Verruciform Xanthoma (VX) is a rare lesion of the oral cavity. Histologically, it is characterized by papillary or verrucous proliferation of squamous epithelium and numerous foam cells. VX arising in the tongue is comparatively rare, as most cases of VX in oral cavity occur in gingiva. A 65-year-old woman was referred to our clinic with a mass on the left side of the tongue. The lesion was yellowish, and its surface was granulated. The patient had neither tenderness nor any symptoms. The lesion was clinically diagnosed to be a benign tumor, and hence, biopsy was performed, according to which it was diagnosed as hyperparakeratosis. Based on this diagnosis, the tumor was excised under general anesthesia. Histopathologically, the tumor consisted of stratified squamous epithelium with parakeratosis and elongated rete ridges. Aggregation of foam cells was observed between and under the rete ridges. From these features, a diagnosis of VX was made. The patient has had no local recurrence as of three years post-operatively.
Foam cell, Hyperparakeratosis, Verrucous proliferation
Case Report
A 65-year-old Japanese woman was referred to our clinic with a mass on the left side of the tongue. She had a history of hypertension, hyperlipidemia and diabetes mellitus. She had full dentures of the upper and lower jaws made around four years earlier. The mandibular denture was inadequate, with evidence of desorption, but the patient have not had a dental check-up. Intra-oral examination showed a yellowish exophytic lesion on the left lateral edge of the tongue. The lesion was well-demarcated and soft, 15×10mm in diameter and clinically asymptomatic [Table/Fig-1]. Lymph nodes were not palpable. No other intra-oral or skin lesions were identified. A provisional diagnosis of a benign tumor was made. Incisional biopsy was performed under local anesthesia, and the result was a hyperkeratotic tumor. Because the patient’s vomiting reflex was strong, the whole lesion was excised under general anesthesia.
Intra-oral tumor findings at the initial examination. A 15x10mm tumor with yellowish exophytic growth is observed in the left lateral edge of the tongue.

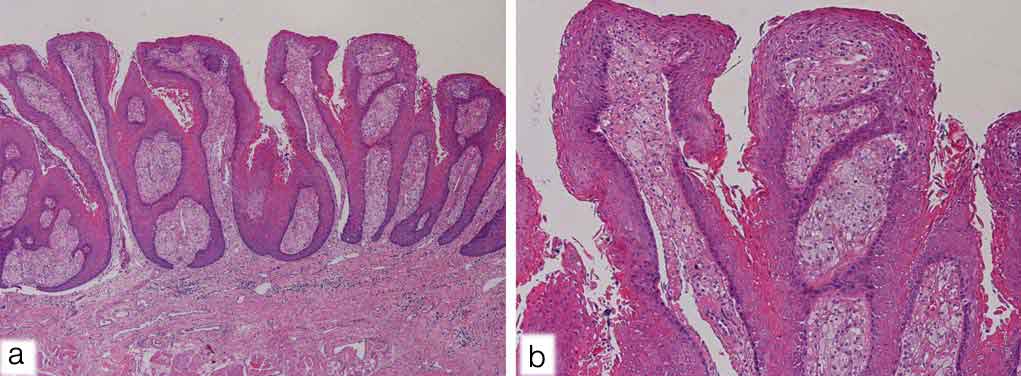
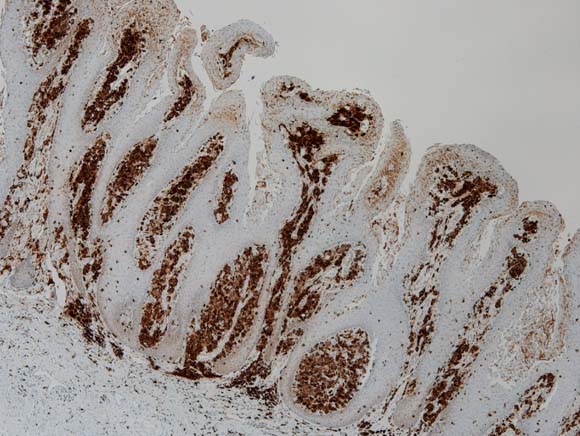
On histopathological examination, the hematoxylin and eosin stained section showed papillary proliferation of the stratified squamous epithelial cell layer, which was covered with a hyperkeratotic layer. Numerous foam cells were seen in the connective tissue papillae between epithelial ridges. These cells showed clear to eosinophilic cytoplasm with eccentrically placed nuclei. Mild to moderate inflammatory cell infiltration consisted mainly of lymphocytes in the underlying connective tissue stroma [Table/Fig-2]. On immunohistochemical staining for CD68, the foam cells were positive [Table/Fig-3]. Based on these histopathological features, a diagnosis of Verruciform Xanthoma (VX) was made.
Epithelial hyperplasia with parakeratosis and elongated rete pegs. There is an abundance of foam cells in the connective tissue papilla [H&E a): x 40) and b): x 100].
Foam cells with strong cytoplasmic CD68 immunostaining (IHC stain x 40).
After the lesion was totally resected, the surgical site underwent normal secondary healing. The patient had no complications, and there was no evidence of recurrent disease during the three year follow-up period.
Discussion
Verruciform Xanthoma (VX) is a rare lesion of the oral cavity. This disease was first described as a rare benign lesion by Shafer in 1971 [1]. Histologically, it is characterized by papillary or verrucous proliferation of squamous epithelium and numerous foam cells. The most frequently encountered site in the oral cavity is the gingiva. VX arising in the tongue is comparatively rare. In 2003, Philipsen HP et al., revealed 282 patients with VX of the oral cavity reported by an extensive search of the literature. The tumor occurred in the gingiva in 162 patients (57.4%), tongue in 29 (10.2%), hard palate in 28 (9.9%), buccal mucosa in 19 (6.7%), floor of the mouth in 13 (4.6%), soft palate in 9 (3.1%), and lower lip in 8 (2.8%) [2].
Zagarelli DJ et al., suggested that local trauma and inflammation lead to epithelial entrapment, and the cause of lipid-containing macrophage accumulation is epithelial degeneration. The products of epithelial breakdown elicit an inflammatory response that is manifested by a predominant neutrophilic infiltrate in the epithelium and a subsequent release of lipid material through the epithelium that is finally scavenged by the macrophages [3]. CD68 is a cell marker confirming the possible role of macrophages in the formation of foam cells [2]. In the present case, the foam cells showed strong CD68 immunoreactivity. Ide F et al., suggested some possible oral aetiologic agents, such as a wet microenvironment, periodontal pathogens, mechanical stimuli, tobacco, alcohol, drugs, sensitizing or allergic substances, foodstuffs, and dental materials [4]. In the present case, the inflammatory reaction from the chronic mechanical irritation that resulted from insertion of an inadequate denture over a long period caused epithelial papillary growth, and it seemed that foam cells accumulated in connective tissue under epithelial ridges.
The clinical differential diagnosis of VX includes squamous papilloma, verruca vulgaris, fibroma and verrucous carcinoma [2]. In the tongue, VX is clinically diagnosed as papilloma in many cases. Therefore, examination of a biopsy specimen may be the only way to distinguish one from the other.
Associations between VX and systemic diseases, such as diabetes mellitus, hyperlipidemia, and graft versus host disease have been reported [2,5]. In the present case, diabetes mellitus and a history of hyperlipidemia were present. However, there has been, in general, no definite correlation between VX and systemic diseases.
We did a systematic search of PubMed (January, 1971, to December, 2015) and Ichushi-Web (January, 1971, to December, 2015). The medical subject heading “Xanthoma” was combined with the following terms: “oral” and “tongue”. Relevant articles, abstracts, and review articles were selected and reviewed. As a result, a world-wide literature survey revealed a total of 40 cases with VX of the tongue, including one case from our own files [Table/Fig-4]. Among the 25 non-Japanese cases reviewed the following characteristics features were marked:
Clinical characteristics of patients with the tongue VX: Non-Japanese vs. Japanese.
| Non-Japanse (n=25) | Japanse (n=15) |
|---|
| Median age (range), years | 38.1 (2-76)a | 52.9 (21-80) |
| Sex, n(%) |
| Male | 11 (50)b | 3 (20) |
| Female | 11 (50)b | 12 (80) |
| Median size (range) mm | 11.6 (1.5-35)c | 10.2 (3-20) |
| Location, n(%) |
| Inferior surface/Lateral edge of the tongue | 15 (65)d | 15 (100) |
| Dorsum of the tongue | 8 (35)d | 0 (0) |
a: n=21, b: n =22, c: n=20, d: n=23
The total number of cases which recorded age were 21, of which the mean age was 38.1 years (age range: 2-76 years).
The total number of cases which recorded gender were 22, of which 11 were males (50.0%) and 11 females (50.0%), giving a male: female ratio of 1:1.
The total number of cases which recorded size were 20, of which the greatest mean dimension of the lesions was 11.6mm (range, 1.5-35mm).
The total number of cases which recorded location were 23, of which fifteen (65.2%) were localized to the lateral edge [2, 5-10].
Kiyokawa T et al., found 14 Japanese tongue VX cases reported in the literature, and they showed the following characteristics [5].
The mean age was 52.1 years (age range: 21-80 years).
Three cases were found in males (21.4%), and 11 in females (78.6%), giving a male: female ratio of 1:3.6.
Most were protruded lesions with color varying, being white, yellowish, or reddish pink, and the greatest mean dimension of the lesions was 9.8mm (range, 3-20mm).
All cases occurred in the inferior surface or lateral edge of the tongue, and there were no reports involving the dorsum of the tongue with slight chronic irritation by teeth and dentures.
Various diseases, such as hypertension, arteriosclerosis, heart disease, and a malignant tumor, were found on the medical history, but diabetes mellitus, hyperlipidemia and liver disease were not found.
In comparison of clinical characteristics, the Japanese mean age and female ratio were higher than the non-Japanese. As for location, our search of the literature revealed no reports of VX arising in the dorsum of the tongue in Japanese patients. In the present case, the lesion was located in the lateral edge of the tongue, with an average size of 15×10mm. However, the patient had diabetes mellitus and hyperlipidemia.
VX is usually treated by conservative excision. Recurrence of oral VX is extremely rare, since only five cases have been reported [3,11-14], all localized to the gingiva. If chronic mechanical irritation seems to be a cause, as in the present case, it is necessary to remove the cause to prevent recurrence.
Conclusion
VX arising on the tongue is comparatively rare. Because it is difficult to clinically differentiate between VX and other diseases involving verruciform surfaces on tongue, the clinical diagnosis may be challenging. Therefore, we seem that this report is useful to better understand the clinical features and pathogenesis of VX.
a: n=21, b: n =22, c: n=20, d: n=23
[1]. Shafer WG, Verruciform xanthomaOral Surg 1971 31:784-9. [Google Scholar]
[2]. Philipsen HP, Reichart PA, Takata T, Ogawa I, Verruciform xanthoma – Biological profile of 282 oral lesions based on a literature survey with nine new cases from JapanOral Oncol 2003 39:325-36. [Google Scholar]
[3]. Zegarelli DJ, Zegarelli-Schmidt EC, Zegarelli EV, Verruciform xanthoma: Further light and electron microscopic studies, with the addition of a third caseOral Surg Oral Med Oral Pathol 1975 40:246-56. [Google Scholar]
[4]. Ide F, Obara K, Yamada H, Mishima K, Saito I, Kusama K, Cellular basis of verruciform xanthoma: Immunohistochemical and ultrastructual characterizationOral Dis 2008 14:150-57. [Google Scholar]
[5]. Kiyokawa T, Shigematsu H, Oku Y, Hoshino M, Kikuchi K, Sakashita H, A case of verruciform xanthoma occurring in a patient with multiple stomatitisJ Jpn Stomatol Soc 2014 63(2):226-32. [Google Scholar]
[6]. Visintini E, Rizzardi C, Chiandussi S, Biasotto M, Melato M, Di Lenarda R, Verruciform xanthoma of the oral mucosa. Report of a caseMinerva Stomatol 2006 55(11-12):639-45. [Google Scholar]
[7]. Yu CH, Tsai TC, Wang JT, Liu BY, Wang YP, Sun A, Oral verruciform xanthoma: A clinicopathologic study of 15 casesJ Formos Med Assoc 2007 106(2):141-47. [Google Scholar]
[8]. Mete O, Kurklu E, Bilgic B, Beka H, Unur M, Flat-type verruciform xanthoma of the tongue and its differential diagnosisDermatol Online J 2009 15(9):5Available from http://escholarship.org/uc/item/0vk3d0bw [Accessed on 15/9/2009] [Google Scholar]
[9]. Shahrabi Farahani S, Treister NS, Khan Z, Woo SB, Oral verruciform xanthoma associated with chronic graft-versus-host disease: A report of five cases and a review of the literatureHead Neck Pathol 2011 5(2):193-98. [Google Scholar]
[10]. Joshi R, Ovhal A, Verruciform xanthoma: Report of Five CasesIndian J Dermatol 2012 57(6):479-82. [Google Scholar]
[11]. Nowparast B, Howell FV, Rick GM, Verruciform xanthoma. A clinicopathologic review and report of fifty-four casesOral Surg Oral Med Oral Pathol 1981 51:619-25. [Google Scholar]
[12]. Neville B, The verruciform xanthoma. A review and report of eight new casesAm J Dermatopathol 1986 8:247-53. [Google Scholar]
[13]. Iamaroon A, Vickers RA, Characterization of verruciform xanthoma by in situ hybridisation and immunohistochemistryJ Oral Pathol Med 1996 25:395-400. [Google Scholar]
[14]. Ryu da J, Lee SH, Yuk JI, Kim HJ, Huh JK, Park KH, Verruciform xanthoma of the palatal gingiva: A report of two casesJ Korean Assoc Oral Maxillofac Surg 2013 39(6):292-96. [Google Scholar]