The incidence of Kyphoscoliosis is two to three percent in general population. Any degree of deformity in either structure or alignment tends to have some sequelae like cardio-respiratory morbidity, neurological symptoms, loss of balance, cosmetic unacceptability or just back pain. Surgical correction of the deformity might be required for prevention or reversal of the above effects and to have an acceptable quality of life. Traditionally, surgical intervention for patients with a spinal deformity has been considered for cosmetic benefits, but surgical intervention can alter the lung physiology or volumes and in turn lead to increase in physical capacity and exercise tolerance. However, there are also other indications for surgery such as risk of severe compromise in lung function tests due to a severe spinal deformity even when the patients do not have any cosmetic concerns [1,2]. Patients with severe deformity tend to have a compromised cardiovascular status leading to a limited or restricted lifestyle causing a decline in the physical capacity and exercise tolerance [3-7]. Surgical intervention in cases of spinal deformity is mainly considered for cosmetic reasons. Surgical correction of the deformity can also lead to changes in the physiological parameters, in turn leading to an improvement in the physical capacity, exercise tolerance and the overall quality of life. A study is necessary to assess whether surgical correction of a spinal deformity can reverse the effects of spinal deformity on exercise tolerance and also quantify the changes in exercise tolerance after a surgical intervention in cases of spinal deformity. A study is also needed to determine whether the parameters used for assessment of exercise tolerance can act as indications for surgical intervention in patients with spinal deformity.
Materials and Methods
A series of 30 patients with spinal deformity who underwent/required surgery for deformity correction (spinal deformity corrective procedures +/- instrumentation +/- thoracoplasty/costoplasty) from January 2012 to November 2014 were studies. The study was an interventional study where all the patients acted as their own controls before they were treated with a surgical intervention for deformity correction. The study hypothesized that surgical intervention in cases of spinal deformity did not lead to improvements in breath holding time, modified Borg scores and six-minute walk test score. All patients were operated by a single surgeon and reviewed independently. The ethics committee approved the study plan and an informed consent was obtained from all the patients before enrolment into the study. Inclusion criteria under the study were a diagnosis of scoliosis with increasing curve in a growing child, severe deformity (greater than 50 degrees) with asymmetry in adolescents, diagnosis of kyphosis greater than 75 degrees, thoracic lordosis, significant scoliosis related cardiorespiratory dysfunction, significant cosmetic deformity and pain not alleviated by conservative treatment. Patients included belonged to Lenke classification curve type-1, type-2 and type-3. Patients with other Lenke types involving lumbar and thoraco-lumbar regions which do not affect the lung volumes and physiology to a similar qualitative or quantitative extent were excluded from the study. The study group homogeneity was maintained and consisted of patients with a thoracic spinal deformity alone. The patients with congenital, infective or other pulmonary pathology (chronic obstructive pulmonary disease/asthma), congenital or other cardiac pathology like cardiomyopathy, infective/ischemic cardiac pathology, neurological deficit and muscular dystrophy (leading to respiratory/other muscle weakness impeding physical activity) were excluded from the study.
All patients were pre-operatively investigated with x-rays of the spine (anteroposterior and lateral views) for the type of curve and the cobb angle and AVBR (Apical Vertebral Body Ratio). Clinical tests for pre-operative breath holding time in number of seconds (after full inspiration), modified Borg scores [Table/Fig-1] [8,9], six-minute walk test scores (heart rate, respiratory rate, maximum distance walked) [10,11] were recorded. The patients were put on intensive respiratory exercises with an incentive spirometer and balloon bladder; suspension exercises for the spine to increase the flexibility of the spinal curve [12]. The patients were started on high protein diet and oral iron supplements to replenish the body stores needed for good tissue healing.
| Rating | Intensity of Sansation |
|---|
| 0 | No Symptoms |
| 0.5 | Very, very slight sensation of symptoms |
| 1 | Very Slight |
| 2 | Slight |
| 3 | Moderate |
| 4 | Somewhat Severe |
| 5 | Severe |
| 6 | |
| 7 | Very Severe |
| 8 | |
| 9 | Very, Very Severe |
| 10 | Maximal |
Among the 30 patients, 17 patients were treated with Ponte’s release followed by posterior instrumentation with pedicle screws and connecting rods. Four patients had an additional thoracoplasty. Three patients were treated with Ponte’s release followed by posterior instrumentation with pedicle screws and growing rods. Six patients were treated with excision of the abnormal congenital vertebra followed by posterior instrumentation with pedicle screws and connecting rods. All patients were operated through a posterior midline approach. Patients were started with their post-operative mobilization, two weeks after the surgery.
They were started on back flexion, extension exercises and paraspinal muscle strengthening exercises. Intensive respiratory exercises were continued in the post-operative period with the incentive spirometer and balloon bladder. The patient’s nutritional supplements were continued post-operatively and discharged after one month. The patients were followed up at three, six and twelve months. The post-operative investigations done at the time of discharge (one month), three, six and twelve months post-operatively were X-rays of the spine and clinical tests. Before enrolment into and during the study, the patients were counselled about the importance of regular follow-up visits and post-operative investigations. None of the patients enrolled into the study were lost to follow-up.
Statistical Analsis
The results were analysed and tested for significance using Student’s T-test for parametric data (paired and unpaired as appropriate) and Wilcoxon signed rank test for nonparametric data.
Results
Among the 30 patients, 23 patients belonged to Lenke curve classification [13] Type-1 (Five 1AN, One 1A+, Four 1A-, Eight 1BN, One 1B+, One 1CN, Three 1C+), four patients belonged to Type-2 (Two 2AN, One 2B+, One 2CN) and three patients belonged to Type-3 (Two 3A+, One 3B+) [Table/Fig-2]. The majority of the cases (20) were diagnosed with idiopathic scoliosis. Six patients were diagnosed with congenital scoliosis and four were diagnosed to be due to neurofibromatosis. The mean cobb angle on anteroposterior view was 65.1 degrees (the highest being 122 degrees and the lowest being 40 degrees). The mean cobb angle on lateral view was 36.8 degrees (the highest being 70 degrees and the lowest being 10 degrees). The mean age of the patients in our study was 15.3 years. The youngest patient in our study was eight-year-old and the oldest patient was 22-year-old. Three patients belonged to less than 10-years of age-group, 19 belonged to the age-group between 11-15 years, five belonged to the age-group between 15-20 years and three patients belonged to age-group of greater than 20 years. Twenty-one patients were females and nine patients were males with a female to male ratio of 2.3:1. The post-operative test results were compared with the pre-operative test results and every patient acted as his/her own control.
Distribution of patients according to Lenke classification.
| Type of curve Lenke classification | No. of patients | Percentage |
|---|
| Type 1 | 23 | 76.7 |
| 1A | 10 | 33.3 |
| 1B | 9 | 30 |
| 1C | 4 | 13.3 |
| Type 2 | 4 | 13.3 |
| 2A | 2 | 6.7 |
| 2B | 1 | 3.3 |
| 2C | 1 | 3.3 |
| Type 3 | 3 | 10 |
| 3A | 2 | 6.7 |
| 3B | 1 | 3.3 |
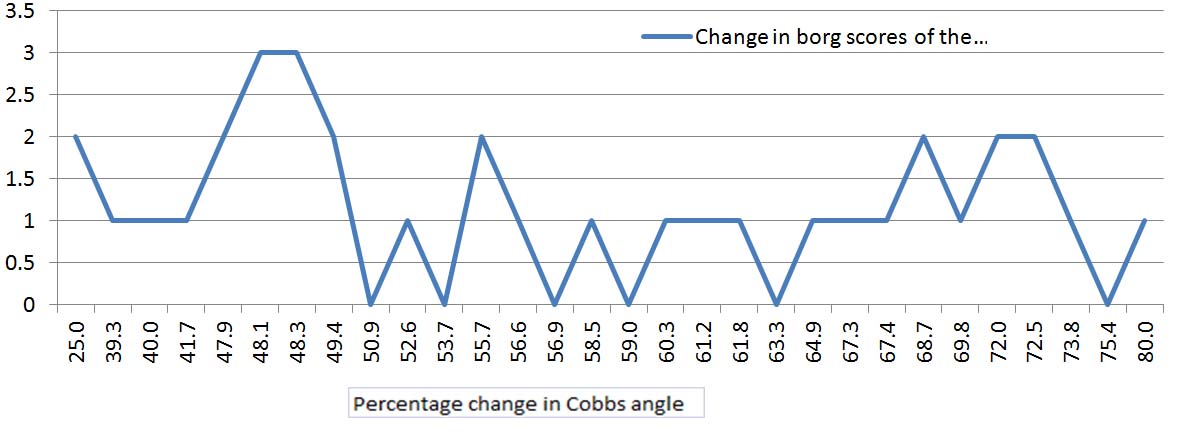
The average correction of the curve, after surgery, achieved on anteroposterior x-ray view was 45.7 degrees (the highest being 72 degrees and the lowest being 30 degrees). The study showed no correlation between changes in modified Borg scores and the percentage correction in the cobb angle [Table/Fig-3].
Changes in modified borg scores of the patients plotted against increasing percentage change in Cobb’s angle.
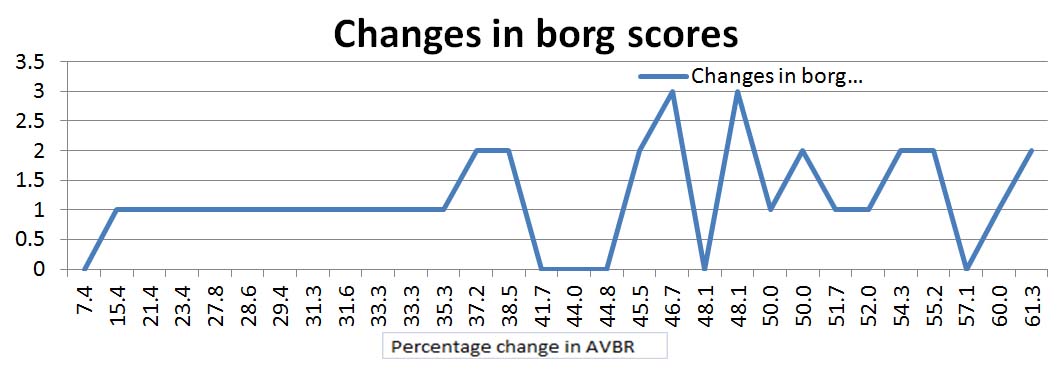
The study showed a mean decrease in percentage change of AVBR of 40 percent (p-value=0.001) after the surgery. However, there was no correlation between the percentage change in AVBR and the percentage correction in cobb angle [Table/Fig-4].
Changes in modified borg scores plotted against increasing changes of percentage AVBR change.
Breath holding capacity (p-value=0.001) showed a significant improvement at 12 months of follow-up, after an initial decline in the immediate post-operative period. The baseline pre-operative levels were regained by three to six months of follow-up.
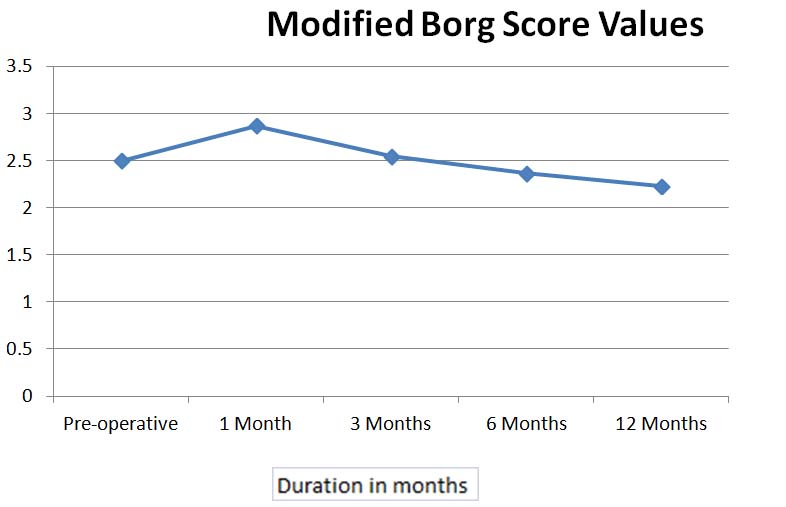
The modified Borg scores showed a significant (p-value=0.012) improvement with patients scoring lower levels of exertion at the twelfth month post-operatively. However, the patients showed a worsening in modified Borg scores during the immediate post-operative period. The parameters were back to pre-operative levels by three months of follow-up [Table/Fig-5].
Modified Borg scores plotted against duration of follow-up.
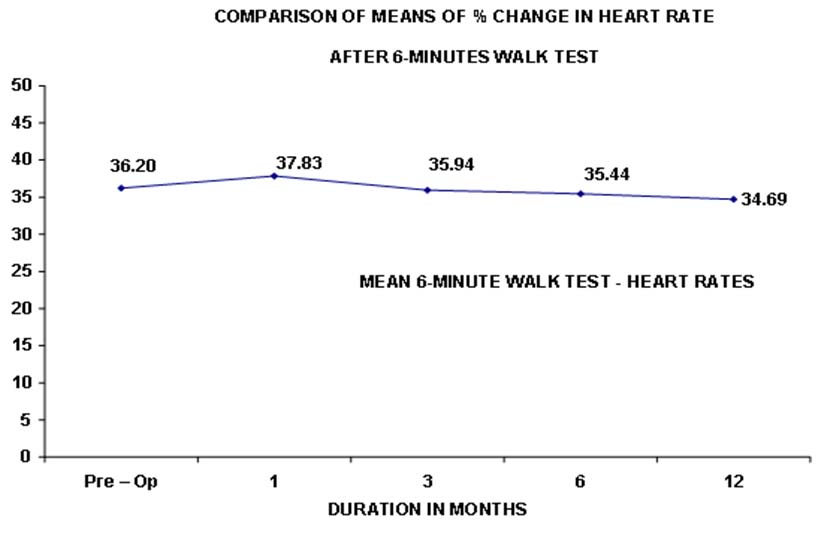
Similar findings were noted with percentage changes in heart rate after a six-minute walk test. The mean percentage change in post-test heart rate was lower during the follow-up at the third, sixth and twelfth month post-operatively, but the results were significant only at twelfth month (p-value = 0.014). The mean percentage change in post-test heart rate was more during the immediate post-operative period [Table/Fig-6].
Percentage change in heart rate after 6 minute walk test plotted against duration of follow-up.
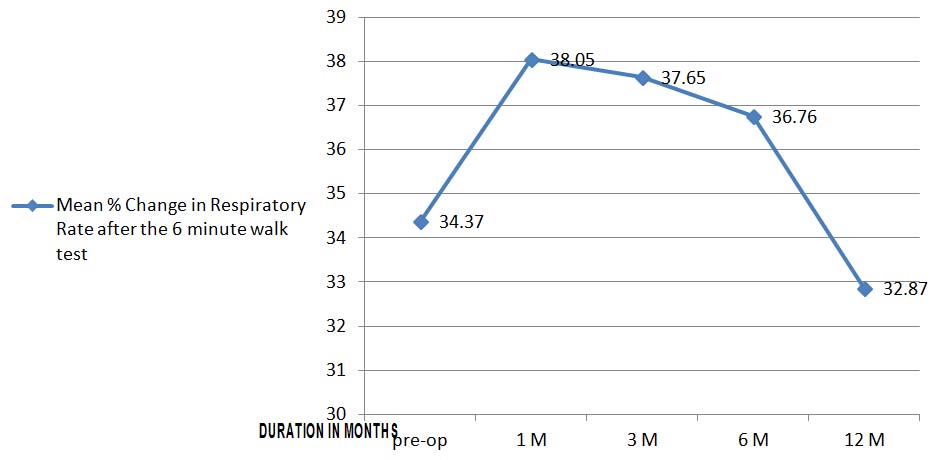
The mean percentage change/increase in respiratory rates after the six-minute walk test was lower at 12 months follow-up. However, the results for the percentage change in respiratory rates after the six-minute walk test were not found to be significant (p-value = 0.28) [Table/Fig-7] even at 12 months.
Mean percentage change in respiratory rate plotted against duration of follow-up.
The maximum distance walked after the six-minute tests also showed a significant (p-value = 0.01) improvement at 12 months of follow-up, with an average increase of 50-100 meters.
Discussion
The patients showed significant improvement in all the parameters used to assess the physical capacity and exercise tolerance at 12 months of follow-up. However, this was not before an initial decline in the immediate post-operative period. This was possibly due to pain in the post-operative period and physical deconditioning when the patient was on minimal mobilization for almost three weeks. The decline in breath holding capacity, modified Borg scores and the six-minute walk test scores (change in heart rates, respiratory rates and maximum distance walked) corresponds to a decline in the pulmonary function tests seen in studies like, "Effect of scoliosis surgery on lung function in the immediate post-operative period" [14-16]. These studies found a decrease in pulmonary function tests in the immediate post-operative period, persisting even up to two years post-operatively. These studies did not assess the physical capacities or exercise tolerance in their patients. The patients in our study, however, regained their baseline values by three to six months post-operatively and no long-term adverse effects of surgical correction were found, with patients showing better exercise tolerance scores by the twelfth month of follow-up.
The patients were put on respiratory exercises and intensive physical therapy, which are important confounding factors to the above results of our study. Respiratory exercises and physical conditioning are known to bring about an improvement in exercise tolerance [12, 17]. Further studies are necessary to see whether surgery alone can give rise to the above results.
The study subjects were divided into two groups. The first group of patients (13) with less than 60 degrees of cobb angle and the second group of patients (17) with more than 60 degrees of cobb angle. The differences between the means of parameters (during the pre-operative period and at the twelfth month post-operatively) were compared among the two groups. All the parameters showed similar findings in both the groups, with improvements slightly greater in the group with above 60 degrees of cobb angle. These differences were not significant, except for the differences in means for breath holding capacity (p-value = 0.015) and the percentage change in respiratory rate after six-minute walk test (p-value = 0.049). This suggests that breath holding capacity and the percentage change in respiratory rate after six-minute walk test can be improved with surgical correction of the deformity, especially in cases with greater than 60 degree cobb angle. The improvement in cases with less than 60 degree cobb angle was not to an extent seen in cases with greater than 60 degree cobb angle [Table/Fig-8].
Mean change from pre-operative period to twelve months follow-up for all parameters.
| Parameters | Mean Change from pre-operative period to 12 months follow-up (x̄ SD) | p-value |
|---|
| ≤ 60 Cobbs angle (N = 13) | > 60 Cobbs angle (N = 17) |
|---|
| Breath holding capacity | -02.77±01.48 | -04.71±02.62 | *0.015 |
| Borg scores | 00.92±00.49 | 01.35±01.00 | 0.133 (NS) |
| 6 Minute walk test - % change in heart rate | 02.15±03.33 | 01.03±03.09 | 0.354 (NS) |
| 6 Minute walk test -% change in Respiratory rate | -01.53±07.03 | 03.82±07.12 | *0.049 |
| 6 Minute walk test - Max distance walked | -42.31±34.44 | -55.88±46.38 | 0.365 (NS) |
Studies have been done on the effect of spinal deformity on exercise tolerance [5-7]. These studies have assessed the physical capacity/exercise tolerance/work capacity in patients with spinal deformity. Among the three studies, the study by Menon B et al., has used the six-minute walk test to assess exercise tolerance in the patients with spinal deformity [5]. The other two studies have assessed work capacity measured using an incremental cycle test and the cardiorespiratory response to exercise; Physical Work Capacity 170 (PWC170) test on a cycle ergometer based on two 5-min submaximal physical effort events. These studies have successfully determined an association between spinal deformity and a decreased exercise tolerance and also determined the usefulness of their respective exercise-tolerance-assessment parameter. However, unlike our study, none of the previous studies have attempted to determine the effect of surgical intervention on the reversibility of exercise tolerance in patients with spinal deformity.
Limitation
There were few limitations of the study. Firstly, the study included a heterogeneous group of patients differing in age, sex, type and severity of the curve which makes it difficult to postulate the results of the study to any one type of spinal deformity or a particular group of patients. A well-designed study, stratifying different groups of patients, is required to determine the effects of surgical intervention in different age-groups, sex-groups and groups of patients with differing types/severity of the curve. Secondly, the patients were put on respiratory exercises and intensive physical therapy, which are important confounding factors to the above results of our study. Larger studies with control groups, treated with physiotherapy and respiratory exercises alone are required to determine whether surgery alone (compared to respiratory exercises, physical conditioning, boosting self-confidence, image counselling) can bring about the sustained and effective results in these patients. Larger studies are also required to investigate whether the decreased functional ability or a particular parameter assessed in the study can act as a more solid indication for surgery.
Conclusion
The management protocol followed improves the cosmetic appearance and balance in the patients. We conclude that surgical correction of the deformity improves exercise tolerance in patients with spinal deformity. Modified Borg scores and six-minute walk test scores are effective tools for assessment of changes in exercise tolerance and physical capacity in patients with spinal deformity undergoing surgical intervention.
The improvements were more in patients with higher grades of severity, but there was no correlation between the degree of correction and the change in parameters assessed. The physical deconditioning in patients with kyphoscoliosis due to lack of exercises, lesser self-confidence, poor self-image might have been major contributors to the deficiencies. Regular physical conditioning exercises, back strengthening exercises, intensive respiratory exercises and counseling to build their self-image form an integral part of management in such patients.