Outcomes of Capsular Dissection Technique with Use of Bipolar Electrocautery in Total Thyroidectomy: A Rural Tertiary Center Experience
Amal T. Das1, S.B. Prakash2, V. Priyadarshini3
1 Assistant Professor, Department of ENT and HNS, DM Wayanad Institute of Medical Sciences, Wayanad, Kerala, India.
2 Associate Professor, Department of ENT and HNS, DM Wayanad Institute of Medical Sciences, Wayanad, Kerala, India.
3 Assistant Professor, Department of ENT and HNS, DM Wayanad Institute of Medical Sciences, Wayanad, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Amal T. Das, Flat No. 312, Residential Block-3, WIMS Campus, Naseera Nagar, Meppadi, Wayanad – 673577, Kerala, India.
E-mail: dr.amaldas@dmwims.com
Introduction
Total thyroidectomy is one of the most routinely performed head and neck surgical procedures with extremely low mortality. This procedure has been associated with two major complications such as recurrent laryngeal nerve injury and hypocalcaemia due to parathyroid insufficiency. The use of bipolar electrocautery has not been widely accepted in view of thermal damage to adjacent structures.
Aim
To study the outcomes and complications of capsular dissection technique along with use of bipolar electrocautery in total thyroidectomy.
Materials and Methods
The study was conducted from May 2013 to May 2016. The study was performed at Department of ENT Otorhinolayngology, DM WIMS Hospital, Wayanad, Kerala, India. This retrospective descriptive study analysed the outcome of 130 patients who underwent total thyroidectomy by capsular dissection technique along with use of bipolar electrocautery for cauterization of vascular pedicles, at our institution over a 3 year period.
Results
The incidence of permanent unilateral vocal cord palsy was 1.5% and permanent hypocalcaemia was 2.3%. There was no case of haemorrhage or haematoma in this study.
Conclusion
Total thyroidectomy by capsular dissection technique along with the use of bipolar electrocautery has very low incidence of recurrent laryngeal nerve and parathyroid injury, as per our data. Hence, we recommend this technique along with routine use of bipolar electrocautery for total thyroidectomy.
Bipolar diathermy, Hypocalcaemia, Thyroidectomy, Vocal cord paralysis
Introduction
Total thyroidectomy is one of the most routinely performed head and neck surgical procedures with extremely low mortality. Theodore Kocher is considered as the father of thyroid surgery. He introduced the technique of capsular dissection and total thyroidectomy using aseptic precautions [1]. With the introduction of artery forceps in clinical practice in 1879, surgeons were able to get better haemostasis. The main complications associated with this procedure were recurrent laryngeal nerve injury and hypocalcaemia [2].
Some surgeons still perform bilateral subtotal thyroidectomy for benign thyroid diseases in order to prevent these complications and avoid the need for thyroid hormone supplementation. The problems associated with subtotal thyroidectomy included recurrence and long-term thyroid dysfunction needing thyroid supplementation [3].
Bleeding is one of the major post-operative complications of thyroid surgery. Intra-operatively, bleeding can obscure the surgical field of vision thereby, making identification of parathyroid glands and recurrent laryngeal nerves difficult. Traditional clamp and tie technique has enabled to achieve effective haemostasis. There are several studies which have reported the successful use of ligasure and harmonic scalpel in reducing blood loss [4–9]. The high cost of these vessel sealing generators and specialized handpieces make it unaffordable to most hospitals in developing countries. The use of bipolar electrocautery in thyroidectomy has not been widely accepted in view of thermal damage to adjacent structures. We wish to present our experience with capsular dissection and the benefits of bipolar electrocautery in total thyroidectomy.
Materials and Methods
This is a retrospective study of 130 total thyroidectomies performed by the ENT surgeon at Department of Otorhinolaryngology, DM WIMS Hospital, Wayanad, Kerala, India. The study was conducted from May 2013 to May 2016. Informed consent was obtained and study was approved by ethics committee. All the patients underwent total thyroidectomy by capsular dissection technique along with use of bipolar electrocautery for cauterization of vascular pedicles instead of tying knots. Patients with both benign and malignant lesions of thyroid were included in the study. Those patients with pre-operative recurrent laryngeal palsy and pre-existing calcium imbalance were excluded from the study. Patients undergoing re-operative thyroid surgery and concurrent lymph node dissection were also not included in this study. Those patients with thyrotoxicosis were controlled pre-operatively with anti-thyroid drugs and beta-blockers. All the patients were subjected to Ultrasonography (USG) of neck, Fine Needle Aspiration Cytology (FNAC) and thyroid function tests prior to surgery. Indirect laryngoscopy was done before the surgery to confirm the vocal cord mobility.
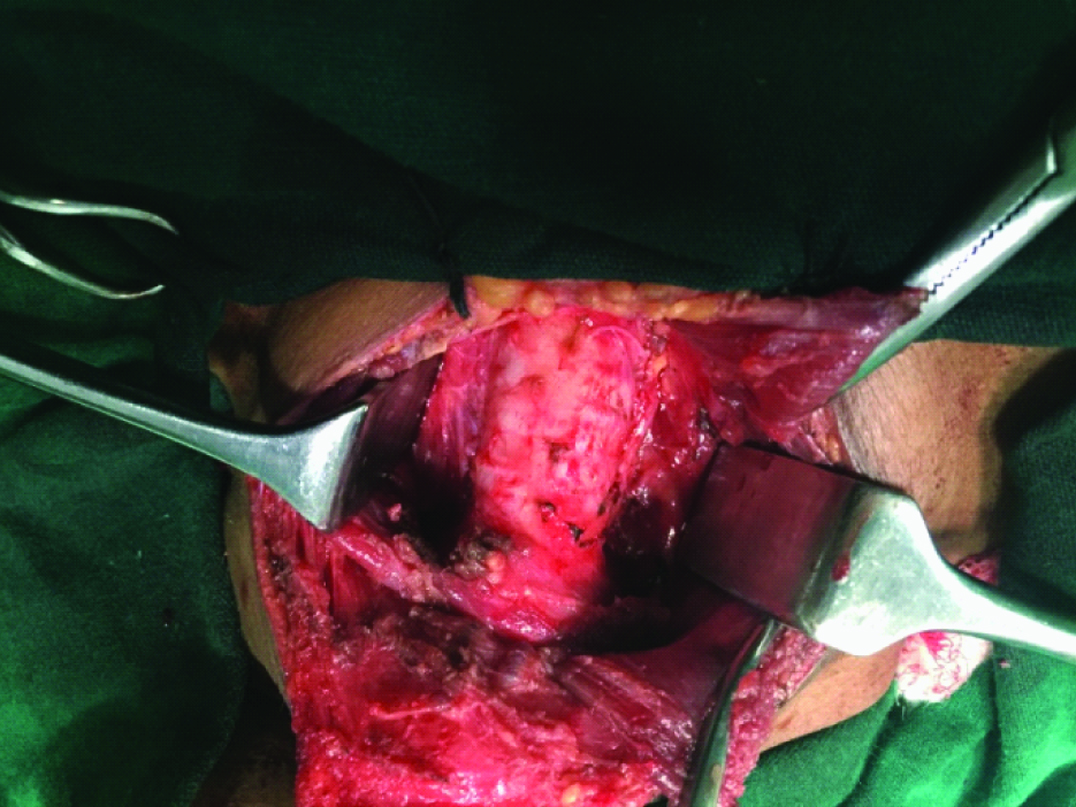
Intra-operatively the superior, middle and inferior thyroid vessels were divided with bipolar electrocautery. The distal extra-laryngeal course of recurrent laryngeal nerve was dissected on both sides [Table/Fig-1]. Parathyroid glands were preserved on both sides and inadvertent removal was managed by auto-transplantation at the lower one-third of sternocleidomastoid muscle. Hypocalcaemia was assessed clinically and biochemically in the post-operative period. Those patients who developed hypocalcaemia was stabilized with intra-venous calcium gluconate and oral calcium supplements along with vitamin D3 and discharged on the sixth or seventh day, while those who were normocalcaemic were discharged on the fourth or fifth day. All the patients were reviewed after one week and one month of surgery and assessed biochemically for serum calcium. Those with hypocalcaemia were reassessed after three months and six months. Permanent hypocalcaemia is considered when serum calcium does not return to normal within six months. Those patients with hoarseness of voice were assessed with videolaryngoscopy at the end of every month for the first six months.
Intra-operatively distal recurrent laryngeal nerves were dissected on both sides.
Results
Out of the 130 patients who underwent thyroid surgeries, majority of patients (54 cases) were in the age group of 41 to 50 years. Most of the patients were females (125 out of 130). In this study [Table/Fig-2], 92 patients underwent total thyroidectomy for multi-nodular goiter, 22 patients had multi-nodular goiter with retrosternal extension [Table/Fig-3], four patients had thyrotoxicosis which was controlled with medications pre-operatively, while only one patient had solitary nodule. There were 11 patients with cancer who underwent total thyroidectomy, of which four of them had papillary cancer while six patients had follicular cancer and one patient had medullary cancer.
Indication for total thyroidectomy.
| Indication | Number of cases |
|---|
| Solitary nodule | 1 |
| Multi-nodular goiter | 92 |
| Mult-inodular goiter with retrosternal extension | 22 |
| Thyrotoxicosis (Controlled) | 4 |
| Papillary cancer | 4 |
| Follicular cancer | 6 |
| Medullary cancer | 1 |
| Total | 130 |
As per this study, no patient had developed bleeding or haematoma despite using bipolar electrocautery for haemostasis. Thus, none of them required blood transfusion in the post-operative period. There was only a single patient who had developed seroma in the second post-operative week which was drained in the out patient department by needle aspiration. There were only two patients (1.5%) of multi-nodular goiter with retrosternal extension which had developed unilateral vocal cord palsy after the procedure. Both these patients developed adequate compensation of the vocal cords within 2 months as confirmed by videolaryngoscopy. There was only a single patient (0.77%) that had transient vocal cord palsy which recovered completely within one week. There were only 3 cases of permanent hypocalcaemia after total thyroidectomy, of which 2 cases had multi-nodular goiter with retrosternal extension greater than 2cm, while one case had thyrotoxicosis. There were 37 cases (28.5%) of temporary hypocalcaemia needing oral calcium supplementation for less than one month [Table/Fig-4].
Multi-nodular goiter with retrosternal extension (8 cm approximately).

Post-operative complications.
| Complications | No. of cases | Percentage |
|---|
| Haematoma | 0 | 0 |
| Seroma | 1 | 0.77% |
| Unilateral vocal cord palsy | | |
| Transient | 1 | 0.77% |
| Permanent | 2 | 1.5% |
| Hypocalcaemia | | |
| Temporary | 37 | 28.5% |
| Permanent | 3 | 2.3% |
Discussion
Total thyroidectomy has been indicated by most surgeons in view of the multi-centricity of thyroid cancer, incidence of 5 to 15 % local recurrence in the opposite thyroid lobe and higher incidence of complications in re-operative thyroid surgery [10–13]. Besides total thyroidectomy also facilitates follow-up with thyroglobulin, which would not be possible in the presence of normal thyroid tissue [10]. Though capsular dissection technique is the preferred method, many surgeons still prefer not to perform total thyroidectomy for benign thyroid swellings due to fear of associated complications.
The most common cause for iatrogenic recurrent laryngeal nerve injury is total thyroidectomy. It leads to either temporary or permanent damage. The various mechanisms of nerve injury include complete or partial transection, traction, contusion, crush injury, thermal damage while using electrocautery, misplaced ligature or compromised blood supply [14]. Delayed onset recurrent laryngeal palsy developing within few days after surgery is considered to be caused either by pressure effect of surrounding tissue oedema or haematoma [14]. There is increased chance of recurrent laryngeal nerve palsy when there is increased local scar formation as seen in thyroiditis, previous radiation and prior neck surgeries.
In the previous studies, temporary recurrent laryngeal nerve palsy was in the range of 4 to 5.8% while permanent palsy was in the range of 0 to 5% [15–17]. As per our study, we had a temporary recurrent laryngeal palsy of 0.77% and permanent palsy of 1.5%, which was well within the prescribed standards despite using bipolar electrocautery.
Temporary or permanent hypocalcaemia is a common complication following total thyroidectomy arising due to parathyroid insufficiency. The incidence of temporary hypocalcaemia can be upto 50% while permanent hypocalcaemia can be upto 4% [18–20]. In our study the incidence of temporary and permanent hypocalcaemia was 28.5% and 2.3% respectively.
The highly variable location of parathyroid glands along with variations in its blood supply creates significant difference in the incidence and degree of the parathyroid insufficiency [21]. There is increased chance of hypocalcaemia following auto-transplantation, extensive thyroid resection and ischemia of the parathyroid gland [22]. The risk factors pre-disposing to post-thyroidectomy hypocalcaemia include large volume goiter, recurrent goiter, retrosternal extension, advanced cancer and hyperthyroidism [22].
The main concern with the use of bipolar electrocautery has been the adequacy of ligation of vessels and the fear of thermal damage to recurrent laryngeal nerve and parathyroid vasculature. Only a single study by Tysome, attempted to prove the efficacy of bipolar cautery in thyroid surgery [23]. He found that patients undergoing hemithyroidectomies required fewer drains with reduced hospital stay. As per our study, we found that despite using bipolar electrocautery there were no cases of haematoma or bleeding and the complications like recurrent laryngeal nerve injury and hypocalcaemia were similar to conventional suture ligation technique. This also helped us in reducing our operating time and it serves as a cheaper alternative to the other expensive devices like ligasure and harmonic scalpel. Besides it helps in avoiding the complications associated with routinely practiced suture ligation that includes risk of knot slipping and suture granuloma [6]. This suture granuloma can pose a problem in patients with cancer as they can mimic tumour recurrence. As per the study by Manouras et al., they found that, both bipolar vessel sealer and harmonic scalpel had comparable results and hence, the choice between them need to be based on the surgeon’s preferences and experience [7].
The routine dissection of distal extra-laryngeal course of recurrent laryngeal nerve rather than the entire nerve course helps in avoiding devascularising the adjacent parathyroids and the nerve itself. Thus, capsular dissection helps in avoiding parathyroid insufficiency and damage to recurrent laryngeal nerve.
The lateral thermal spread and char formation associated with use of bipolar electrocautery can be minimized by the use of saline irrigation and lifting the vessels away from vital adjacent structures including recurrent laryngeal nerve before the application of electrocautery. The bipolar forceps was regularly cleared of char, so as to improve the accuracy of cauterization applied in the surgical field.
Limitation
The main limitation of this study was that, there was no control group. The complication rates are dependent on the skill and surgical experience of the operating surgeon. Better understanding of the anatomic variations of the recurrent laryngeal nerves helps in avoiding inadvertent damage to the recurrent laryngeal nerve.
Conclusion
Total thyroidectomy by capsular dissection technique has very low incidence of recurrent laryngeal nerve and parathyroid injury, as per our data. Hence, we recommend this technique over the dissection of the recurrent laryngeal nerve along it entire course. Besides total thyroidectomy offers immediate and permanent cure with no recurrences. The use of conventional bipolar electrocautery is time-saving and safe adjunct for thyroid surgeries and equally effective when compared to expensive devices like ligasure and harmonic scalpel.
[1]. Sakorafas GH, Historical evolution of thyroid surgery: From the ancient times to the dawn of the 21st centuryWorld J Surg 2010 34(8):1793-804. [Google Scholar]
[2]. Delbridge L, Total thyroidectomy: The evolution of surgical techniqueANZ J Surg 2003 73(9):761-68. [Google Scholar]
[3]. Dominello A, Guinea A, Reeve TS, Delbridge LW, Progressive increase in thyroid dysfunction after subtotal thyroidectomy for Graves diseaseAsian J Surg 2000 23:131-35. [Google Scholar]
[4]. Dror A, Salim M, Yoseph R, Sutureless thyroidectomy using electrothermal system: a new techniqueJ Laryngol Otol 2003 117(3):198-201. [Google Scholar]
[5]. Shen WT, Baumbusch MA, Kebebew E, Duh QY, Use of the electrothermal vessel sealing system versus standard vessel ligation in thyroidectomyAsian J Surg 2005 28(2):86-89. [Google Scholar]
[6]. Ecker T, Carvalho AL, Choe JH, Walosek G, Preuss KJ, Haemostasis in thyroid surgery: harmonic scalpel versus other techniques – A meta analysisOtolaryngol Head Neck Surg 2010 143(1):17-25. [Google Scholar]
[7]. Manouras A, Markogiannakis H, Koutras AS, Antonakis PT, Drimousis P, Lagoudianakis EE, Thyroid surgery: Comparison between the electrothermal bipolar vessel sealing system, harmonic scalpel, and classic suture ligationAm J Surg 2008 195(1):48-52. [Google Scholar]
[8]. Cordon C, Fajardo R, Ramirez J, Herrera MF, A randomized, prospective, parallel group study comparing the harmonic scalpel to electrocautery in thyroidectomySurgery 2005 137(3):337-41. [Google Scholar]
[9]. Siperstein AE, Berber E, Morkoyun E, The use of the harmonic scalpel vs conventional knot tying for vessel ligation in thyroid surgeryArch Surg 2002 137(2):137-42. [Google Scholar]
[10]. Shaha AR, Controversies in the management of thyroid noduleLaryngoscope 2000 110(2 Pt 1):183-93. [Google Scholar]
[11]. Giles Y, Boztepe H, Terzioglu T, Tezelman S, The advantage of total thyroidectomy to avoid reoperation for incidental thyroid cancer in multinodular goiterArch Surg 2004 139(2):179-82. [Google Scholar]
[12]. Efremidou El, Papageorgiou MS, Liratzopoulos N, Manolas KJ, The efficacy and safety of total thyroidectomy in the management of benign thyroid disease: A review of 932 casesCan J Surg 2009 52(1):39-44. [Google Scholar]
[13]. Agarwal G, Aggarwal V, Is total thyroidectomy the surgical procedure of choice for benign multinodular goiter? An evidence-based reviewWorld J Surg 2008 32(7):1313-24. [Google Scholar]
[14]. Chiang FY, Lu IC, Kuo WR, Lee KW, Chang NC, Wu CW, The mechanism of recurrent laryngeal nerve injury during thyroid surgery – The application of intraoperative neuromonitoringSurgery 2008 143(6):743-49. [Google Scholar]
[15]. Lo CY, Kwok KF, Yuen PW, A prospective evaluation of recurrent laryngeal nerve paralysis during thyroidectomyArch Surg 2000 135(2):204-07. [Google Scholar]
[16]. Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W, Advantages of recurrent laryngeal nerve identification in thyroidectomy and parathyroidectomy and the importance of pre-operative and post-operative laryngoscopic examination in more than 1000 nerves at riskLaryngoscope 2002 112:124-33. [Google Scholar]
[17]. Chiang FY, Wang LF, Huang YF, Lee KW, Kuo WR, Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerveSurgery 2005 137(3):342-47. [Google Scholar]
[18]. Ritter K, Elfenbein D, Schneider DF, Chen H, Sippel RS, Hypoparathyroidism after total thyroidectomy: Incidence and resolutionJ Surg Res 2015 197(2):348-53. [Google Scholar]
[19]. Seo ST, Chang JW, Jin J, Lim YC, Rha KS, Koo BS, Transient and permanent hypocalcaemia after total thyroidectomy: Early predictive factors and long-term follow-up resultsSurgery 2015 158(6):1492-99. [Google Scholar]
[20]. Bergamaschi R, Becouarn G, Ronceray J, Arnaud JP, Morbidity of thyroid surgeryAm J Surg 1998 176(1):71-75. [Google Scholar]
[21]. Park I, Rhu J, Woo JW, Choi JH, Kim JS, Kim JH, Preserving parathyroid gland vasculature to reduce post-thyroidectomy hypocalcaemiaWorld J Surg 2016 40(6):1382-89. [Google Scholar]
[22]. Abboud B, Sargi Z, Akkam M, Sleilaty F, Risk factors for post-thyroidectomy hypocalcaemiaJ Am Coll Surg 2002 195(4):456-61. [Google Scholar]
[23]. Tysome JR, Hassan R, Davis J, Standard bipolar diathermy forceps vessel ligation is safe in thyroidectomyJ Eur Arch Otorhinolaryngol 2009 266:1781-86. [Google Scholar]