Non-Infiltrating Angiolipoma of Floor of Mouth-A Rare Case Report and Literature Review
Sanat Kumar Bhuyan1, Ruchi Bhuyan2, Priyanka Debta3, Fakir Mohan Debta4
1 Professor and Head of Department, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bhubaneswar, Odisha, India.
2 Professor, Department of Oral Pathology and Microbiology, Institute of Dental Sciences, Bhubaneswar, Odisha, India.
3 Reader, Department of Oral Pathology and Microbiology, Institute of Dental Sciences, Bhubaneswar, Odisha, India.
4 Assistant Professor, Department of Oral Medicine, SCB Government Dental College, Cuttack, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanat Kumar Bhuyan, Professor and Head of Department, Department of Oral Medicine and Radiology, Institute of Dental Sciences, Bhubaneswar-751015, Odisha, India.
E-mail: drsanatkumar68@gmail.com
Angiolipoma, a subtype of lipoma is a benign tumour in which adipose tissue and vascular component are intermingled. The tumour occurs commonly in the trunk and extremities and very rarely seen in maxillofacial region. Here we report a case of Non-Infiltrating Angiolipoma (NIAL) in floor of mouth which is the second case to be reported in literature to the best of our knowledge. We have reviewed all NIAL cases involving the oral cavity from 2008 to 2016 and found 12 cases of NIAL and assessment was made according to age, sex, site and size of lesion for better understanding of the lesion and its nature.
Benign tumour, Fatty tissue, Oral cavity, Rare lesion
Case Report
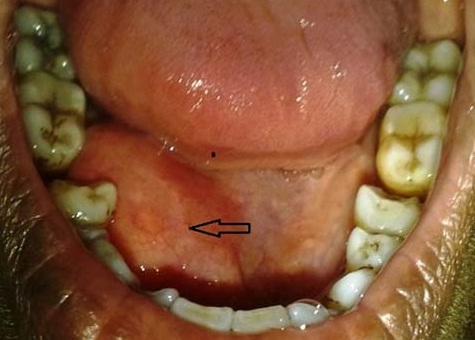
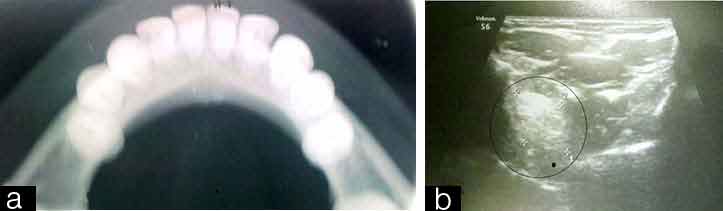
A 28-year-old female patient reported with a chief complaint of a large swelling in the right side of floor of the mouth. The swelling started 3 years back as a small one and gradually increased to attain the present size. The patient also reported difficulty in eating and phonation. On clinical examination, extraorally there was diffuse swelling in the submandibular region. Intraorally swelling was soft in consistency, smooth surface, mobile, fluctuant, and non-reducible, non-tender on palpation and measuring approximately 3x3.5cm in size. No overlying mucosal changes and ulceration were noticed [Table/Fig-1]. So, a provisional diagnosis of soft tissue lipoma with ranula as differential diagnosis was made. Medical history was not significant and blood investigations were within normal limits. Occlusal radiograph revealed absence of any radiopaque structure like salivary stones or any calcified mass and no bony involvement [Table/Fig-2a]. USG revealed presence of a mass measuring approximately 3x3cm in diameter [Table/Fig-2b]. MRI revealed a well encapsulated lesion (26x23x16mm) in the right paramedian floor of the mouth with T1W/T2W hyperintense lesion with complete attenuation in fat saturated image [Table/Fig-3a-c]. All these diagnostic investigations suggested a benign non-infiltrating lesion of soft tissue.
Intraoral view-A well defined swelling present in the right side of the floor of the mouth.
(a) Occlusal radiograph no bony involvement; (b) USG shows an echogenic mass present in the right submandibular region.
(a) T1 axial view in MRI shows an hyper intense mass in the right submandibular region; (b) T2 axial view in MRI shows an hyper intense mass in the right submandibular region; (c) T2 saggital view in MRI shows an hyper intense mass in the right submandibular region.

No fluid could be detected on aspiration so with the written consent of patient excisional biopsy was planned under local anaesthesia. A longitudinal incision was made over the mucosa covering the tumour, and aspiration was done again but no fluid could be detected and the lesion was resected completely [Table/Fig-4a-c]. Then mucosal layers were closed together with absorbable sutures. Macroscopic view of surgically excised specimen was yellowish in colour, soft in consistency and of size approximately 3.5x3cms [Table/Fig-5a].
(a) Intra-operative picture shows the mass beneath the mucosa after the incision; (b) FNAC of the lesion shows no fluid; (c) The intra-operative picture shows that the mass is not attached to the underlying structure.

(a) Shows the tumour mass after excision; (b) Healed lesion after one month.
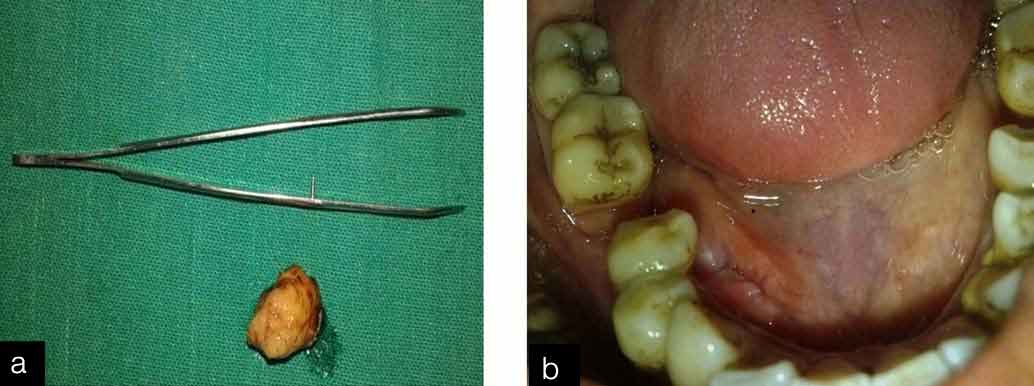
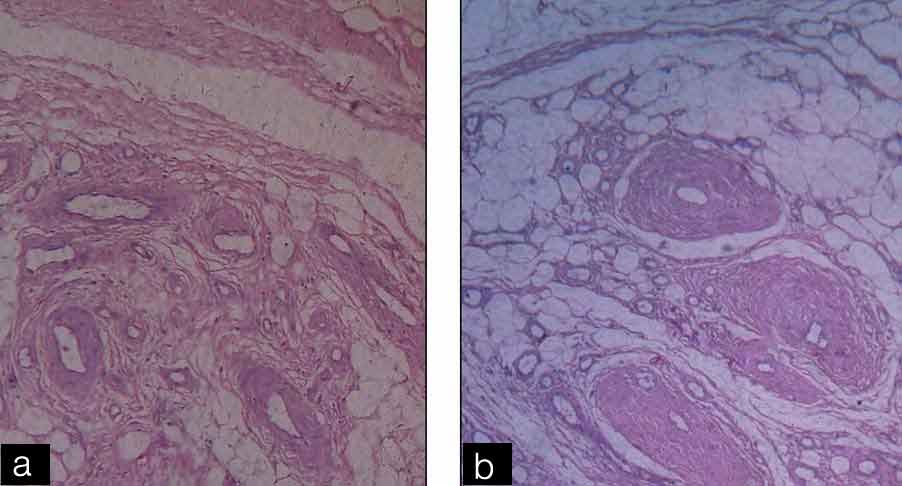
Microscopic view in H&E stained section under low magnification revealed an encapsulated tumour mass consisting of adipose tissue separated by branched vascular network. Thick walled blood vessels were present at the periphery of the tumour mass. Higher magnification revealed numerous mature adipocytes and variable sized, thick walled endothelial lined blood vessels. Few areas showed presence of fibrinous microthrombi and dilated blood vessel. A diagnosis of Non-Infiltrating Angiolipoma (NIAL) was made [Table/Fig-6a,b]. Patient recovered without any complication after surgery. No evidence of recurrence was seen after one month of surgery [Table/Fig-5b].
(a) Encapsulated tumour mass consist of adipose tissue intermixed with thick walled blood vessel (H&E stain, X10 view); (b) Sheets of mature adipose tissue, vascular element containing thrombi and the congested vessels shows no cellular atypia (H&E stain, X40).
Discussion
Lipomas are relatively exceptional benign mesenchymal tumours that originate from mature adipocytes [1]. Incidence of lipoma reported in head and neck region is 15-20% of which 1-4% affects the oral cavity [2]. The categorization for benign lipoma includes, classic lipoma and lipoma variants (e.g., angiolipoma, osteolipoma, chondroid lipoma, myolipoma, spindle cell lipoma, hamartomatous lesions, diffuse lipomatous proliferation and hibernoma) [3]. Angiolipoma (AL) accounts for 6-17% of all lipomas [4]. It was first described as a distinct entity by Bowen. AL is a relatively rare tumour of head neck region, although it occurs more commonly in the forearm and trunk region. This tumour has been rarely reported in oral cavity [5]. They are benign mesenchymal tumours made up of mature lipocytes and blood vessels. Gonzalez-Crussi et al., suggested two histologic types of AL-Infiltrating and non-infiltrating. NIAL are encapsulated; whereas, infiltrating angiolipomas lack this capsule [3]. To the best of our knowledge, it has been reported only once in floor of mouth by Park JY et al., in 2008 [6]. Here we present a case of NIAL in floor of mouth with review of all published cases of NIAL involving oral cavity since 2008-2016.
Variants of lipoma are much rare and differ from ordinary lipoma by characteristic clinical and microscopic features [7]. Lipomas are most commonly seen in young male patients in their second or third decades of life. They can be multiple and are most commonly seen on forearm followed by the trunk and upper arm. When seen in the oral cavity, it has been noted on the cheek, lip, palatal mucosa and buccal mucosa being the most common site [8]. Arenaz Bua J et al., in 2010 reviewed the cases of AL from 1976-2007 and they found 26 cases of NIAL among which 14 cases were from oral cavity [9]. We reviewed NIAL in oral region from 2008-2016 and found 12 cases among which only one case was reported in floor of mouth [Table/Fig-7].
Non infiltrating angiolipoma (NIAL) from 2008-2016.
| Authors | Year | Age/Sex | Site | Size |
|---|
| Park JY et al., [6] | 2008 | -* | Floor of mouth | -* |
| Altug H A et al., [5] | 2009 | 22/M | Cheek | 4X3cm |
| Arenaz Bua J et al., [9] | 2010 | 5/M | Cheek | 2.5x2.5cm |
| Arenaz Bua J et al., [9] | 2010 | 58/F | Cheek | 2x2cm |
| Studart-Soares E C et al., [10] | 2010 | 65/F | Retromolar area | 1.5x1.5 cm |
| Yanase S et al., [11] | 2011 | 76/M | Buccal mucosa | 20x20mm |
| Palaia G et al., [12] | 2011 | 66/F | Cheek | 2x1.5cm |
| Sah K et al., [8] | 2012 | 9/F | Upper lip | 2x2cm |
| Silva Junior G O et al., [13] | 2013 | 57/M | Pteriygomandibular raphae | 15mmx15mm |
| Mohiuddin SA et al., [3] | 2014 | 46/M | Buccal vestibule | 4x2cm |
| Chandrashekaran D et al., [14] | 2016 | 55/F | Hard palate | 1.5x1.5cm |
| Bhuyan SK et al., (this report) | 2016 | 28/F | Floor of mouth | 3x3.5cm |
*Not available
In view of the intraoral angiolipomas, there was a ratio of 3:1 for non-infiltrative to infiltrative subtypes. Mean age of the patients with NIAL (28.2 years) was lower than the mean age of the patients affected by infiltrative angiolipomas (50.5 years), and mean size of the non-infiltrative lesions (3.1cm) was also lower than the mean size of the infiltrative lesions (3.8cm). Although there seems to be differences in these two parameters, the few reported cases preclude any definite conclusions [13,15]. In the present review (reported from 2008 to 2016) the mean age of NIAL was found to be 48 years (range 9-76yrs). Male predilection was observed with 6:5 as male to female ratio. The mean size of lesion was 3.8cm (range 9mm-4cm) [Table/Fig-8].
Clinical parameters of cases of non infiltrating angiolipoma (2008-2016) in the oral cavity.
| Mean age | 48 (9 to 76) |
| Sex predilection | 6:5 (male: female) |
| Site | Cheek-4 cases, Upper lip-1, Palate-1Buccal mucosa-1, Buccal vestibule-1Floor of mouth-1, Retro molar area-1Pterygo mandibular raphae-1 |
| Size | 3.8cm (0.9-4cm) |
The pathogenesis of AL remains unclear. Many of the lesions occurred in areas subject to repeated pressure or irritation and trauma has been suggested as a possible aetiologic factor. Fatty metamorphosis of a central hemangioma, hyperplasia of fat with an associated increase in vascular channels, or a true neoplasm may be the possible cause of AL. There is support for the theory that AL originates as a congenital lipoma, which later undergoes vascular proliferation. Howard and Helwig thought that embryonic sequestration of multipotential cells becomes active at puberty by hormones and differentiate into a simple lipoma. Further stimuli such as trauma can cause vascular infiltration of the lesion, but trauma is not present in many cases of AL [9]. Most AL show a normal karyotype, suggesting that these tumors can represent reactive non-neoplastic proliferations. Ida-Yonemochi H et al., reported the presence of numerous Vascular Endothelial Growth Factor (VEGF)-expressing mast cells around blood vessels in an intraoral AL, suggesting that secretion of this growth factor by mast cells could play an important role in the vascular proliferation in these tumors [16].
Most AL are originally diagnosed as lipoma. MRI, CT, sonography and aspiration biopsy can be used to differentiate between hemangioma, lipoma and AL; however, the accuracy of these methods remains low for these tumors. A definitive diagnosis in most literature has been made by histopathology. In our case also we did radiograph, USG, aspiration biopsy and MRI which was more suggestive of involvement with adjacent structures but final diagnosis was made only by histopathology only after excision of lesion.
Histological characteristics of AL reveal a well-demarcated, sometimes poorly-encapsulated, proliferation of mature adipocytes (usually representing at least 50% of the tumor mass) and interspersed connective tissue fibers showing an angiomatous proliferation composed of several small to medium sized congested blood vessels containing fibrin thrombi, and numerous mast cells. The simple presence of blood vessels in a benign lipomatous tumor is not a diagnostic criterion for angiolipomas. AL do not present representative amounts of other mesenchymal elements, such as muscle and neural tissue, or pleomorphism and necrosis. Our case fulfilled all histological criteria for an intraoral NIAL [Table/Fig-6a,b]. When diagnosing intraoral AL, due to the presence of this angiomatous component, it is essential to exclude other histological differential diagnosis, such as a conventional lipoma with prominent blood vessels, hemangiomas with fat entrapment, and lymphangiomas and Kaposi’s sarcomas in close relationship to adipose tissue [13]. Recent marker—PCNA and Ki67 immuni-histological staining can be performed to evaluate the proliferative capacity of tumors [11].
Current histologic guidelines for diagnosis of AL are as follows [8,9]:
Well encapsulated (non-infiltrating ALs) or poorly encapsulated (infiltrating ALs).
Evidence of 50% mature adipocytes in the tumour.
Interspersed angiomatous proliferation in the tumour.
Fibrinous micro-thrombi.
Absence of other mesenchymal elements (smooth muscle) or pleomorphism [Table/Fig-6a,b].
The case reported in the present study was classified as non-infiltrating lesions and were successfully managed through conservative surgical approach without any complication and no recurrence was observed within one year of follow-up. Most intraoral AL reported till date were managed through simple excision [13–15].
Conclusion
Angiolipomas are rarely seen in oral cavity. The case presented here showed typical clinical and histopathological findings of a NIAL. This was the second case to be reported in floor of mouth. This review of literature has added 12 cases of NIAL to the previously available 14 cases raising the total number to 26 cases for documentation.
*Not available
[1]. Rajendran R, Shivapatha Sundharam B, Shafer’s Textbook of Oral Pathology 2012 7 edNoidaElsevier:140 [Google Scholar]
[2]. Adoga AA, Nimkur TL, Manasseh AN, Echejoh GO, Buccal soft tissue lipoma in an adult Nigerian: A case report and literature reviewJ Med Case Reports 2008 2:382 [Google Scholar]
[3]. Mohiuddin SA, Badal S, Doiphode A, Sulatana S, Noninfiltrating intraoral angiolipoma in the mandibular buccal vestibuleJournal of Oral Sciences 2014 5(1):33-34. [Google Scholar]
[4]. Hamakawa H, Hino H, Sumida T, Tanioka H, Infiltrating angiolipoma of the cheek: A case report and a review of the literatureJ Oral Maxillofac Surg 2000 58:674-77. [Google Scholar]
[5]. Altug HA, Sahin S, Sencimen M, Dogan N, Erdogan Ö, Non-infiltrating angiolipoma of the cheek: A case report and review of the literatureJ Oral Sci 2009 51:137-39. [Google Scholar]
[6]. Park JY, Yoon YH, Rha KS, Koo BS, A case of angiolipoma of floor of mouthKorean Journal of Otolarynologology Head and Neck Surgry 2008 51(4):399-401. [Google Scholar]
[7]. Enzinger FM, Weiss SW, Soft tissue tumours, benign lipomatous tumours 2008 5th edSt LouisCV Mosby:429-76. [Google Scholar]
[8]. Sah K, Kadam A, Sunita JD, Chandra S, Non-infiltrating angiolipoma of the upper lip: A rare entityJ Oral Maxillofac Pathol 2012 16(1):103-06. [Google Scholar]
[9]. Yanase Arenaz Búa J, Luáces R, Lorenzo Franco F, García-Rozado A, Crespo Escudero JL, Fonseca Capdevila E, Angiolipoma in head and neck: Report of two cases and review of the literatureInt J Oral Maxillofac Surg 2010 39:610-15. [Google Scholar]
[10]. Studart-Soares EC, Gurgel Costa FW, Bitu Sousa F, Negreiros-Nunes Alves AP, Verde Osterne RL, Oral lipomas in a Brazilian population: A 10-year study and analysis of 450 cases reported in the literatureMed Oral Patol Oral Cir Bucal 2010 15:e691-96. [Google Scholar]
[11]. Anase S, Nomura J, Matsumura Y, Kato H, Takeoka T, Imura H, Angiolipoma of the cheek-A case report with a literature reviewAsian Journal of Oral and Maxillofacial Surgery 2011 23:35-37. [Google Scholar]
[12]. Palaia G, Giamari G, Giudice R, Galankis A, Tenore G, Romeo U, Excision of oral angilipoma by ktp laser a case reportAnnals Di Stomatologia 2011 (1-2):28-31. [Google Scholar]
[13]. Silva-Junior G O, Picciani BL, Costa R C, Barbosa S M, Silvares M G, Oral soft tissue angiolipoma-Report of two cases of rare oral lipomatous lesion with emphasis on morphological and immunohistochemical featuresJournal of Oral Science 2013 55(1):85-88. [Google Scholar]
[14]. Chanrasekaran D, Swami RDC, Simhan MN, Kumar AEN, Natarajan PS, Non infiltrating angiolipoma of the palate in geriatric patient: A Case report with review of literatureJ Clin Diagn Res 2016 10(1):ZD01-ZD02. [Google Scholar]
[15]. Fregnani ER, Pires FR, Falzoni R, Lopes MA, Vargas PA, Lipomas of the oral cavity: Clinical findings, histological classification and proliferative activity of 46 casesInt J Oral Maxillofac Sur 2003 32:49-53. [Google Scholar]
[16]. Ida-Yonemochi H, Swelam W, Saito C, Saku T, Angiolipoma of the buccal mucosa: A possible role of mast cell-derived VEGF in its enhanced vascularityJ Oral Pathol Med 2005 34:59-61. [Google Scholar]