Routine abdominal drainage after laparoscopy cholecystectomy is an issue of considerable debate. Need for putting drains after Laparoscopy cholecystectomy is fear of collection of blood and bile which consequently led to open procedures [1]. Another reason for draining is to allow carbon dioxide insufflated during laparoscopy to escape via drain site thereby decreased shoulder tip pain. Shoulder tip pain is mostly due to diaphragmatic irritation by carbon dioxide which is left retained after laparoscopy cholecystectomy. This retained carbon dioxide is also a cause of post-operative nausea and vomiting [2]. This is evident from reduced nausea, vomiting in gasless laparoscopic cholecystectomy [3]. Residual gas resulted in loss of surface tension between viscera and parities in particular liver and diaphragm. The unsupported liver drags on its diaphragmatic attachments giving rise to shoulder tip pain. By using suction drains, it exerts its therapeutic effect by restoring normal surface tension between visceral and parietal peritoneum and hence reduced post-operative shoulder pain and nausea/ vomiting [4]. Higher wound infection has been reported in drain group [5]. Hospital stay is also prolonged as none of patient can be discharged on same day. Some studies demonstrate that infection rate and reoperation rate were not significantly different irrespective of whether drains were put or not [6,7]. Also, some studies show that pain post laparoscopy cholecystectomy was not statistically different between drain and no drain group [6–8]. Some studies show that drains results in increased post-operative pain and overall morbidity [9,10].
So, in review of this unresolved controversy regarding necessity of using drains in uncomplicated laparoscopy cholecystectomy, a prospective randomized study was performed with aim to assess the role of drains in uncomplicated laparoscopic cholecystectomy.
Materials and Methods
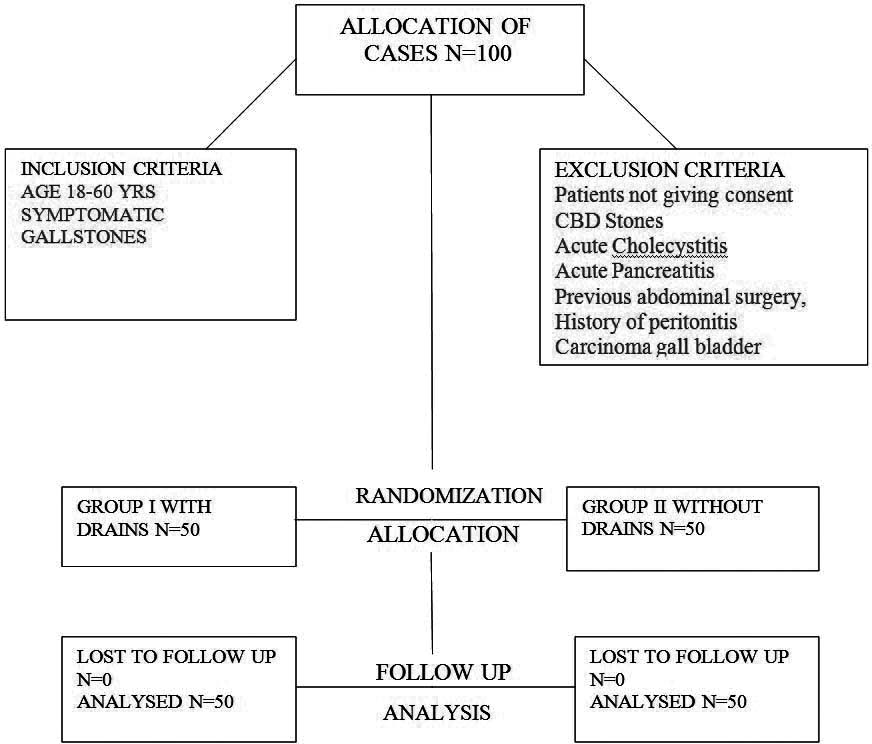
This study was conducted in the Department of General Surgery, Government Medical College and Rajindra Hospital, Patiala between 2007-2010. After approval from the hospital ethical committee, a randomized double blind study was conducted. Taking level of significance to be 5% and power of study to be acceptable at 80% with confidence level of 95% 2 Standard Deviation, a total of 100 patients with 50 patients in each arm were included. The inclusion criteria were patients having symptoms consistent with biliary colic having ultrasound evidence of gall stones. Patients not giving consent, having CBD Stones, Acute Cholecystitis, Acute Pancreatitis, Previous abdominal surgery, History of peritonitis and Carcinoma gall bladder were excluded from the study. After obtaining a written informed consent from the patients, they were randomly divided by computer generated numbers into 2 groups of 50 each. Any Intra-operative complication like liver bleed, cystic duct bleed, CBD injury were considered under complicated cases and were not included in study [Table/Fig-1].
Flow diagram of the progress through the phases of a parallel randomised trial of two groups.
Group I with 50 patients were operated for laparoscopic chole-cystectomy with suction drain placed in right subhepatic space and other group (Group II) had no drain placed after laparoscopic cholecystectomy.
Post-operative analysis was made in terms of operative time, Nausea and vomiting (0,6,12 hours post-operative) shoulder tip pain (incidence at 0,6,12,24,48 hours), analgesic requirements and hospital stay. Drain was removed, if the nature of discharge was serous and the amount was less than 30ml. Standard statistical method and tests (Chi-Square Test and Fisher-Exact Test) used for analysing the data.
Statistical Analysis
Descriptive statistics was done for all data and were reported in terms of mean values and percentages. Continuous variables were analysed with the unpaired t-test. Categorical variables were analysed with the Chi-Square Test and Fisher-Exact Test. Statistical significance was taken as p<0.05. The data was analysed using SPSS version 16.0 and Microsoft Excel 2007.
Results
Demographic characteristics of the patients were similar in the two groups. Average operative time in both the groups was also similar (p 0.977) [Table/Fig-2].
Demographic characterstics of both Groups. (Probabilities are shown in Asterisks)., **significant at p-value <0.05 * insignificant at p-value >0.05, Independent student t test
| Demographic Parameters | Group A | Group B | p-value |
|---|
| Age (Yrs) | 43.08±6.57 | 43.08±6.57 | 0.89* |
| Weight (Kg) | 65.84±5.6 | 66.12±9.86 | 0.86* |
| Operative Time | 56.5 min | 56.4 min | 0.977* |
There were more incidences of nausea /vomiting in Group II than in Group I. Shoulder tip pain was lower in Group I, in first 12 hours post-operative. However, after 12 hours, Group I, had higher shoulder tip pain than Group II Analgesic requirement was higher in Group II upto 12 hours after which it was higher in Group I.
In terms of hospital stay, Patients in Group I. had a longer stay in hospital as compared to Group II (2.96 vs 2.26 p <0.001) see [Table/Fig-3].
Comparison of Post-operative nausea/vomiting, Shoulder tip pain, analgesic requirements and hospital stay between two groups.
| Parameters | Drain GroupPercentage of pt.(time) number | No Drain Group | p-value |
|---|
| Nausea/Vomiting | 66%(0hours)33/5044%(6hours)22/5010%(12hours)5/50 | 94%(0hours)47/5098%(6hours)49/5078%(12hours)39/50 | 0.002**0.0001**0.0001** |
| Shoulder Tip Pain | 8%(0hours)4/508%(6hours)4/502%(12hours)1/5032%(24hours)16/5032%(48hours)16/50 | 18%(0hours)9/5018%(6hours)9/5014%(12hours)7/5024%(24hours)12/5010%(48hours)5/50 | 0.137*0.137*0.056*0.373*0.010** |
| Analgesic Requirement | 94%(0hours)47/5092%(6hours)46/5064%(12hours)32/5034%(24hours)17/506%(48hours)3/50 | 92%(0hours)46/5090%(6hours)45/5062%(12hours)31/5040%(24hours)20/5010%(48hours)5/50 | 0.695*0.727*0.836*0.534*0.461* |
| Hospital Stay | 2.96 Days | 2.26 Days | 0.001** |
**significant at p-value <0.05 * insignificant at p-value >0.05, Independent student t test
Discussion
The present study was conducted to assess the utility of subhepatic drain in uncomplicated laparoscopic cholecystectomy in alleviation of pain, nausea, vomiting and other complications of laparoscopic cholecystectomyIn this study, average operative time between two groups was not statistically significant which is consistent with various studies as depicted in the [Table/Fig-4] [1,11,12].
Average operative time between two groups among various studies.
| Studies | Drain | No drain | p-value |
|---|
| Hawasli [1] | 33 min | 30 min | 0.9 |
| Uchiyama [11] | 82.1 | 81.4 | - |
| Tzovaras [12] | 45 | 43 | - |
| Present study | 56.5 | 56.4 | 0.977 |
In this study there was more incidence of nausea/vomiting in Group II than in Group I which was statistically significant [Table/Fig-5] [1,2,7]. Thus all the studies showed higher incidence of nausea /vomiting in no drain group than in drain group. The reason for post laparoscopy nausea /vomiting is multifactorial. One of the proposed mechanisms is that CO2 insufflated causes increased cerebral blood flow thereby increasing nausea/vomiting [10]. Moreover retained CO2 leads to formation of carbonic acid which causes intra peritoneal acidosis and hence increased nausea /vomiting.
Incidence of nausea/vomiting among various studies [1,2,7].
| Author | Drain | No drain | p-value |
|---|
| Hawasli [1] | 24% | 34% | 0.6 |
| Nursal [2] | 31%(6hours)11%(12hours)6%(24hours)9%(48hours) | 38%(6hours)21%(12hours)15%(24hours)9%(48hours) | 0.60.20.040.6 |
| Mrozowicz [7] | 6% | 9% | 0.6 |
| Present study | 66%(0hours)44%(6hours)10%(12hours)8%(24hours)4%(48hours) | 94%(0hours)98%(6hours)78%(12hours)24%(24hours)8%(48hours) | 0.001 |
Elimination of CO2 by abdominal wall lifting devices has been reported to lead to less post-operative nausea/vomiting and fast recovery in laparoscopic cholecystectomy [13].
Drains placed in subhepatic space acts as a conduit for the escape of retained CO2 thus reducing intra peritoneal acidosis and hence reducing nausea /vomiting. This was seen in present study as well as other studies.
Shoulder tip pain was lower in Group I in first 12 hours post-operative. However after 12 hours, Group I had higher shoulder tip pain than Group II [Table/Fig-6].
Post-operative shoulder tip pain among various studies [1,2,7].
| Author | Drain | No drain | p-value |
|---|
| Hawasli [1] | 30% | 44% | 0.4 |
| Nursal [2] | 11%(0hours)17%(24hours)9%(48hours) | 15%(0hours)12%(24hours)6%(48hours) | 0.70.40.7 |
| Mrozowicz [7] | 13% | 3% | 0.05 |
| Present study | 8%(6hours)2%(12hours)32%(24hours)32%(48hours | 18%(6hours)14%(12hours)24%(24hours)10%(48hours) | 0.977 |
Mechanism of shoulder tip pain is multi factorial. Retained Co2 causes diaphragmatic stretch [14] which leads to phrenic nerve neuropraxia [15]
Retained carbon dioxide forms intraperitoneal carbonic acid which is directly proportional to duration of pneumoperitoneum and intra abdominal pressure. It seems that the total volume of CO2 may be a more important factor than the duration of exposure to CO2 [16].
Also, Co2 gets absorbed causing systemic hypercarbia which leads to sympathetic nervous system excitation resulting in amplification of local tissue inflammatory response [17].
Drain acts as a conduit for removal of subphrenic CO2 resulting in less formation of carbonic acid. Moreover, suction on the drainage tube results in further decrease of shoulder tip pain [4]. Suction drain may exert its therapeutic effect by restoring normal surface tension between visceral and parietal peritoneum [4]. Similar results are seen with other studies as mentioned. But increased incidence of shoulder tip pain beyond 24 hours is due to the fact that drain being a foreign body, irritates the diaphragm thus causing increased pain.
Analgesic Requirement
Analgesic requirement was higher in Group I upto 12 hours after which it was higher in Group II. This may be due to higher drain site pain in initial hours as well as increased mean intensity of pain in Group I. Although analgesic requirement is increased in no drain group beyond 24 hours, but it is not statistically significant. Similar results are seen with other studies [2,11,18].
Hospital stay
In terms of hospital stay patients Group I had a statistically significant longer stay in hospital as compared to Group II (2.96 vs 2.26;p <0.001). This statistically significant difference is due to the fact that none of the patient in the drain group could be discharged before removal of the drain. This increased overall hospital expenditure. Other studies also showed similar results [11,12,19].
Limitation
The study is limited by patient bias as patient with drain group can see the intervention of drain placed in abdomen as compared to patients without drains.
Conclusion
To conclude routine use of drains in laparoscopic cholecystectomy has not been found to be useful, it reduces nausea and vomiting but increases post-operative pain and hospital stay. It is reasonable to leave a drain if there is a surgical indication like potential bile leak i.e., imperfect closure of cystic duct or bile staining in the lavage fluid or gall bladder bed a indication for selective use of drain, bearing in mind that drain placement is a source of only false sense of security and its role in reducing post-operative shoulder pain and nausea/vomiting is not justified.
**significant at p-value <0.05 * insignificant at p-value >0.05, Independent student t test