A Rare Case of Multiple Myeloma with Biclonal Gammopathy
Abhik Banerjee1, Kshama Pimpalgaonkar2, Alap Lukiyas Christy3
1 Pathologist, Department of Clinical Chemistry and Immunoassays, SRL Central Clinical Reference Laboratory, Mumbai, Maharastra, India.
2 Biochemist, Department of Clinical Chemistry and Immunoassays, SRL Central Clinical Reference Laboratory, Mumbai, Maharastra, India.
3 Biochemist, Department of Clinical Chemistry and Immunoassays, SRL Central Clinical Reference Laboratory, Mumbai, Maharastra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kshama Pimpalgaonkar, Biochemist, Department of Clinical Chemistry and Immunoassays, SRL Central Clinical Reference Laboratory, Mumbai-400062, Maharastra, India.
E-mail: kshamapp@rediffmail.com
Multiple myeloma is a debilitating malignancy arising from plasma cells. These malignant plasma cells called myeloma cells proliferate and infiltrate the bone marrow. The disease is characterized by the presence of a monoclonal protein in plasma and/or the urine.
In this report, we present a case of biclonal multiple myeloma which showed two M bands on serum protein electrophoresis. The patient had elevated serum IgA and IgG levels. To reveal the nature of M bands or clonality, serum Immunofixation study was performed which revealed IgA with Lambda and IgG with Kappa light chains. Such pattern is very rare if we consider the various immunofixation patterns observed in different gammopathies.
Immunofixation electrophoresis, Neoplastic clonal disease, Serum protein electrophoresis
Case Report
A 64-year-old female patient presented with anaemia, fatigue and lower back pain since one month. Routine Laboratory investigations were done following a thorough clinical assessment. Haemoglobin was 10.8 g/dL, ESR was 101mm/1st hr. Serum albumin was 3.37g/dL (Reference range: 3.2-4.6 g/dl), whereas, serum calcium and creatinine were within normal limits. X-ray dorsal spine showed a lytic lesion in the body of D8 vertebra. X-ray lumbar spine showed evidence of degenerative changes at L4 and L5 level. The bone marrow aspiration showed 21% plasma cells including some binucleate forms. All these features were compatible with plasma cell dyscrasia suggestive of multiple myeloma.
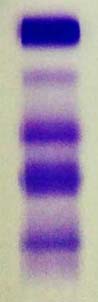
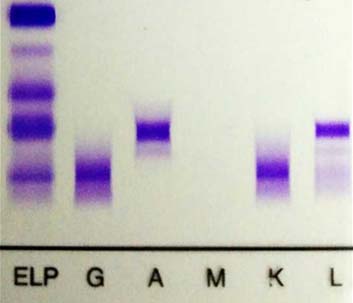
Serum protein electrophoresis and immunofixation electrophoresis were done. Serum protein electrophoresis on agarose gel revealed two sharp discrete bands in the gamma globulin region [Table/Fig-1]. Densitometric analysis of monoclonal components revealed M spike 1= 1.14 g/dl and M spike 2= 0.79 g/dl. On Immunofixation Electrophoresis (Sebia), serum revealed IgA lambda and IgG kappa gammopathy [Table/Fig-2].
Serum protein electrophoresis.
Serum immunofixation electrophoresis.
Serum β2 microglobulin measured by chemiluminescence was 8251.3ng/ml (Reference range: 609-2366ng/ml). Serum Immunoglobulin and free light chains levels were measured by nephelometry. IgG level was 18.20gm/L (Reference range: 6.5-16.4gm/L), IgM level was 0.92gm/L (Reference range: 0.39-3.38gm/L) whereas IgA level was 9.95 gm/L (Reference range: 0.90-5.32 gm/L). The free kappa chain level was 55.60mg/L (Reference range: 3.30-19.40mg/L) and the free lambda chains level was 63.70 mg/L (Reference range: 5.71-26.30mg/L) with a free kappa/lambda light chain ratio of 0.87 (Reference range: 0.26-1.65). Urine Bence-Jones protein was positive with heat coagulation test.
Thus a final diagnosis of Biclonal multiple myeloma was made. Unfortunately, patient could not be tracked to know regarding her treatment and subsequent follow-up.
Discussion
Multiple myeloma is a neoplastic clonal disease characterised morphologically by plasma cell infiltration of the medullary space and involvement of extraosseous tissues in a multi-focal fashion [1]. Monoclonal gammopathy is a group of B cell disorders which is known for production of a specific and unique M component. However, biclonal gammopathies are defined by simultaneous appearance of different M components, two distinct or different monoclonal proteins [2]. Biclonal gammopathy is relatively rare in M proteinemia and accounts for approximately 1-5% of all myelomas [3]. The most commonly encountered combination is IgG and IgA (53%), followed by IgM and IgG (24%) as per literature [2,3]. According to different literature, either one monoclonal cell clone in a monoclonal gammopathy may give rise to biclonal gammopathy or else, the same may arise from two different monoclonal cell clones. Hence, biclonal gammopathy may arise either due to independent proliferation of two separate clones of plasma cells where each clone gives rise to an unrelated monoclonal immunoglobulin or this may result from a single clone of plasma cells producing two different monoclonal proteins [4].
Biclonal gammopathies are more symptomatic than its monoclonal counterpart. However, no significant difference has been reported with monoclonal gammopathy in respect to clinical features, presentations or response to therapy. About 40% of the patients with biclonal gammopathies present with suggestive clinical signs and symptoms. A significant percentage of the symptomatic patients have underlying lymphoproliferative disease most commonly waldenstrom macroglobulinaemia. Nafia Al-Riyami et al., had recently described a rare occurence of biclonal gammopathy in a patient with Chronic Lymphocytic Leukemia (CLL) [5]. Rest of the symptomatic patients either have multiple myeloma or have some underlying non-haematolgical disorder. Nae Yu Kim et al., described a rare case of biclonal gammopathy accompanied by prostate cancer [4]. In our study, patient presented with anaemia, fatigue and low back pain. However, no underlying disorders were found other than multiple myeloma.
Ideal biclonal cases show two different Ig Light chain rather than two different Ig Heavy chain subtypes because most commonly a single myeloma clone can express a single type of light chain only. Hence, such true biclonal myeloma cases expressing both kappa and lambda are extremely rare. Between 1966 and 1979, a study was conducted on 57 patients detected with biclonal gammopathy. Out of these 57 patients, 53% patients had IgG, IgA components whereas 26% had IgG, IgM components. Of the 115 light chains, 70% were kappa and 63% were both kappa and lambda [3]. A large study comprising of 1027 plasma cell myeloma patients showed only 2% cases of biclonal gammopathy on serum protein electrophoresis [6]. However, there was no mention regarding the combinations of biclonal M-proteins detected in the study. There are few other reports where combinations of IgG/IgM, IgA/IgG, and kappa/lambda light chain biclonal gammopathies have been described [7–10]. Study of Nafia Al-Riyami et al., described a rare case of biclonal gammopathy with CLL which showed biclonal immunoglobin A (IgA) kappa and IgA lambda in serum immunofixation electrophoresis [5]. Mala Mahto et al., described a similar case of IgG Kappa and IgA Lambda type biclonal gammopathy detected by appearance of two bands in the gamma region on serum protein electrophoresis [11]. Bakta and Sutarka reported a rare case of biclonal gammopathy with IgA and IgM in a 48-year-old male patient [12].
Conclusion
Biclonal multiple myeloma accounts for only 1-5% of all myelomas. In the case presented above, we have reported IgA Lambda and IgG Kappa type of biclonal gammopathy detected by appearance of two bands in the gamma region on serum protein electrophoresis. The classes IgA Lambda and IgG Kappa were further confirmed by immunofixation.
[1]. Osterborg A, Hansson LO, Mellstedt H, Immunoglobulins in multiple myeloma. In: Garhton G, Durie B(eds)Multiple myeloma 1996 1st edLondonOxford University Press:36-50. [Google Scholar]
[2]. Osterborg A, Mellstedt H, Monoclonal and biclonal immunoglobulin producing disordersEurp J 1989 43(51):11-18. [Google Scholar]
[3]. Kyle RA, Robinson R, Katzman J, The clinical aspects of biclonal gammopathiesAm J Med 1981 71:999-1006. [Google Scholar]
[4]. Kim NY, Gong SJ, Kim J, Youn SM, Lee JA, Multiple myeloma with biclonal gammopathy accompanied by prostate cancerKorean J Lab Med 2011 31(4):285-89. [Google Scholar]
[5]. Al-Riyami N, Al-Farsi K, Al-Amrani K, Al-Harrasi S, Al-Huneini M, Al-Kindi S, Biclonal gammopathy in chronic lymphocytic leukemia: case report and review of the literatureOman Medical Journal 2015 30(3):216-18. [Google Scholar]
[6]. Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A, Review of 1027 patients with newly diagnosed multiple myelomaMayo Clinic Proceedings 2003 78(1):21-33. [Google Scholar]
[7]. Juge-Morineau N, Heirman C, Bakkus M, Van Camp B, Malfait R, Harousseau JL, Immunoglobulins D and M multiple myeloma variants are heavily mutatedClinical Cancer Research 1997 3(12):2501-06. [Google Scholar]
[8]. Huppmann AR, Liu ML, Nava VE, Concurrent diagnoses of Hodgkin lymphoma and biclonal myeloma in the bone marrowAnnals of Diagnostic Pathology 2010 14(4):268-72. [Google Scholar]
[9]. Franck P, Petitpain N, Guerci AP, Denisart S, Jacob C, Gueant JL, Myeloma with two monoclonal IgG and IgD in serum: a case reportActa Haematologica 1994 92(3):144-47. [Google Scholar]
[10]. Tharp AM, Woodruff RD, Shihabi ZK, IgD-Kappa myeloma: an unusual caseAnnals of Clinical and Laboratory Science 2003 33(1):97-100. [Google Scholar]
[11]. Mahto M, Balakrishnan P, Koner BC, Lali P, Mishra TK, Saxena A, Rare case of biclonal gammopathyIJCRI 2011 2(2):11-14. [Google Scholar]
[12]. Bakta IM, Sutarka IN, Biclonal gammopathy in multiple myeloma: a case reportGan To kagaku Ryoh 2000 27(2):544-88. [Google Scholar]