Tuberculosis (TB) is transmitted mainly by droplet infection and droplet nuclei generated by sputum-positive patients with pulmonary TB. Coughing generates the largest number of droplets of all sizes [1]. Thus, its transmission is attributed to indiscriminate disposal of sputum by patients [2,3]. Patients and their immediate contacts should thus be cautious of where and how they collect and dispose potentially infectious sputum.
A study from West Bengal observed that only 33% of private practitioners use correct method of sputum collection [6]. It was observed among south Indian subjects that only half of them followed safe sputum disposal practice, which translates to the fact that only a small number of them collected sputum safely [7]. The perception and practices of infected individuals may affect the level of transmission of the disease. These may determine the control of the disease in the community. Guidelines and recommendations have been made regarding safe sputum disposal techniques for pulmonary tuberculosis patients [8]. Safe sputum disposal provides an effective measure to minimize the spread of the disease and health education efforts need to be strengthened to create better awareness of this important aspect of TB control [9]. Therefore, in this study, we studied perceptions about the disease and determined the sputum disposal practices followed by sputum-positive TB patients.
Materials and Methods
The present cross-sectional study was conducted among 422 subjects. Sputum-positive TB patients aged more than 15 years registered in the Tuberculosis Unit Ambala city from January 2012 – September 2012 formed the study population. Study subjects were randomly selected from both previously treated (Category II) and newly diagnosed patients (Category I) who had been on treatment for at least two months. Ethical clearance for this study, as per university norms, was obtained from the Institutional Ethics Committee for Human Research and permission was obtained from the DTO, Ambala city. Written informed consent was obtained from the study participants. The sample size was calculated − with an anticipated proportion of sputum-positive patients following safe sputum disposal as 50%, 5% absolute precision, 95% confidence interval and 10% non-response error − as 422 participants.
Inclusion criteria was sputum-positive TB patients aged more than 15 years and were put on DOTS treatment. Sputum-positive TB patients aged less than 15 years and sputum-negative TB patients were excluded from this study. A cohort of study subjects fulfilling the inclusion criteria were selected among the patients diagnosed with having sputum-positive TB at Tuberculosis Unit Ambala city and put on DOTS till the desired sample size i.e., 422 participants was achieved.
For the purpose of the current study, safe sputum disposal was defined as pouring boiling water in the sputum container, spitting in a bactericidal container (containers with 5% phenol/cresol/sodium hypochlorite), or spitting on a paper and burning it. Unsafe sputum disposal is defined as spitting indiscriminately or spitting in a public dustbin.
In this observational study, first of all, 422 participants were enrolled for the study as per inclusion criteria. At the end of one month, they were assessed for sputum collection and disposal practices by a trained person at their place of residences. Sputum disposal practices were assessed by checking their sputum disposal containers and asking relevant questions to them. Every effort was made to motivate the study subjects to adopt the correct and safe technique for sputum disposal at the end of each interview.
A structured questionnaire containing both open and close-ended questions was framed in consultation with the experts of the field for the purpose of capturing relevant details. Study variables were age, sex, education, different aspects related to knowledge of TB i.e., how does TB spread, correct method of sputum disposal, hazards of indiscriminate sputum disposal, etc. and practice related to sputum disposal, care taken while coughing, sneezing, etc. The questionnaire was designed in English initially and later translated in Hindi and retranslated to English to check the validity of questions contained. All the questionnaires were manually checked and edited for completeness and were then coded for computer entry. After compilation of collected data, analysis was done using Statistical Package for Social Sciences (SPSS), version 20.0. For statistical analysis, the χ2 test was applied. A two tailed p<0.05 was considered statistically significant.
Results
The mean age of the study population was 41±12.8years. Safe sputum disposal was practised by 46.4% of the study subjects. More females (70.4%) than males (39.2%) disposed sputum safely, as did more subjects of middle than low socio-economic status (n=146, 74.1% vs. n=50, 22.2%). A 70.9% (n=66) of the subjects with a family history of TB practiced safe sputum disposal methods as compared to 39.5% (n=130) subjects without a family history of TB practiced the same. Similarly, more literate than illiterate subjects (n=150, 57.5% vs. n=46, 28.6%) practiced safe sputum disposal methods. The difference in the proportion observed was found to be statistically highly significant (p < 0.001) in all the categories [Table/Fig-1].
Sputum disposal practices in relation to their socio-demographic factors among study subjects (N = 422).
| Category | Sputum disposal practices | Levelof Significance |
|---|
| Safe* (n = 196) | Unsafe (n = 226) |
|---|
| No. (%) | No. (%) |
|---|
| Sex |
| Male | 127 (39.2) | 197 (60.8) | < 0.001* |
| Female | 69 (70.4) | 29 (29.6) |
| Education |
| Literate | 150 (57.5) | 111 (42.5) | < 0.001* |
| Illiterate | 46 (28.6) | 115 (71.4) |
| Socio-economic status |
| Middle | 146 (74.1) | 51 (25.9) | < 0.001* |
| Low | 50 (22.2) | 175 (77.8) |
| History of tuberculosis in the family |
| Yes | 66 (70.9) | 27 (29.1) | < 0.001* |
| No | 130 (39.5) | 199 (60.5) |
Footnote: n - Number of study subjects (*indicates statistically highly significant)
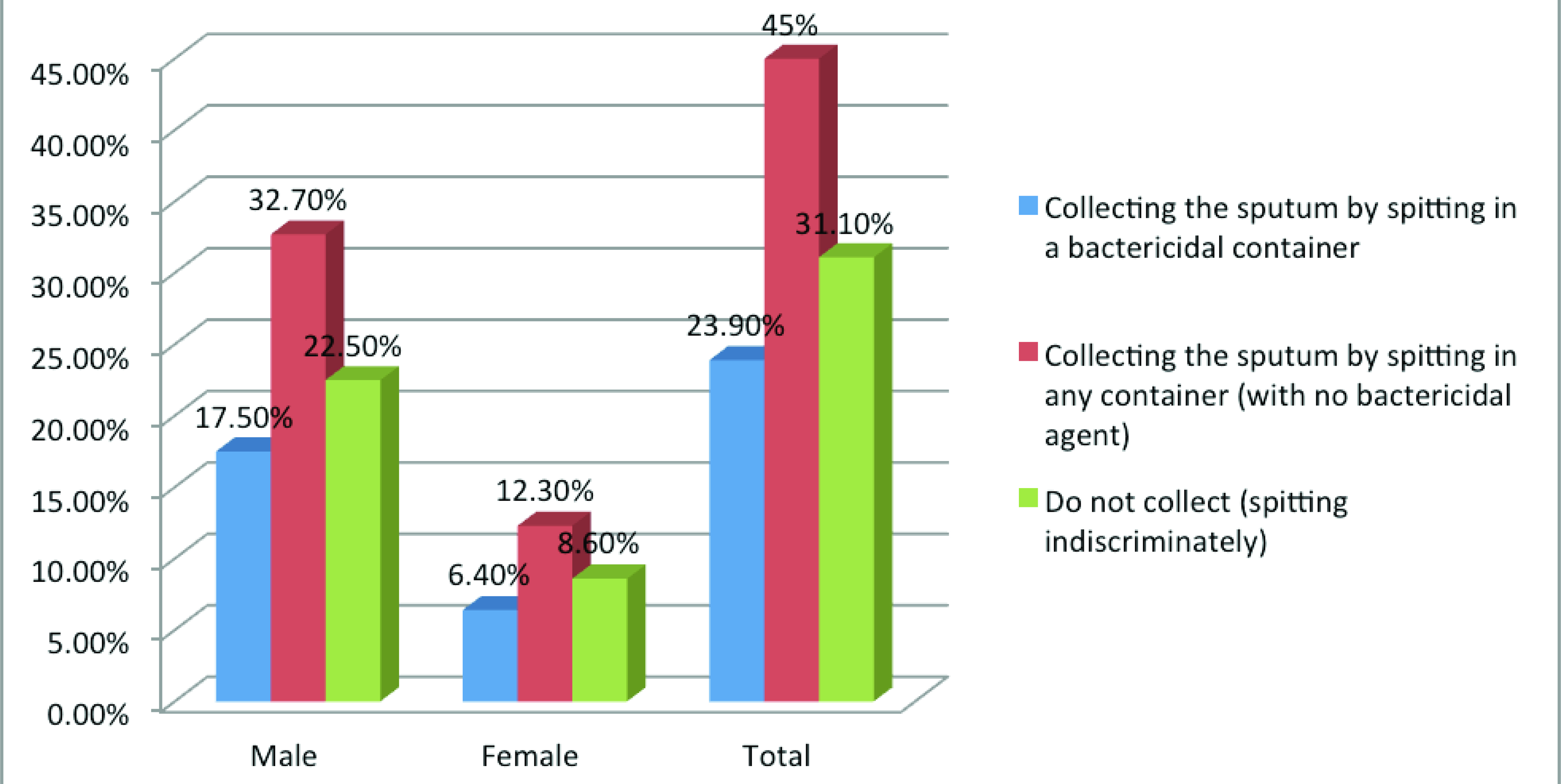
The majority (n=291, 68.9%) of the subjects collected their sputum in some form of container as compared to 31.1% (n=131) who did not collect their sputum at all. Gender wise males spitted indiscriminately more as compared to females [Table/Fig-2].
Gender wise distribution of sputum collection practices among study subjects.
Regarding knowledge of causation of TB, most of the study subjects were in the view that TB was a disease caused by multiple factors, the most common being smoking (n=287, 68%), followed by germs (n=266, 63%) and unhygienic living conditions (n=232, 55%). Regarding spread of TB, majority (n=245, 58.1%) of the subjects believed that tuberculosis spreads through contaminated water or food. 28% (n=118) and 24% (n=101) were in the view that this disease spreads by air and sharing cloths or towels with infected person respectively.
Discussion
It was observed in our study that safe sputum disposal was practised by 46.4% of the study subjects. Another study from coastal South India is also in concordance with our observations [7]. It is a matter of concern, as a single case of pulmonary TB can infect many others [10]. Hence, to ensure better control of the disease, it is imperative that all patients dispose their sputum safely.
Gender wise females disposed of sputum safely than males. Probably this could be due to the fact that the majority of the females worked in the home and therefore, had access to better tools required for sputum disposal methods such as boiling water, containers, etc. On the other hand, another study from Ethiopia among tuberculosis patients observed that gender wise there was no difference in sputum collection practices [11].
Regarding knowledge of causation of tuberculosis only 63% of the study subjects were in the view that this disease is caused by germs. The result of this study is in agreement with previous study from Tamilnadu [12]. But this is in contrast to the study by Bhattacharyya K from Kolkata, where only 17% of patients attributed the disease to germs [13]. A case control study by Sophia V et al., in 20 selected districts of the six states, found that patient’s knowledge regarding susceptibility to TB, its cause and spread and other related factors were assessed through a set of questions [14]. Patients exhibited poor knowledge. Findings of several other studies confirm the results of our study [15–17].
Not surprisingly, our study shows that illiteracy is another major determinant in the causation of any disease including. In our study, it was observed that 42.5% of literate and 71.4% of illiterate subjects did not dispose of their sputum properly. Illiterate patients may not be aware about the potential hazards of improper sputum disposal and might continue to do so despite repeated advice. The result of this study is in agreement with previous study by Rabahi MF and O’Boyle [18,19]. In the current study, it was also observed that the subjects with a family history of TB practiced much safer disposal methods than those whose relatives had not been previously infected. This finding can be attributed to better awareness of the disease among family members.
Unsafe sputum disposal can be improved by supervising the TB patients, which will help to reduce the transmission of TB in the community. This supervision should be stretched to used items like sputum cups, tableware, respirators and other everyday items, which can also spread TB. Health workers usually are not aware of rules regarding supervision of sputum disposal by patients with TB [20]. A detail of methods of supervision of sputum disposal by incorporating these aspects in the field level personnel’s training is need of an hour.
This study has several strengths. First, to our knowledge, assessment of the sputum disposal practices followed by sputum-positive TB patients in India has not been extensively investigated. Very few similar studies are available in the literature. The perception and behaviour of infected individuals may determine the quantum of incidence and level of transmission. This issue looks very simple and small but it has huge implication as far as prevention of tuberculosis is concerned. Situation becomes very relevant if it is applicable to high TB burden area. Second, data collection was conducted by a trained person, which created a sense of quality data gathering.
Limitation
The study has some limitations as well. First, some may argue that findings emerging out of this study may not be generalised. Because baseline data like income, literacy level, gender distribution and other socio-demographic-cultural factors tend to vary in different geographical areas. Administrative strength of RNTCP may also vary from place to place. Second, such a community-based study is always susceptible to recall bias. Third, educational intervention was not imparted.
Conclusion
The findings of the study highlight that a large number of pulmonary tuberculosis patients practiced unsafe sputum disposal. Unsafe sputum disposal was higher among males, illiterate patients and those belonging to the lower socio-economic group. The study demonstrated a glaring lack of awareness about the causes of disease, mode of transmission and control measures. Therefore it is need of the hour to launch Information Education and Communication (IEC) activities so as to improve the sputum disposal practices among tuberculosis patients. A large-scale educational interventional study is also warranted.
Footnote: n - Number of study subjects (*indicates statistically highly significant)