Kangaroo Mother Care (KMC) is a method which includes skin-to-skin contact between mother and preterm or Low Birth Weight (LBW) infant. It provides tactile, vestibular, kinaesthetic stimulation and transmits heat from the mother’s body to the infant’s body. It was originally created by Ray and Martinez at Bogota, Columbia as an alternative option to traditional incubator care of LBW babies as there was over-crowding and scarcity of resource availability in their country’s hospitals. It has now evolved into a practice which includes frequent or exclusive breastfeeding. With the emergence of better understanding of complex physiological mechanisms involved and the gathering evidence regarding its positive outcomes, KMC has gained wide acceptability across the world among the high income as well as low income countries [1–4]. We previously reported short-term outcomes of KMC (at 40 weeks corrected gestation) and observed that, KMC in the KMC ward is as effective as Conventional Method Care (CMC) in the Neonatal Intensive Care Unit (NICU) in the stable Very LBW (VLBW) infants [5]. However, information on short-term outcomes is insufficient to assess the overall benefits and risks of common post-natal interventions.
Materials and Methods
This was an open labeled randomized controlled trial conducted at a level III tertiary care hospital between April 2011 to August 2011. Methodology has been described in detail in our earlier article and requisite details are being mentioned again [5].
Randomization: Inborn singleton, VLBW (birth weight <1500gm) infants, tolerating spoon feeds of 150mL/kg/day and haemodynamically stable (not on oxygen or respiratory support, no apnea for 72 hours, not on any intra-venous fluids) were enrolled. Infants with major malformations were excluded. All enrolled neonates were randomized using random numbers generated using a web based random number generator; the same were placed in a serially numbered, sealed, opaque envelope and were opened after taking informed consent by the research coordinator. Babies were randomized to KMC or CMC.
Intervention: KMC: All infants allocated to KMC were shifted to the KMC ward. A trained nurse supervised the care of the baby in KMC ward. Neonates were given skin-to-skin contact between the mother breasts in an upright position dressed with a cap, socks and diaper and supported at their bottom with a cloth sling/binder. Front open gowns, comfortable chairs and beds were made available for the mothers. Mothers were encouraged to do KMC for as many hours per day as possible ensuring a minimum of eight hours per day. Infants were discharged home at a minimum weight of 1300grams or when gaining weight at a rate ≥ 10gm/day on 3 consecutive days if weight at randomization was >1300gm. Mothers were encouraged to continue KMC at home as long as the baby was tolerating it.
Conventional care: Infants allocated to CMC group (incubator/warmer) were cared in the NICU. Mother was encouraged for doing baby care such as diaper change, oil massage and paladai (type of spoon used commonly in India for feeding neonates) feeding. Infant’s temperature was maintained in the servo mode of the incubator. Infants were discharged home when they were euthermic (skin temperature of 36 to 37°C) in servo mode with heater output less than 25%, weight gain of ≥ 10g/day for 3 consecutive days, with minimum discharge weight of 1300g and mother/guardian confident in taking care of the baby. Feeding in both the groups was expressed breast milk given with a paladai at 2 hourly intervals along with direct breast feed on demand. When expressed breast milk was not available a preterm formula was used.
Follow-up and Outcome assessment: All the enrolled infants were followed regularly up to a period of 6 months to one year. At 6 to 12 months corrected age, the assessment included the measurement of growth parameters. The weight was recorded using an electronic weighing machine with a variability of 5 grams. The occipito-frontal circumference was measured with a non-stretchable tape and recorded in centimeters. The length was measured with an infantometer to the nearest 0.1 centimeters.
The physician assessing the growth outcomes was blinded to the intervention group of the baby. Nutritional indicators were assessed by: (i) Malnutrition (measured by weight-for-age); (ii) wasting (measured by weight-for-height); (iii) stunting (measured by height-for-age) and small head (measured by head circumference-for-age). We followed the World Health Organization (WHO) child growth standards. WHO Anthro 2005 software [6] was used for calculating the Z-score of each indicator. The cut-off point for malnutrition was a Z-score < 2 and severe malnutrition corresponded to a Z-score < 3. Feeding information included the duration of exclusive or partial breastfeeding (months of chronological age and of corrected age), the age (chronological age and corrected age) at which weaning diet was started and the type of weaning diet.
Statistical Analysis
Comparisons between study groups for primary outcomes and secondary outcomes were performed with Odds Ratio (OR) calculator using Medcalc online statistical software [7]. Continuous variables were compared by means of Student’s t-test. The study was analysed with “intention to treat” perspective (effectiveness as opposed to efficacy), all patients were according to the group to which they were allocated, regardless of compliance with treatment or contamination of the intervention.
Results
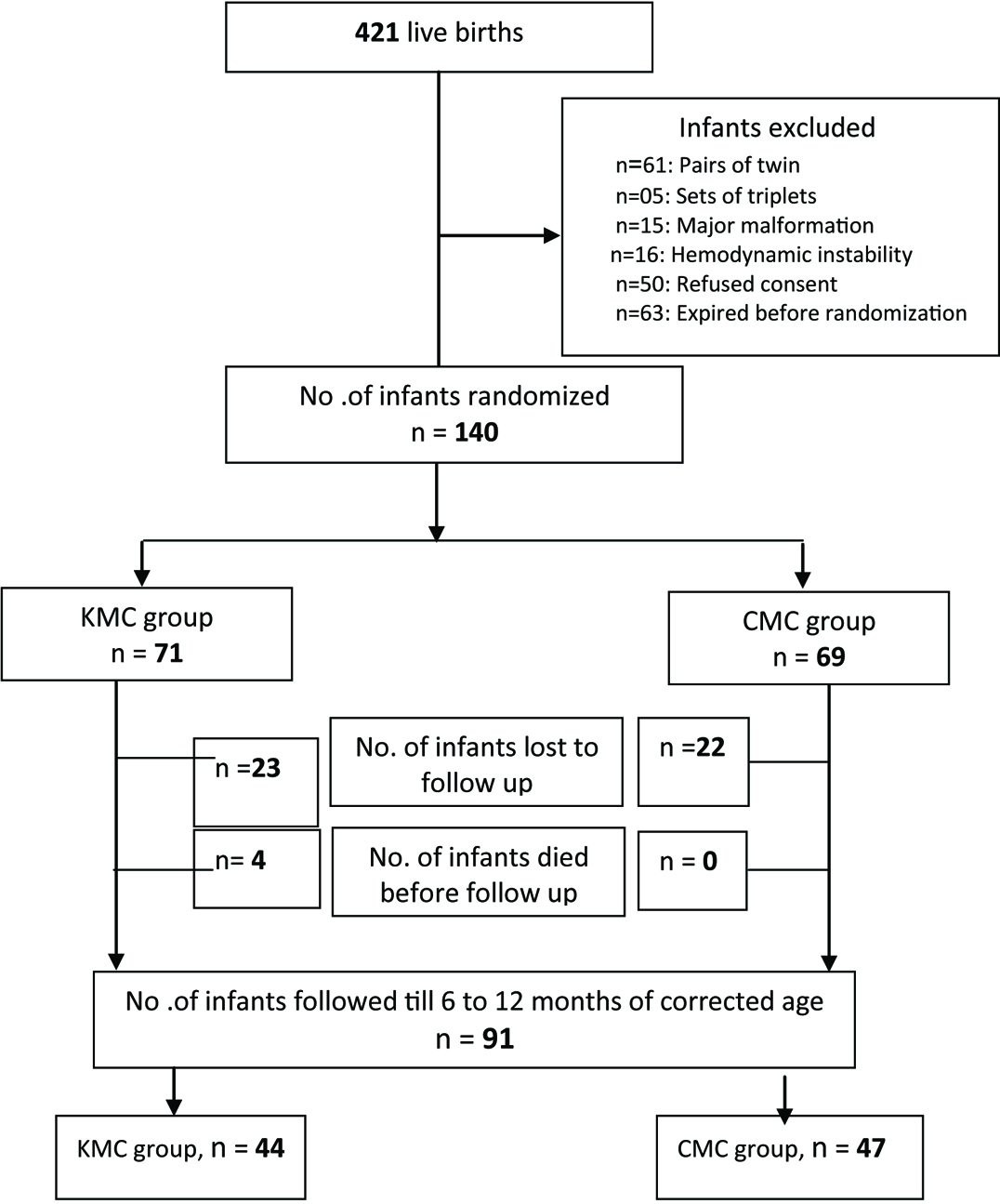
A total of 421 VLBW infants were born alive during the study period. After the exclusions, 140 infants were enrolled and randomized either to KMC (n=71) and CMC (n= 69) groups [Table/Fig-1]. Over all there was 65% follow-up till the corrected age of 6 to 12 months. Twenty three infants (32%) in the KMC group and 22 (32%) infants from the CMC group were lost to follow-up because the family got relocated and could not be contacted by telephone. Four infants (5.63 %) from the KMC group died before the first follow-up. Two of them died at 3 months of age with septicaemia, one at 4 months with pneumonia and another one at 2 months of age with intra-cranial bleed. None of the infants from the CMC group died after discharge. Adequate data for analysis was available for 44 (62%) and 47 (68%) infants from KMC and CMC group respectively. Males were 25 (56.8%) in KMC group and 25 (53.2%) in CMC group. Caesarian section deliveries were 42 (95.5%) in KMC group and 37 (78.7%) in CMC group. Small for Gestational Age (SGA) babies were 13 (29.5%) in KMC and 13 (27.7%) in CMC group. Resuscitation was required in 9 (20.5%) babies in KMC and 9 (19.1%) babies in CMC group.
[Table/Fig-2] describes the base line maternal and neonatal characteristics which were similar in both the groups. The mean (SD) corrected age at assessment was similar in both the groups. [Table/Fig-3] describes the primary and secondary outcome parameters and there was no significant difference in the primary and secondary outcomes in both the groups.
Base Line characteristics.
| Variable | KMC (n=44)Mean (SD) | CMC (n=47) Mean (SD) | p-value |
|---|
| Birth Weight (grams) | 1145 (175) | 1192 (177) | 0.21 |
| GA (weeks) | 30.7 (2.0) | 30.6 (1.97) | 0.81 |
| Weight at Randomization (grams) | 1179 (125) | 1201 (122) | 0.4 |
| GA at Randomization (wks) | 33 (1.53) | 33 (1.77) | 1.0 |
| Age at Randomization (days) | 15 (10.63) | 12.8 (8.85) | 0.28 |
| Corrected Age at Assessment (months) | 8.96 (2.69) | 9.8 (3.06) | 0.18 |
| Term Weight (grams) | 2453 (378) | 2576 (491) | 0.19 |
| Term Length (cm) | 46.6 (2.93) | 47.7 (3.16) | 0.09 |
| Term Head Circumference (cm) | 32.9 (1.54) | 33.4 (1.68) | 0.14 |
Primary and secondary outcomes.
| Variable | KMCn= 44 | CMCn= 47 | p-value | OR | 95%CI |
|---|
| Primary outcomes |
| Malnutrition(Z score < 2) n (%) | 21 (47.7) | 15 (31.9) | 0.13 | 0.51 | 0.22 - 1.2 |
| Stunting(Z score < 2) n (%) | 10 (22.7) | 6 (12.8) | 0.22 | 0.5 | 0.16 - 1.51 |
| Wasting(Z score < 2) n (%) | 15 (34.1) | 15 (31.9) | 0.83 | 0.91 | 0.38 - 2.17 |
| Small Head(Z score < 2) n (%) | 8 (18.2) | 15 (31.9) | 0.14 | 2.11 | 0.79 - 5.63 |
| Secondary outcome |
| Breastfeed (complete or partial) at 6 Month Post-Birth n (%) | 32 (72.7) | 34 (72.3) | 0.97 | 0.98 | 0.39 – 2.46 |
| Weaning at 6 Month Post-Birth n (%) | 31 (70.5) | 26 (55.3) | 0.14 | 0.52 | 0.22 – 1.23 |
| Type of weaning foods |
| Home Made n (%) | 19 (43.2) | 19 (40.4) | 0.89 | 0.79 | 0.39 – 2.06 |
| Cerelac(Market products) n (%) | 9 (20.5) | 9 (19.1) | 0.88 | 0.92 | 0.33 – 2.58 |
| Mixed n (%) | 16 (36.4) | 19 (40.4) | 0.37 | 0.68 | 0.29 – 1.59 |
Primary and secondary outcome analysis done by odds ratio calculator using Medcalc online statistical software [7].
Discussion
This is one of few randomized controlled trials evaluating the role of KMC on the long term effects in VLBW infants from this country. At 6 to 12 months of corrected age, the somatic growth parameters calculated as Z-scores using the WHO child growth standards for malnutrition, wasting and stunting did not show any difference between infants those who received KMC and CMC. The head growth was better in the infants in KMC group but had lesser weight and length compared to the CMC group but the difference was not statistically significant. When analysed for the severe (>-3 SD) malnutrition, wasting, stunting and microcephaly, the number of infants in the CMC group were more, though difference was not significant. We compared the growth parameters of infants with the WHO standards as each of the infant was followed-up at different age but within the ambit of 6 to 12 months of age corrected for gestation.
Similar findings were also observed in the Cochrane meta-analysis, which supports the use of KMC in LBW infants as an alternative to conventional neonatal care especially in resource-limited settings [8]. Sloan NL et al., reported that, there were no significant differences between the KMC and CMC groups in growth indices during the six month follow-up [9]. Ali SM et al., observed similar results at follow-up of 6 months corrected age and concluded that KMC was at least as effective as CMC [10]. However, these observations were made in higher weight infants i.e., LBW infants and not VLBW infants.
Though the percentage of VLBW infants was less in a study conducted by Charpak N et al., from France, the growth indices were observed to be similar in both groups except for height for corrected age at 9 to 12 months and head circumference from 3 to 12 months of corrected age which was found to be higher in the KMC group [11].
The growth parameters in the infants of KMC group and the CMC group might be similar because not many mothers continued doing KMC after discharge. These mothers had to get involved in the household work along with taking care of the infant. Despite counseling the family members regarding the advantages of continuing KMC after discharge, there was not much support to the mothers at home for doing KMC and all those mothers whose infants were randomized to CMC group were taught the feeding technique and the basic newborn care before discharge.
The breast feeding rates at 6 months corrected age in our study was similar in both the groups. Sloan NL et al., and Charpak N et al., also reported similar outcome in their studies [9,11]. Ali SM et al., from India reported a higher rate of breastfeeding in the KMC group at 6 months post-conceptional age [10]. However, we could not show this differential benefit, probably because both groups have relatively high prevalence of breast feeding at 6 months. Strict adherence to breast feeding is a rigorous policy in our hospital and on follow-up.
Weaning was started in more number of infants in KMC group at 6 months post-birth compared to those in CMC group, though difference was not statistically significant. Weaning was started with homemade food, market food like cerelac or mixed feeds and there was no statistically significant difference in preference of weaning food in either group.
As already discussed even at 40 weeks of corrected age, KMC was found to be as effective as CMC in terms of weight gain and increase in the length and head circumference. From this study we conclude that kangaroo care in KMC ward is an effective alternative to conventional incubator in the NICU for the management of stable VLBW infants and has similar impact on growth and feeding conditions not only at 40 weeks of corrected age but throughout infancy also.
Limitation
Limitation of the study includes considerable loss to follow-up and lack of record regarding implementation of KMC by mothers during the study period.
Conclusion
KMC group does not differ significantly with CMC group, in terms of long term growth and feeding pattern at 6 to 12 months of corrected age.
Primary and secondary outcome analysis done by odds ratio calculator using Medcalc online statistical software [7].