Meningitis with Digital Gangrene in Meningococcal Infection: An Atypical Presentation
Jitendra Singh1, Dandu Himanshu2, Ranjit Kumar Nim3, Anju Dinkar4, Kamlesh Kumar Gupta5
1 Senior Resident, Department of Medicine, King George Medical University, Lucknow, Uttar Pradesh, India.
2 Associate Professor, Department of Medicine, King George Medical University, Lucknow, Uttar Pradesh, India.
3 Senior Resident, Department of Medicine, King George Medical University, Lucknow, Uttar Pradesh, India.
4 Assistant Professor, Department of Microbiology, IMS, BHU, Varanasi, Uttar Pradesh, India.
5 Associate Professor, Department of Medicine, King George Medical University, Lucknow, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anju Dinkar, Assistant Professor, Department of Microbiology, IMS, BHU, Varanasi-221005, Uttar Pradesh, India.
E-mail: dranjudinkar@gmail.com
Meningococcal infection is an important public health concern. Neisseria meningitidis usually colonizes the nasopharynx of healthy adolescents and adults and remains as asymptomatic colonizer, while in rare cases it may present as invasive disease as either meningitis or septicemia or both. Most of the cases have typical presentation of rashes. We hereby present a case of a 40-year-old male who presented with meningococcal meningitis and peripheral digital gangrene but without development of typical rashes. He improved by early institution of appropriate intravenous antibiotics with supportive care.
Bacterial meningitis, Digital gangrene, Rashless presentation, Septicemia
Case Report
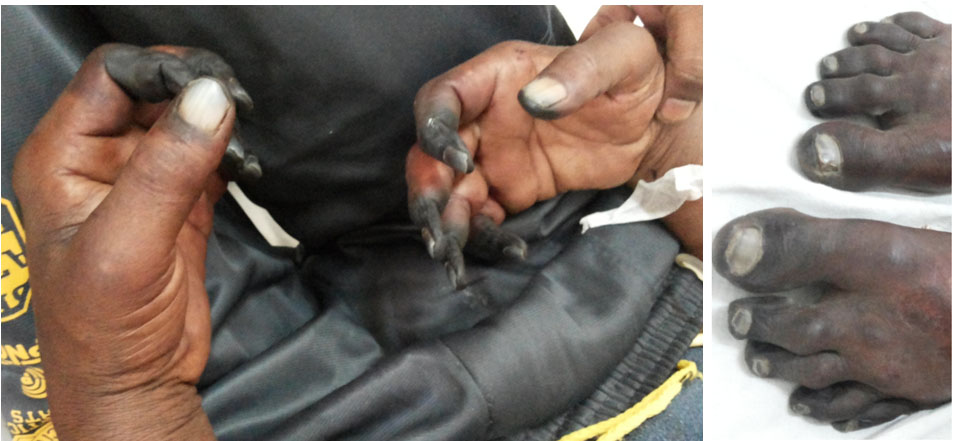
A 40-year-old male presented to the medicine department with complaints of high grade fever for five days, blackening of both hands and feet for three days followed by altered behaviour. On general examination, patient was febrile (temperature 102.5°F) without pallor, icterus or cyanosis. Dry gangrene of both hands and feet was present [Table/Fig-1,2]. All peripheral pulses of both, upper and lower limbs (brachial, radial, ulnar, femoral, popliteal, posterior tibial, dorsal pedis arteries), were palpable. His vitals were: pulse rate 110/minutes regular and brachial blood pressure in both arms 118/80mmHg. Examination of central nervous system revealed that patient was drowsy with Glasgow Coma Scale (GCS) of 11 (E3V3M5). Signs of meningeal irritations were present with bilateral extensor planter reflex. Bilateral pupils were equal and reactive to light. Rest of the systemic examinations were normal. There was no history of smoking, diabetes, hypertension, trauma, seizure, vasculitis, drug intake, heart disease and previous similar illness.
Dry gangrene of both hands and feet.
Laboratory tests showed Hb-14.1gm/dl, total leucocyte count of 13200/mm3 with predominant neutrophils, platelet count 140000/mm3, random blood sugar 104mg/dl, serum Na+ 137mEq/L, serum K+ 4.4mEq/L, blood urea 50mg/dl and serum creatinine 1.1mg/dl. His liver function test was mildly deranged (alanine aminotransferase; SGPT 60 U/L, aspartate aminotransferase; SGOT 65U/L and alkaline phosphatase; SALP 150U/L). Erthyrocyte Sedimentation Rate (ESR) by Westergreen method was 17mm/hr. Serology for hepatitis A, B, C and ELISA for HIV were negative. Serum Antinuclear Antibody (ANA) test was negative. Blood culture showed growth of meningococci. Lumbar puncture was performed and Cerebrospinal Fluid (CSF) was suggestive of bacterial meningitis (turbid, total cell count 600/mm3 with neutrophils predominant, protein 48mg/dl and sugar 15mg/dl). CSF culture was sterile. Doppler study of four limbs showed minimal/absent flow in small peripheral arteries of hands and feet. Rapid card test and smear for malaria parasite were negative. Bilateral fundus examination was normal. Chest X-ray and ultrasonography of abdomen were normal.
On the basis of clinical and laboratory findings, the standard protocol for management of meningococcal meningitis was started. He was given intravenous ceftriaxone 2gm 12 hourly for one week with adequate fluid resuscitation and supportive management. Necrotic tissues of digits were amputated in our surgical department. He responded well and was discharged on the 13th day of hospitalization. He was alright on OPD follow-up of three months.
Discussion
Neisseria meningitidis is a heterotrophic gram negative aerobic diplococcal bacterium. There are total 13 identified serotypes (A to L), while only 5 serotypes namely A, B, C, Y and W-135 are known to cause major invasive disease. It is estimated that about 5.2 cases per 100000 population are affected each year worldwide, while 10% individuals die. Generally, invasive meningococcal infection presented as meningitis or septicemia or combination of both and rashes are commonly associated with disease [1]. Meningococcemia is rarely reported without rashes [2]. On reviewing literature, unusual association with meningococcal infection was found whereas no other case of meningococcal meningitis presented with early vascular involvement without development of rashes was found [3].
Though meningitis and meningococcal septicemia are common clinical presentations but it may also manifest as pneumonia, purulent pericarditis, pyogenic arthritis or osteomyelitis, endophthalmitis, conjunctivitis, primary peritonitis and urethritis. Lipopolysaccharide is an endotoxin which is a component of meningococcal cell wall [1]. The pathophysiology of meningococcemia involves direct bacterial toxicity, cytokine release, ischemia, vasculitis and oedema. Meningococcal septicemia has more aggressive course and it is associated with high mortality [1,4,5]. Eventhough, death due to fulminant meningococcemia may occur within hours of the first symptoms. Rashes are developed in more than 80% cases of meningococcal disease. These rashes develop as a result of occlusion of small vessels by antigen antibody interaction in the dermis of skin. Rash may be absent during early phase of illness or in overwhelming sepsis [1]. It is often suspected on the basis of clinical presentations and diagnosis is confirmed by blood culture. Once endothelial injury occurred, it results in platelet-release reactions, local vasoconstriction and platelet plugs formation which leads to intravascular thrombosis. Severe thrombosis in the microvasculature of the skin may present in meningococcemia which often occurred in glove-and-stocking pattern that can necessitate amputation of digits or limbs [6]. Neisseria meningitidis is the second most common cause of community acquired bacterial meningitis in adults. It remains a major health problem especially in developing countries [7]. So, it is necessary to prevent the disease by cutting the route of transmission, proper vaccination and chemoprophylaxis of close contacts especially in rural areas.
Conclusion
This case report highlights the rarity of atypical presentation. Therefore, it is important for treating physicians to be aware of the rashless presentation of meningococcemia as early diagnosis and prompt treatment with high dose antibiotics has a good outcome.
[1]. Pollard AJ, Meningococcal Infections. Editors. Kasper DL, Hauser SL, Jameson JL, Fauci AS, Longo DL, Loscalzo JHarrison’s Principles of Internal Medicine 2015 19th edMcGraw-Hill Education:995-1003. [Google Scholar]
[2]. Sunita Singh M, Kapoor D, Atypical meningococcal meningitis with rashless presentation: A case reportJournal of Acute Disease 2012 1(1):72-74. [Google Scholar]
[3]. Dinkar A, Singh J, Atam V, Sahani KK, Patel ML, Self mutilating behaviour in severe meningococcal infection: An interesting associationJ Clin Diagn Res 2016 10(5):3-4. [Google Scholar]
[4]. El Bashir H, Laundy M, Booy R, Diagnosis and treatment of bacterial meningitisArch Dis Child 2003 88(7):615-20. [Google Scholar]
[5]. Pathan N, Faust SN, Levin M, Pathophysiology of meningococcal meningitis and septicaemiaArch Dis Child 2003 88(7):601-07. [Google Scholar]
[6]. Faust SN, Levin M, Harrison OB, Goldin RD, Lockhart MS, Kondaveeti S, Dysfunction of endothelial protein C activation in severe meningococcal sepsisN Engl J Med 2001 345(6):408-16. [Google Scholar]
[7]. Johri S, Gorthi SP, Anand AC, Meningococcal meningitisMJAFI 2005 61:369-74. [Google Scholar]