Human navigation, perception and interpretation of the surrounding visual scene require interaction between the visual system, the motor system and the parts of the brain serving attention, perception and cognition [1]. Hence, vision is not just what is identified and resolved but also, how it is interpreted. Vision involves about 40% of the brain [2]. It has two interrelated functions: to perceive objects along with understanding their relations, which forms the basis for the person’s cognitive function and control of actions by the motor system with respect to the object [3]. Any damage to the visual brain can result in impaired visual function including perceptual and cognitive dysfunction [2]. Cerebral Visual Impairment (CVI) is a result of damage to the visual pathways, higher visual centres and the occipital cortices [4]. The two principle higher visual pathways involved in CVI are: the dorsal stream, connecting the occipital lobes to the parietal lobes and the ventral stream, connecting the occipital lobes to the temporal lobes [5]. CVI has heterogeneous clinical manifestations depending on the region and degree of visual system involvement [6]. Sixty percent of children with cerebral palsy manifest features suggestive of CVI [6,7]. Structured clinical history taking and observation for visual cognitive and perceptual behaviours have been shown to provide an effective as well as a reproducible method of ascertaining the nature and degree of the child’s visual field, cognitive and perceptual impairments [4,8-10].
Existing constructs in one culture warrant study in relation to their content and structural contexts in another culture. Cultural differences like always using one’s right hand to receive or give things to people or to avoid making an eye contact while having a conversation with an elder, can constitute a major hindrance for determining the effectiveness of a clinical tool especially when subjective elements of structured history taking and observation are involved. The Structured Clinical Question Inventory (SCQI) is a question inventory developed in United Kingdom to diagnose CVI based on clinical history and observation of parents and caregivers.
The aim of this study was to determine the face, content and construct validity as well as the internal consistency of the SCQI in an Indian context.
Materials and Methods
This study was conducted at the CVI Clinic, Department of Ophthalmology, at a tertiary care teaching hospital in Southern India. The data from the case-notes of all children below 18 years of age, referred by paediatricans, paediatric neurologists and child psychiatrists to the CVI Clinic from March 2011 to February 2012, were extracted by the primary researcher (SSP), a consultant ophthalmologist with 8 years experience of working with children and with training in CVI, its identification and management. The study was reviewed and approved by the Institutional Review Board.
Ophthalmological data based on clinical history, clinical observation, ocular examination, visual assessment using age-appropriate preferential looking cards (Lea paddle, Cardiff acuity cards), or Optokinetic Nystagmus (OKN) stimuli (OKN drum), as well as crowded and uncrowded visual acuity charts (Snellen’s visual acuity and Kay pictures), ocular motility assessment, slit-lamp biomicroscopy and dilated fundus examination using indirect ophthalmoscopy were extracted from the case-notes by the primary researcher (SSP). The binocular visual acuity, (using the appropriate refractive correction), was the chosen assessment in most of the children due to their age and associated neurological disabilities. In addition, the clinical information specifically relating to the SCQI [4], a 15-domain (50 item) inventory, based on a face-to-face interview in a non–leading manner was performed in all patients. The data extracted from the SCQI were the domains and SCQI score. The domains comprised: Neglect/ Inattention (6 items), Impaired attention (4 items), Gaze apraxia (1 item), foreground clutter (3 item), background clutter (1 item), Difficulty with crowds (5 items), dyskinetopsia (2 items), face recognition (4 items), shape recognition (1 item), word recognition (1 item), object recognition (1 item), visual memory (1 item), orientation (2 items), visual guidance of movement (11 items), visual field impairment (7 items). The SCQI score was accorded by the interviewing ophthalmologist, out of a score of 15 (each domain scored separately as yes or no) relying on the caregiver’s answers to the questions in each domain and the ophthalmologist’s own observation of the child. If the ophthalmologist found clear evidence of visual dysfunction in any domain then that domain was scored as positive even if the caregiver did not report it. The neuro-psychological details were extracted from the case-notes of the appropriate referring physician.
Structured Clinical Question Inventory (SCQI)
The 50 item question inventory used in this study was based on one developed by GND [4] in Glasgow and it required minor modification for the Indian cultural setting. For people living in one-unit apartment/from villages, the question on orientation within familiar situations was omitted.
The primary researcher (SSP) modified the following questions to suit the cultural setting.
‘While on a walk do you carry your child or allow them to walk? If they walk: Does your child identify the puddles and uneven ground?’.
‘In the locality where you live is there vehicular traffic? If yes: does your child walk into the traffic’. (Many villages in India do not have vehicular traffic and people have to walk long distances to avail themselves of transport).
‘If there is some object lying on the floor what does your child do?’
When your child is asked to replace an object on the table, is the object placed at the edge of the table?’.
‘Does your child eat food on his/her own?’ If yes, does the child need prompting to finish all that is served on the plate?’ (Many families feed their children during lunch and dinner, firstly due to the number of food items eaten during these meals and secondly due to lack of time for the parents).
‘Do you have a TV at home? If yes, does your child watch TV/ does your child go close to the TV to watch?’
‘Does your child know letters/ shapes?’ (For children who have never gone to school nor been taught at home, we have omitted this question.)
Validation Process
We studied the face, content, construct validity and internal consistency of the SCQI. This exercise was carried out at the end of the data collection. The face validity accords a subjective view of the diagnostic relevance of the SCQI with respect to CVI by asking the question ‘Does this inventory comprehensively list the CVI features?’ For verification, four ophthalmologists with various levels of training as well as experience (a post graduate trainee, a senior resident, consultant ophthalmologist with not more than 4 years experience and consultant ophthalmologist with 8 years of experience) were consulted. The content validity was ascertained after the same ophthalmologists endorsed the different dimensions of CVI in the SCQI by rank ordering the domains from 1-15. Any domain that was not included in the ranking by at least 3 of the ophthalmologists was not considered part of the concept of CVI.
Statistical Methods
The Pearson correlation coefficient tests were performed to seek the total domain correlation of the total SCQI score. Those domains with a high correlation coefficient with the SCQI total score were considered to give the greatest contribution to the concept of CVI. Pearson’s correlation co-efficient test with resampling was carried-out (boot-strapped 1000 times) to calculate the 95% confidence interval of the correlation coefficient. To document the homogeneity of the 15 domains in the SCQI or how well the existing domains picked up CVI, we used the statistical concept of internal consistency. The internal consistency of the SCQI was evaluated using Cronbach’s alpha. The construct validity of the SCQI was tested using exploratory factor analysis with principal component analysis and varimax rotation after checking for the suitability of the data with the Kaiser-Meyer-Olkin Measure of sampling adequacy and the Bartlett’s Test of sphericity. We retained a factor if its Eigen value as ≥ 1 (Guttman-Kaiser rule). The domain was considered to have ‘loaded’ on to a factor if the coefficient value was ≥ 0.4 and ‘cross-loaded’ if the secondary loading had an unacceptably high value of ≥ 0.3. Initially, we analysed the data without any presumptions about the number of factors and let the data fall where they might. Later we imposed a 2-factor model to explain our biological assumptions that dorsal and ventral stream symptoms would group together under specific factors. All test values were considered significant if p ≤ 0.05. Data were analysed using SPSS (version 19.0).
Results
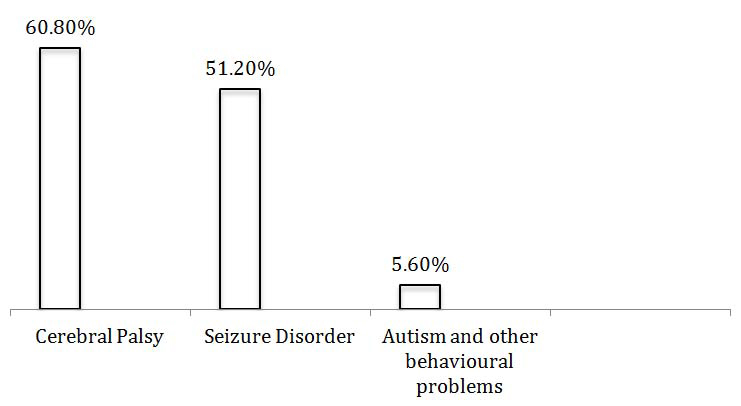
Of the total 342 children seen in the CVI clinic, 35.7% (N=122) were boys and 64.3% (N=220) were girls with a mean age of 3.8 years (range 0-17years, median 3 years). The concomitant neurological problems of children included in the study were cerebral palsy 60.8% (N=208), symptomatic epilepsy 51.2% (N=175), autism and other behavioural issues 5.6% (N=19) [Table/Fig-1].
Profile of children included in the study.
The rank ordering, without any reservation, of all the items of SCQI as measuring the clinical entity of CVI suggested that the measure has good face validity. Also, the practicing ophthalmologists considered that all the dimensions of CVI were represented by the existing items in the SCQI and did not include any other item when they were given the choice, suggesting a good content validity for the measure.
The internal consistency (Cronbach’s α) of the SCQI as a whole was 0.93 and for each domain it ranged from 0.92 to 0.94. The total-domain correlation ranged from 0.02 for the domain of Neglect to 0.74 for the Foreground clutter [Table/Fig-2]. As the Kaiser-Meyer-Olkin Measure of Sampling Adequacy was 0.89 and p-value of Bartlett’s Test of Sphericity was 0.001, we found the sample to be adequate enough to conduct an explorative factor analysis to identify the structure of the SCQI. Initially, when we analysed the data without any presumptions about the number of factors, the 15 domains fell under a 5-factor model that explained 73.16 % of the variance. Later when we imposed a 2-factor model to explain our biological assumptions, the domains grouped under the two factors, which were identified as the ‘Dorsal Stream Dysfunction’ and ‘Ventral Stream Dysfunction’ [Table/Fig-2]. The total variance explained by the 2-factor model was 62.60% and the details of the domains that loaded on to each of the factor are given in [Table/Fig-3].
Content and construct validity of Structured Clinical Question Inventory showing in rank order the question groupings that are most likely to identify features of CVI.
| Rank Order | Endorsement Rate % (N) | Total-item correlationr (95% CI) | Internalconsistency(α) | Factor structure |
|---|
| DSD | VSD |
|---|
| Neglect and inattention | 14 | 12.9 (44) | 0.02 (-0.27-0.32); p= 0.8 | 0.93 | 0.73 | 0.09 |
| Impaired attention | 7 | 50.1% (N=171) | 0.13 (-0.07-0.35); p=0.2 | 0.93 | 0.04 | -0.31 |
| Gaze apraxia | 15 | 5.3% (N=18) | 0.37 (0.15-0.54); p=0.002 | 0.94 | 0.26 | -0.41 |
| Foreground clutter | 5 | 19.4% (N=66) | 0.74 (0.65-0.82); p<0.001 | 0.93 | 0.43 | 0.003 |
| Background clutter | 1 | 20.5% (N=70) | 0.72 (0.63-0.81); p<0.001 | 0.93 | 0.88 | 0.08 |
| Difficulty with crowd | 6 | 18.8% (N=64) | 0.47 (0.27-0.64); p<0.001 | 0.92 | 0.88 | 0.05 |
| Dyskinetopsia | 2 | 26.7% (N=91) | 0.55 (0.36-0.71); p<0.001 | 0.93 | 0.55 | 0.005 |
| Face recognition | 8 | 32.6% (N=111) | 0.43 (0.18-0.61); p< 0.001 | 0.93 | 0.49 | 0.22 |
| Word recognition | 11 | 17.3% (N=59) | 0.51 (0.34-0.65); p<0.001 | 0.93 | 0.23 | 0.48 |
| Shape recognition | 12 | 17% (N=58) | 0.46 (0.28-0.62); p<0.001 | 0.92 | 0.08 | 0.90 |
| Object recognition | 9 | 23.5% (N=80) | 0.56 (0.40-0.70); p<0.001 | 0.93 | 0.06 | 0.83 |
| Poor memory | 10 | 11.1% (N=38) | 0.42 (0.21-0.60); p<0.001 | 0.93 | 0.17 | 0.84 |
| Orientation | 13 | 12.3% (N=42) | 0.47 (0.29-0.64); p<0.001 | 0.93 | 0.44 | 0.009 |
| Impaired Visual guidance of movement | 4 | 16.1% (N=55) | 0.73 (0.64-0.80); p< 0.001 | 0.94 | 0.10 | 0.83 |
| Visual Field impairment | 3 | 28.7% (N=98) | 0.54 (0.35-0.69); p< 0.001 | 0.93 | 0.83 | 0.11 |
DSD- (Dorsal Stream Dysfunction, VSD- Ventral Stream Dysfunction)
Domains regarded as dorsal stream dysfunction and ventral stream dysfunction.
| Dorsal Stream Dysfunction | Ventral Stream Dysfunction |
|---|
| Neglect and inattention | Recognition of face |
| Impaired visual attention | Recognition of words |
| Gaze apraxia | Recognition of shapes |
| Foreground clutter | Recognition of objects |
| Background clutter | Poor visual memory |
| Visual field impairment | Orientation |
| Impaired guidance of movement | |
| Difficulty with crowding | |
| Dyskinetopsia | |
Discussion
The SCQI was developed to encompass the well-documented clinical features of CVI. However, it still has to be evaluated empirically before being clinically used in another culture with possibly different psychosocial constructs. Therefore, this study was undertaken to validate the SCQI in the Indian context. The face validity of the SCQI as a measure for CVI has long been established by consensus among clinicians elsewhere [9], and we accepted it as such.
The total-domain correlation ranged from low (r=0.02 for neglect) to moderate (r=0.74 for foreground clutter), thus some domains contributed more to the concept of CVI as measured by SCQI. Neglect, as identified by these questions, was dissociated from other features of CVI in this population. This may be a genuine dissociation or indicate a need to change the questions relating to neglect in this population. The internal consistency of the SCQI was high, ranging from 0.92 to 0.94. The internal consistency that we have documented is much higher than in the previous study where it ranged from 0.56 to 0.82 [9]. This may suggest a more homogeneous pathology range in our setting. Such a high level of consistency could suggest redundancy and the possibility of reducing the number of domains for speed of diagnosis. Against this however it must be remembered that one of the purposes of the SCQI is to get a detailed understanding of a child’s visual perceptual problems so that detailed adaptive strategies to behaviour and environment can be suggested.
The purpose of the factor analysis was to see which features tend to group together in patients and to test the biological plausibility of the responses in order to find out, if there was evidence of symptoms attributable to dorsal stream (occipito-parietal pathways) dysfunction and ventral stream (occipito-temporal pathways) dysfunction, clustering together and also symptoms attributable to CVI. The construct validity of the SCQI with exploratory factor analysis demonstrated a 5-factor and 2-factor structure with different exploratory variances for the models. Although the 5-factor model had a higher level of variance, the five factors could not be explained by the current theoretical underpinning of the SCQI. Therefore, we imposed a biologically plausible 2-factor (dorsal and ventral) model as a better structural model despite its lower level of explanatory variance. The following domains are thought to be dorsal stream dysfunctions and did cluster together as expected: Neglect/inattention, Impaired attention, Gaze apraxia, Foreground clutter, Background clutter, Difficulty with crowding, Dyskinetopsia and visual field impairment; the following domains are thought to be ventral stream dysfunctions and did cluster together as expected: Impaired Word recognition, Shape recognition, Object recognition and Poor memory [9]. However, unexpectedly, Impaired Visual Guidance of Movement (thought to be dorsal) loaded on to the factor of Ventral Stream Dysfunction and impaired Face Recognition, as well as Orientation (thought to be ventral) loaded onto Dorsal Stream Dysfunction. These ‘anomalies’ are worthy of further investigation and suggest that it is rare for children to have only symptoms, which are regarded as dorsal or ventral but that a mixed picture is often seen. This 2- factor model supported the theoretical construct of CVI better.
With our current validation data, it appears that it is possible to shorten the SCQI into a brief instrument for identifying CVI by including only those domains that have a high factor-loading coefficient. Thus, the domains of Neglect, Background clutter, Difficulty with crowds and visual field impairment can represent the domains for identifying ‘Dorsal Stream Dysfunction’, while Shape recognition, Object recognition and Poor memory can represent the domains for identifying ‘Ventral Stream Dysfunction’ to produce a brief diagnostic version of the SCQI. On the other hand, when the responses to the questions are used to guide habilitation, additional contextually appropriate questions may warrant design and inclusion for the management of children in India. To further improve the lingual and functional equivalence of the items in domains, validity of the instrument, standardization of the administration of tasks and questions to suit the needs and resources of low and middle-income country settings, we suggest that a modified, abridged version of the measure warrants consideration.
Conclusion
The Structured Clinical Question Inventory has a similar theoretical construct between the UK and India. The clinical use of a short version of SCQI may be warranted and useful for middle and low-income countries like India, where there are limited funds and manpower. The diagnostic accuracy, reliability and utility of this measure for CVI warrant further study.
DSD- (Dorsal Stream Dysfunction, VSD- Ventral Stream Dysfunction)