on foreign body surfaces and may cause recurrent infections.
The main organism responsible for osteomyelitis due to delayed infection following craniotomy is Staphylococci [3,4]. However, the aetiological agent in our patient was Pseudomonas aeruginosa. Although Pseudomonas aeruginosa is known to cause osteomyelitis of the temporal bone in patients with malignant otitis externa [5,6], our patient did not have any evidence of otogenic infection.
The isolates of Pseudomonas aeruginosa were resistant to amikacin and ciprofloxacin. Rapidly acquiring resistance of Pseudomonasaeruginosa to antibiotics that are traditionally being used for treatment remains a matter of concern.
Multiple surgical interventions and presence of implants (plate and screws) in our patient predisposed him to develop iatrogenic chronic osteomyelitis wherein Pseudomonas aeruginosa was the causative pathogen, not commonly reported in similar patients. Appropriate tissue sampling, surgical wound debridement supplemented by a comprehensive microbiological work up aided in pathogen identification and targeted antibiotic administration for prompt clinical and symptomatic improvement in this child.
We recommend multidisciplinary management approach involving the neurosurgeon and the microbiologists in investigating and appropriately managing such cases.
[1]. Ryu J, Cheong JH, Kim JH, Kim CH, Kim JM, Delayed infection following cranioplastyJ Kor Neurotraumatol Soc 2005 1(1):110-13. [Google Scholar]
[2]. Tokoro K, Chiba Y, Tsubone K, Late infection after cranioplasty-review of 14 casesNeurol Med Chir (Tokyo) 1989 29(3):196-201. [Google Scholar]
[3]. Davies BM, Jones A, Patel HC, Implementation of a care bundle and evaluation of risk factors for surgical site infection in cranial neurosurgeryClin Neurol Neurosurg 2016 144:121-25. [Google Scholar]
[4]. Buang SS, Haspani MS, Risk factors for neurosurgical site infections after a neurosurgical procedure: A prospective observational study at Hospital Kuala LumpurMed J Malaysia 2012 67(4):393-98. [Google Scholar]
[5]. Mani N, Sudhoff H, Rajagopal S, Moffat D, Axon PR, Cranial nerve involvement in malignant external otitis: implications for clinical outcomeLaryngoscope 2007 117(5):907-10. [Google Scholar]
[6]. Ridder GJ, Breunig C, Kaminsky J, Pfeiffer J, Central skull base osteomyelitis: new insights and implications for diagnosis and treatmentEur Arch Otorhinolaryngol 2015 272(5):1269-76. [Google Scholar]