In recent years, we have witnessed different “evidence-based” guidelines in Hypertension (HTN) management [1–5]. The target Blood Pressure (BP) in the elderly and in those with co-morbidities is a major critical issue. Recommended target BP in these populations varies among guidelines. Raising the target systolic BP in patients ≥ 60 years to <150mmHg by the recent Joint National Committee (JNC)-8 was criticized by few of the panellists of JNC-8. They reported that, there is insufficient evidence for increasing the goal. BP and this may increase risk of Cardiovascular (CV) disease in such patients [6]. Also, the recommended target BP varied for HTN with co-morbidities [Table/Fig-1]. For Beta Blockers (BB), the indication advised by different guidelines is HTN associated with Coronary Artery Disease (CAD) and Heart Failure (HF) [2,3,5]. Further, the recommended interval prior to treatment modification, in newly diagnosed hypertensives, vary among the guidelines [1,2,5]. In addition to this, few physician surveys suggested that the clinicians’ hesitation to reduce BP to goal levels can contribute potentially to the health and economic burden associated with uncontrolled BP [7]. Given the lack of consensus in HTN management guidelines, we aimed to evaluate the current practice and perspectives of the physicians involved in management of HTN.
Materials and Methods
This cross-sectional, observational, questionnaire based survey was performed amongst attending delegate physicians at the 66th annual conference of Cardiological Society of India (Hyderabad, December 2014). Following a verbal consent, the physicians willing to participate were explained in brief about the survey. We sought perspectives related to current practices of the physicians (from different specialities like cardiology; endocrinology and internal medicine) with the help of a structured questionnaire. The questionnaire was assessed by all the authors in addition to two out of study experts for its completeness and self-administration. Questions were finalized only after inputs from all the experts. This questionnaire was related to clinical practice followed by physicians in routine. However, we did not conduct any pre-study pilot survey for assessing the questionnaire validity. Questions were related to the goal BP in the elderly, diabetes, CKD patients; use of BB and miscellaneous agent for the HTN treatment, strategies to the treatment changes and use of an Ambulatory Blood Pressure Monitoring (ABPM) in the routine clinical practice. Detailed questionnaire is provided in [Table/Fig-2]. Based on their clinical experience and approach, the physicians were requested to respond to the questionnaire. All the responses were recorded at a single-point of contact. Data collected was analysed with descriptive statistics.
Survey questionnaire adopted in our study.
| Q1. At what BP level, you start treatment in patients of HTN above 60 years without comorbidities? |
| a. > 150 or 90 | b. > 140 or 90 |
| c. > 140 or 80 | d. > 130 or 80 |
| e. Other____________________ |
| Q2. What is your BP goal in patients of HTN above 60 years without comorbidities? |
| a. < 150/90 | b. < 140/90 |
| c. < 140/85 | d. < 130/80 |
| e. Other____________________ |
| Q3. What is your BP goal in patients of HTN with Diabetes? |
| a. < 140/90 | b. < 140/85 |
| c. < 140/80 | d. < 130/80 |
| e. Other____________________ |
| Q4. What is your BP goal in patients of HTN with CKD without proteinuria? |
| a. < 140/90 | b. < 140/85 |
| c. < 130/90 | d. < 130/80 |
| e. Other____________________ |
| Q5. What is your BP goal in patients of HTN with CKD with proteinuria? |
| a. < 140/90 | b. < 140/85 |
| c. < 130/90 | d. < 130/80 |
| e. Other____________________ |
| Q6. In a newly diagnosed HTN, after how many days you modify treatment prescribed in order to achieve BP goal? |
| a. ≤ 15 days | b. 20 day |
| c. 30 days | d. 45 days |
| e. Other ___________________ |
| Q7. Which HTN Guidelines do you follow routinely in your clinical practice? |
| a. Indian HTN Guidelines | b. JNC Guidelines |
| c. ESC-ESH Guidelines | d. ASH-ISH Guidelines |
| e. NICE Guidelines |
| f. Other _____________________________________ |
| Q8. In what percentage of HTN patients, do you use ABPM? |
| a. < 10% | b. 10 – 25% |
| c. 26 – 50% | d. > 50% |
| Q9. In which clinical scenarios, do you prefer beta-blockers in management of HTN without comorbidities? |
| a. Initial agent in all patients | b. Initial agent in all patients aged < 40 years (young hypertensives) |
| c. Second line drug if BP uncontrolled with first drug | d. Third line agent after ACEIs/ARBs and CCBs or thiazide-diuretic |
| e. Other ______________________________________________________________ |
| Q10. In what percentage of HTN patients, you prefer drugs like alpha blockers, aldosterone antagonists, central sympatholytic, etc.,? |
| a. < 10% | b. 10 – 25% |
| c. 26 – 50% | d. > 50% |
Results
Guidelines Followed in Clinical Practice
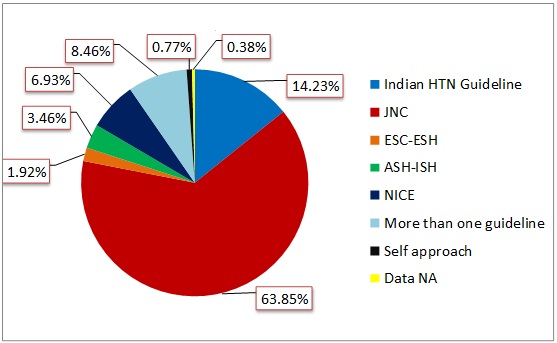
In this cross-sectional survey, 260 physicians participated. From the widely known HTN guidelines, majority of the physicians refer JNC guidelines (n=166) followed by Indian guidelines on HTN (n=37) [Table/Fig-3].
Guidelines commonly followed in clinical practice.
JNC-8: Joint National Committee-8, ASH-ISH: American Society of Hypertension and International Society of Hypertension, ESH-ESC: European Society of Hypertension-European Society of Cardiology, NICE: National Institute for Health and Care Excellence, NA – Not available.
Blood Pressure (BP) Threshold and BP Goal in Elderly (≥ 60 years)
BP goals recommended by various guidelines are outlined in [Table/Fig-1]. In patients aged 60 years and above [Table/Fig-4], more than half (n=150) of the physicians initiated treatment at BP ≥ 150 or 90mmHg as against one-third (n=90) who initiated at BP ≥ 140 or 90mmHg. BP goal of <140/90mmHg in the same population was practiced by most (n=113) of the physicians whereas nearly one-third (n=88) practiced the BP goal of <150/90mmHg. Lower BP goals were followed by some of the physicians as described in [Table/Fig-4].
Blood pressure goals practiced in different patient population.
| Population | n/N | % |
|---|
| BP threshold to start treatment in age ≥ 60 years |
| ≥ 150 or 90 mm Hg | 150/260 | 57.70 |
| ≥ 140 or 90 mm Hg | 90/260 | 34.61 |
| ≥ 140 or 85 mm Hg | 12/260 | 4.61 |
| ≥ 130 or 80 mm Hg | 7/260 | 2.70 |
| ≥ 160 or 90 mm Hg | 1/260 | 0.38 |
| BP goals in age ≥ 60 years |
| < 150/90 mm Hg | 88/260 | 33.85 |
| < 140/90 mm Hg | 113/260 | 43.46 |
| < 140/85 mm Hg | 23/260 | 8.85 |
| < 130/80 mm Hg | 34/260 | 13.08 |
| < 160/90 mm Hg | 1/260 | 0.38 |
| Data Not available | 1/260 | 0.38 |
| BP goal in diabetes mellitus |
| < 140/90 mm Hg | 57/260 | 21.92 |
| < 140/85 mm Hg | 25/260 | 9.61 |
| < 140/80 mm Hg | 15/260 | 5.77 |
| < 130/80 mm Hg | 161/260 | 61.92 |
| Other (<135/85 and <130/85) | 2/260 | 0.78 |
| BP goal in CKD without proteinuria |
| < 140/90 mm Hg | 63/260 | 24.23 |
| < 140/85 mm Hg | 34/260 | 13.08 |
| < 130/90 mm Hg | 35/260 | 13.46 |
| < 130/80 mm Hg | 125/260 | 48.08 |
| Other (120/80, 130/85) | - | - |
| Data Not Available | 3/260 | 1.15 |
| BP goal in CKD with proteinuria |
| < 140/90 mm Hg | 26/260 | 10.00 |
| < 140/85 mm Hg | 20/260 | 7.70 |
| < 130/90 mm Hg | 29/260 | 11.15 |
| < 130/80 mm Hg | 179/260 | 68.85 |
| Other (120/80, 130/85) | 3/260 | 1.15 |
| Data Not Available | 3/260 | 1.15 |
Blood Pressure (BP) Goal in Co-Morbid Conditions
In patients with T2DM, majority of the physicians (n=161) pursued the BP goal of <130/80mmHg. Proportions of physicians with other BP goals are presented in [Table/Fig-4].
A BP goal of <130/80mmHg is aimed for, by most physicians in patients suffering from CKD with proteinuria (n=179) as well as without it (n=125). In patients with CKD without proteinuria, nearly one-fourth (n=63) of the physicians aim for a BP goal of <140/90 mm Hg [Table/Fig-4].
Interval Prior to Modification of Treatment
When the BP goal is not achieved with the initial treatment prescribed in a newly diagnosed hypertensive patient, modification of treatment regimen was most commonly undertaken within 15 days (n=97, 37.31%,) or 30 days (n=93, 35.77%,) Modifying treatment regimen as per the need was practiced by only few of them.
Use of Ambulatory Blood Pressure Monitoring (ABPM)
ABPM, nevertheless, seemed unpopular among the physicians as most (71.93%) used it in less than five percent of their patients.
BB use in Hypertension without Co-morbidities
A lot of variation was observed in the use of BB in hypertension without co-morbidities [Table/Fig-5]. Most of the physicians (n=117) considered BB as third line agent after Angiotensin Converting Enzyme Inhibitors (ACEIs) Angiotensin Receptor Blockers (ARBs), Calcium channel blockers (CCBs) or diuretic agent. Interestingly, although a few of them (n=27) still use BB as first line agent in treating HTN. Some (n=35) don’t prefer BB in hypertension without comorbidities at all.
Preference of Beta Blockers in hypertension without comorbidities.
| Beta Blocker Use | n/N | % |
|---|
| As initial agent in all patients | 27/260 | 10.38 |
| As a second line if BP not controlled with first drug | 59/260 | 22.70 |
| As a third line agent after ACEIs/ARBs, and CCBs or diuretic | 117/260 | 45.00 |
| Don’t prefer in patients without comorbidities | 35/260 | 13.46 |
| Other* | 17/260 | 6.54 |
| Data not available | 5/260 | 1.92 |
*young hypertensive, coronary artery disease, HTN with high sympathetic tone.
Miscellaneous Drugs for Hypertension Management
Majority of the physicians (n=121, 46.54%) use drugs like aldosterone antagonists, alpha/alpha-beta blockers, etc. rarely in their practice (in <5% of their patients). Only few of them (n=30, 11.53%) uses such agent in >10% of their patients.
Discussion
Year 2013-14 was marked by release of the guidelines in major therapeutic areas like hypertension [1–3,5]. JNC-8 panel recommendations were criticized by some of its panellists for raising the systolic BP goal from <140 to <150mmHg in the elderly [1]. Though our survey indicates that most physicians (63.85%), across India refer to JNC guidelines, the target BP in elderly (≥ 60 years) aimed for by majority of the physicians (43.46%) was still <140/90mmHg. This is also reflected in IGH [5], which is the second most (14.23%) referred guideline and which recommends a target BP of <140/90mmHg in the elderly. Only a third of the physicians follow the JNC-8 recommended BP goal of <150/90 mmHg, indicating that most Indian physicians are not convinced with the new JNC recommendations. The impact of this raise in goal BP in elderly population was assessed by Banglore et al., in their revisited INVEST (International Verapamil SR Trandolapril study) trial [11]. In patients aged ≥ 60 years, BP goal of <150mmHg was associated with lesser benefits compared to <140mmHg. They observed significantly increased risk of CV mortality (p=0.04), total stroke (p=0.002) and non-fatal stroke (p=0.03) with goal of <150mmHg [11].
Presence of the comorbidities increase risk of CV events in patient of HTN [12,13]. A lower BP goal is recommended in patients with T2DM and CKD. Although, BP goal of <140/90mmHg is specified by most guidelines for T2DM, most physicians followed BP goal of <130/80 (61.92%) rather than <140/90 (followed by 21.92%). In a recent systematic review, Emdin et al., reported that in diabetic patients [14], lowering systolic BP by 10mmHg was significantly associated with lower mortality risk, CV events, Coronary Heart Disease (CHD), stroke, albuminuria and retinopathy. Patients with baseline BP ≥ 140mmHg had improved mortality benefits. In patients of T2DM with HTN, the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial [15] compared intensive BP lowering (<120mmHg) to standard group (<140mmHg) in patients of T2DM with HTN. At the end of one year, the intensive therapy (achieved mean SBP 119.3mmHg) did not reduce the composite outcome of non-fatal myocardial infarction, non-fatal stroke, or death from CV causes compared to standard therapy (achieved mean SBP 133.5mmHg). However, in a recent review considering the evidence from above two studies, Rosendorff C. suggested that lower BP goal (compared to recommended goal of <140/90mmHg) may be appropriate in patients with diabetes [16]. In patients with CKD, almost all HTN guidelines recommend BP goal of <140/90mmHg for patients without proteinuria and <130/90 mm Hg for patients with proteinuria (< 130/80 by NICE-CKD guideline) [1–3,5,9]. Interestingly, JNC-7 had recommended a BP goal of <130/80mmHg in HTN associated with diabetes and renal disease [7]. We observed that majority of the physicians followed lower BP goal of < 130/80mmHg in CKD patients with (68.85%) or without (48.08%) proteinuria. About a fourth of the physicians consider a target BP <140/90mmHg in the patients without proteinuria. Benefits of additional BP lowering to <140/90mmHg in CKD without proteinuria remains controversial. No renal or CV benefits have been reported with aggressive BP lowering [17]. Upadhyay et al., in a systematic review on BP target in CKD reported no benefit with additional BP lowering to 130/90 mm Hg compared to goal of 140/90mmHg [18]. However, they reported a beneficial effect of lowering BP to <130/90mmHg for proteinuria of more than 300 to 1000mg/day. Thus, the practice of lower BP goal in patients without proteinuria by the physicians needs to be re-emphasized. In a similar physician survey conducted by Mogi et al., in Japanese physicians, most physicians reported a goal BP of 130/80mmHg for diabetes and CKD whereas a goal of 140/90 mmHg was suggested for elderly patients with low CV risk [19]. Recently released SPRINT (Systolic Blood Pressure Intervention) trial reported lower rates of primary composite cardiovascular outcome (myocardial infarction, other acute coronary syndromes, stroke, heart failure, or death from cardiovascular causes) in the intensive BP lowering group (mean SBP = 121.4mmHg) than the standard group (mean SBP = 136.2mmHg) in non-diabetic high risk hypertensive patients (1.65% Vs 2.19% per year, hazard ratio 0.75; 95% confidence interval 0.64 to 0.89; p<0.0001) [20]. This reinforces the recommendation of a lower BP goal in high-risk hypertensive patients.
Guideline recommendations vary on the interval after which modification of treatment is to be made to achieve optimal BP control. Most surveyed physicians change the treatment (either increase dose/frequency or addition of other drug) in less than two-weeks or four-weeks (37.31% and 35.77% respectively) of initiation. Though, the specific interval varies amongst the guidelines and also the physicians, it is an individuals’ response to the BP lowering drugs that determines an effective approach to strategize a therapeutic regime.
ABPM is now an established standard practice in the HTN care for both adult and paediatric population. It provides prognostic value in hypertension especially associated with co-morbidities [21]. Almost 40% of the physicians consider the use of ABPM in just one percent of their patients. This indicates trifling use of ABPM in routine clinical practice possibly because of limited availability, patients’ discomfort, cost and operational difficulties associated with it.
BB were one of the initial agents recommended for HTN management in the past, though some (10.38%) physicians still considered them as first line agents. Most physicians (45%) abide by the JNC-8 recommendations [1] as is reflected in their preference of ACEIs/ARBs, CCBs and diuretics for the management of HTN. Guidelines have restricted the use of BB, selectively, in HTN associated with specific co-morbidities like coronary artery disease, and heart failure [1,2]. Survey from Mogi et al., revealed similar findings, with BB not being the first choice and rarely being used as second-line agents, among the physicians [19]. Miscellaneous agents used in HTN management like aldosterone antagonists, alpha-beta blockers, etc., did not seem popular; as majority of the physicians (85.77%) using such agents in less than 10% of their patients. This probably indicates that most physicians are not fully convinced with their usefulness and rely on mono- or combination therapies with major drug classes like ACEIs/ARBs, CCBs and diuretics along with BB in management of HTN.
Clinical Importance
Setting a BP goal is a difficult task in routine clinical practice as multiple factors needs to be weighed in, for each patient. Hypertension management is a complex subject with far too many variables (like age, gender, social background, comorbidities etc.,) to be considered. Hypertension management guidelines have evolved over time and they will continue to evolve, as more and more information becomes available. Indian physicians’ practice of lower BP goals needs to be re-emphasized to understand the adherence in the guidelines.
Benefit: Risk balance should prevail in considering individual BP goal by the physicians. The need to remain updated about changing guidelines recommendations and changing evidence in HTN management cannot be emphasized enough. A lower than recommended BP goal in high-risk non-diabetic hypertensive patients is beneficial as suggested by SPRINT trial [20].
Limitation
We only found practice of the physicians on BP goals but whether and to what extent these practiced BP goals lead to actual clinical benefit in-terms of reducing mortality and morbidity remains to be studied. Drug utilization pattern for achievement of BP goals was not assessed which could provide crucial information as to whether the treatment practices are aligned to or vary from guidelines recommendations. Also, practice of BP measurement need evaluation as the instruments and the procedures followed by each physician might vary significantly. Focused in-depth interview based interventional study would reflect practice of HTN management by the physicians much better than a simple questionnaire-based survey.
Conclusion
With literature evidence being the same, guidelines differ in their recommendations on BP goal. Overall, physicians followed a lower BP goal than the recommendations of various guidelines in patients with diabetes or CKD and aged 60 years and above. Physicians should take into considerations the clinical outcome benefits against the risks associated with lower BP goal. As anti-hypertensives, BB are now being used mostly in cases of HTN with comorbidities-especially CAD as recommended by guidelines. Use of ABPM still remains. In conclusion, Indian physicians practice lower BP goals than the recommendations of most referred JNC guidelines. Prospective, long duration and larger prescription- outcome studies are needed to understand HTN practices and changing trends in HTN management.
HTN: Hypertension, DM: Diabetes mellitus, CKD: Chronic kidney disease, JNC-8: Joint National Committee-8, ASH-ISH: American Society of Hypertension and International Society of Hypertension, ESH-ESC: European Society of Hypertension-European Society of Cardiology, NICE: National Institute for Health and Care Excellence, IGH-III: Indian Guidelines on Hypertension-III. * Age ≥ 50 years, † Age ≥ 60 years, ‡Age < 60 years, §NICE Diabetes Guideline, ||Nice CKD guideline.