Anaemia is the most common nutritional disorder worldwide. According to WHO adolescent age group is defined as life span between 10-19 years [1]. In India the prevalence of anaemia among adolescent girls were 56% and this amounts to an average 64 million girls at any point in time [2]. Studies conducted in different regions of India shown that the prevalence of anaemia was 52.5% in Madhya Pradesh, 37% in Gujarat, 41.1% in Karnataka, 85.4% in Maharashtra, 21.5% in Shimla, 56.3% in Uttar Pradesh, 77.33% in Andhra Pradesh, 58.4% in Tamilnadu and in Kerala (19.13% among college students and 96.5% in tribal area) [3–12]. The major risk factors identified from the above studies were socio-economic status, blood loss during menstruation, nutritional status, hand hygiene and worm infestation.
Nutritional needs of girls during adolescent period are generally ignored leading to stunting and poor health. One of the major consequences of the physiological changes and the nutritional neglect which happens during this period is anaemia. In a tropical country like India helminthic infestation is very common which can lead to chronic blood loss which in turn results in anaemia [13].
Anaemia causes adverse consequences as the disease progress. It not only affects the growth of adolescent girls but also affect their attentiveness, memory and school performance and retention in school and attendance. It also causes delay in onset of menarche, affects immune system leading to infections. If the anaemic adolescent girl becomes pregnant, it may increase foetal morbidity and mortality, increase the perinatal risk, increase the incidence of Low Birth Weight (LBW), and overall increase in Infant Mortality Rate (IMR) and Maternal Mortality Rate (MMR). As growing pregnant adolescents compete with the growing foetus for nutrients anaemia in pregnancy will be worse than in older women [14].
In-spite of Kerala having good indicators of health compared to other states in India, the area which need focus is the nutrition of adolescent girls. Number of studies conducted in Kerala regarding adolescent nutrition were very less with relatively few published studies among them [11,12]. Hence the data regarding magnitude of anaemia among adolescent girls are scarce, particularly community based studies. It is not possible to implement a health programme without sufficient data. Hence, this study was done to find out the prevalence of anaemia and its associated factors among adolescent girls.
Materials and Methods
After getting ethical clearance from institutional review board, a cross-sectional study was conducted among adolescent girls (10-19 years) in Ettumanoor panchayat which is the field practice area of Department of Community Medicine, Government Medical College, Kottayam during the period from April 2013 to May 2014
Sampling frame: Prior permission was obtained from Child Development Project Officer (CDPO) of Ettumanoor block panchayat. Details about adolescent girls were obtained from all anganwadi centers in the same area. Based on data from registers in the anganwadi centers, 2601 adolescent girls were there in ettumanoor panchayat.
Sample size calculation: Based on the study conducted by Chaudhary et al., prevalence of anaemia among adolescent girls were 35.2% [15]. Hence 35.2% was considered as the expected prevalence (p) with an allowable error of 6% (absolute precision = d) was used for sample size calculation. Z-value at 95% confidence interval =1.96.
For a finite population, finite population correction needed
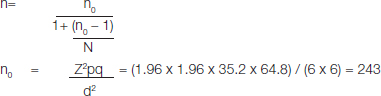
n= sample size of finite population
N = population size = 2601
Calculation for sample size
n0 = 243 after finite correction, n = 223
Based on the above calculation sample size was found to be 223, but considering non-availability of subjects due to reasons like non-consenting, migration and non-availability on repeated attempts, extra 20% was added, which made final sample size to 268 which rounded to 270.
Sampling technique: Using SPSS random number generator, 270 adolescent girls were selected randomly with a sampling frame of 2601. The selected adolescent girls were mobilized to the nearby anganwadi centers for the ease of blood collection with the help of Accredited Social Health Activist (ASHA) workers and Junior Public Health Nurse (JPHN).
Inclusion criteria
Adolescent girls of the age group 10-19years who were residing in the study area for a minimum period of 6months.
Exclusion criteria
Adolescent girls who were pregnant.
Adolescent girls who were not willing to participate in the study
Case definition
WHO cut off values for assessing anaemia in adolescent girls [16].
Normal > 12gm/dl
Mild anaemia >11gm/dl and <11.9gm/dl
Moderate anaemia >8gm/dl and <10.9gm/dl
Severe anaemia <8gm/dl
A brief introduction about the study topic was discussed with the anganwadi workers, ASHA workers and JPHN in Ettumanoor primary health center area. Details about the study and regarding blood collection, stool collection and importance of the present study were explained to them by researcher. Study subjects selected by simple random sampling technique were contacted with the help of ASHA and anganwadi workers and preliminary information about the concept of the study was conveyed to parent of study subjects. The selected study subjects were asked to assemble at anganwadi center with the help of ASHA workers and JPHN on specified date for the ease of blood and stool collection by researcher. Those girls who were not able to attend on that particular day were contacted with the help of anganwadi worker and the blood sample was collected from them during the next visit. Girls who were not available even after two consecutive visits were excluded from the list. A proforma which was designed with the help of head of the department of community medicine, pathology and microbiology was used for data collection. Pilot study was conducted among 50 adolescent girls in the service area to test the proforma. Based on the problems faced corrections were done in the proforma. After getting informed and written consent from the parents, researcher collected data regarding socio-demographic variables, menstrual pattern, nutrition habits (24 hour recall method), deworming status, personal hygiene and iron and folic acid intake history using pre-designed and pre-tested proforma. Weight was measured using portable weighing machine by instructing the subjects to stand erect over the machine without foot wears and facing the wall and height measured using measuring tape fixed in the wall by instructing the subjects to stand erect with heel, buttocks, scapula and occiput in a straight line and touching the wall. Blood sample collected under aseptic precautions with 2ml disposable syringe and peripheral smear were prepared with a drop of blood in a glass slide, and the remaining blood were transferred to Ethylenediaminetetraacetic acid (EDTA) tubes and properly labelled (name and serial number). After transferring the blood in EDTA tube the blood samples were gently agitated between the palms to mix with the EDTA. The blood sample collected in the EDTA tubes were transported using vaccine carrier to Advanced Clinical Research (ACR) lab in the medical college campus for further analysis and stool samples to the department of microbiology. Haemoglobin estimation was done using Auto-analyser SYSMAX 800i. Peripheral smear and stool examination for ova/cyst were done with help of pathologist and microbiologist of Government Medical College, Kottayam.
Data Compilation and Analysis
After the completion of data collection, it was coded and was entered into microsoft excel. The compiled data was imported to the software SPSS version 16.0 for further analysis. Association between the categorical variables were tested with Chi-square test and for continuous variables independent t-test was used. The level of significance was fixed at p-value of < 0.05. Logistic regression was done to find out the independent factors associated with anaemia.
Results
A cross-sectional study was conducted to find out the prevalence of anaemia and its associated factors among adolescent girls in Ettumanoor panchayat. A total of 270 adolescent girls were selected randomly for the study, of which 13 were excluded due to lack of consent and non-availability. Finally the total participants were 257.
The mean age of the study subject was 13.39 years with a standard deviation of 2.341 years. Most of the girls 144(56%) belonged to the age group of 10-13 years. Majority 172(66.9%) belonged to hindu religion followed by christians 74(28.8%) and muslims 11(4.3%).
Most of them 159(62%) belonged to nuclear family. Majority of the study subjects belonged to middle class 137(53.4%) followed by upper lower 117(45.5%) according to modified “Kuppusamy Classification” [17]. Among them 162(63%) have attained menarche. Mean age of menarche among the study subjects were found to be 12.37 years with a standard deviation of 1.158 years.
Based on WHO Z-score system [18], children aged 5 to 19 years are classified into severely thin, thin normal, overweight and obese. In the present study 44(17.2%) were thin and 31(12%) were overweight or obese. This shows the twin burden of malnutrition in the study subjects.
Prevalence of anaemia among the study subjects was found to be 21% (54/257) [Table/Fig-1]. Majority of them 19.1% (49/257) had mild anaemia and rest moderate anaemia 1.9% (5/257) [Table/Fig-2]. Most of the subjects 36 (66.6%) had normocytic normochromic, followed by 13(24.1%) had microcytic hypochromic anaemia [Table/Fig-3]. The mean Packed Cell Volume(PCV), Mean Corpuscular Volume(MCV), Mean Corpuscular Hemoglobin(MCH) and Mean Corpuscular Hemoglobin Concentration(MCHC) were significantly lower among anaemic subjects compared to normal subjects [Table/Fig-4].
Prevalence of anaemia among study sample (N=257).
| Haemoglobin status | Number of girls | Percentage |
|---|
| Anaemic (Hb < 12 gm) | 54 | 21.0 |
| Normal (Hb > 12 gm) | 203 | 79 |
| Total | 257 | 100 |
Classification of study subjects based on grading of anaemia (N=257).
| Grading of anaemia (Hb in gm/dl) | Number of girls | Percentage |
|---|
| Normal (>12) | 203 | 79 |
| Mild anaemia (11-11.9) | 49 | 19.1 |
| Moderate anaemia (8-10.9) | 5 | 1.9 |
| Total | 257 | 100 |
Classification of anaemia according to peripheral smear study (N =54).
| Anaemia type | Number of girls | Percentage |
|---|
| Normocytic normochromic | 36 | 66.6 |
| Microcytic hypochromic | 13 | 24.1 |
| Dimorphic | 5 | 9.3 |
| Total | 54 | 100 |
Distribution of anaemia according to various blood indices (N=257).
| Blood indices | Haemoglobin status | Frequency | Mean | Std. Error Mean | t value | p-value |
|---|
| PCV* | Anaemic | 54 | 35.161 | 0.3180 | 13.525 | <0.001 |
| Normal | 203 | 39.547 | 0.1444 |
| MCV† | Anaemic | 54 | 84.874 | 0.7699 | 2.7336 | 0.0067 |
| Normal | 203 | 86.800 | 0.3005 |
| MCH‡ | Anaemic | 54 | 27.470 | 0.3365 | 2.9985 | 0.0030 |
| Normal | 203 | 28.385 | 0.1296 |
| MCHC§ | Anaemic | 54 | 32.126 | 0.2119 | 2.3858 | 0.0178 |
| Normal | 203 | 32.589 | 0.0828 |
*Packed cell volume, † Mean Corpuscular Volume, ‡ Mean Corpuscular Haemoglobin, § Mean Corpuscular Haemoglobin Concentration
The major risk factors found to be significantly associated with anaemia in the present study in the univariate analysis were presence of ova or cyst in stool (p = 0.003) OR (odds ratio) = 2.942(CI = 1.422-6.085) and number of pads usage per day during menstruation (p = 0.004). Protective factors were personal hygienic practices including hand washing before food intake (p = 0.026) OR = 0.5 (95% C.I. = 0.27-0.93), hand washing after toileting (p = 0.02) OR = 0.311(95% C.I. = 0.11-0.88) and usage of foot wear (p = 0.022) OR = 0.247 (95% C.I. = 0.07-0.89) and Jaggery intake (p = 0.042) [Table/Fig-5,6].
Distribution of anaemia according to various risk factors (N=257).
| Risk factors | Anaemia present (%) | Anaemia absent (%) | Chi-square value | p-value |
|---|
| Age group in years | 10-13 | 31(21.5) | 113(78.5) | 0.078 | 0.962 |
| 13-16 | 18(20.7) | 69(79.3) |
| 16-19 | 5(19.2) | 21(80.8) |
| Family type | Nuclear | 37(23.3) | 122(76.7) | 1.282 | 0.258 |
| Joint | 17(17.3) | 81(82.7) |
| Socio-economic status | Upper | 1(33.3) | 2(66.7) | 0.307 | 0.959 |
| Upper middle | 7(21.9) | 25(78.1) |
| Lower middle | 22(21) | 83(79) |
| Upper lower | 24(20.5) | 93(79.5) |
| Menarche status | Attained | 32(19.8) | 130(80.2) | 0.418 | 0.518 |
| Not attained | 22(23.2) | 73(76.8) |
| Dietary habit | Vegetarian | 3(33.3) | 6(66.7) | 0.853 | 0.356 |
| Non-vegetarian | 51(20.6) | 197(79.4) |
| BMI adjusted for age | Severely Thin | 1(7.7) | 12(92.3) | 3.521 | 0.4746 |
| Thin | 5(16.1) | 26(83.9) |
| Normal | 39(21.4) | 143(78.6) |
| Overweight | 6(26.1) | 17(73.9) |
| Obese | 3(37.5) | 5(62.5) |
| Supplementary nutrition | Not utilized | 24(22) | 85(78) | 0.116 | 0.734 |
| Utilized | 30(20.3) | 118(79.7) |
| History of iron prophylaxis | Yes | 5(14.7) | 29(85.3) | 0.939 | 0.333 |
| No | 49(22) | 174(78) |
| Skipping of meals | Yes | 29(21.6) | 105(78.4) | 0.067 | 0.796 |
| No | 25(20.3) | 98(79.7) |
| Pallor | Present | 18(27.3) | 48(72.7) | 2.098 | 0.148 |
| Absent | 36(18.8) | 155(81.2) |
Distribution of anaemia according to jaggery intake and personal hygiene (N=257).
| Variable | Anaemia present (%) | Anaemia absent (%) | Chi-square value | p-value |
|---|
| Jaggery intake | Weekly | 10(37) | 17(63) | 6.353 | 0.042 |
| Occasionally | 41(18.5) | 181(81.5) |
| Never | 3(37.5) | 5(62.5) |
| Hand washing after toileting | Every time | 47(19.5) | 194(80.5) | 5.315 | 0.021 |
| Occasionally | 7(43.8) | 9(56.2) |
| Hand wash before food intake | Every time | 30(17.1) | 145(82.9) | 4.946 | 0.026 |
| Occasionally | 24(29.3) | 58(70.7) |
| Foot wear | Every time | 49(19.8) | 198(80.2) | 5.268 | 0.022 |
| Occasionally | 5(50) | 5(50) |
| Deworming status | Done | 26(19.3) | 109(80.7) | 0.526 | 0.47 |
| Not done | 28(23) | 94(77) |
| Ova/cyst (N=132 only 132 subjects provided stool sample) | Present | 29(54.7) | 24(45.3) | 8.709 | 0.003 |
| Absent | 23(29.1) | 56(70.9) |
The risk factors associated with anaemia in logistic regression were presence of ova or cyst in stool (worm infestation), odds ratio 4.150 (95% C.I. 1.180 – 14.598), p = 0.027 and number of pads use per day during menstruation, odds ratio 3.063 (95% C.I. 1.606 – 5.841), p = 0.001. Hand washing before food intake was emerged as a protective factor with odds ratio of 0.153 (95% C.I. 0.038 – 0.613), p = 0.008. Regular usage of foot wear was also evolved as a protective factor with odds ratio of 0.042 (95% C.I. 0.002 – 0.870), p=0.04 [Table/Fig-7].
Logistic regression (N = 132).
| Variables in the equation | Constant | Standard error | p-value | Odds ratio | 95% C.I. for odds ratio |
|---|
| Lower limit | Upper limit |
|---|
| Presence of stool ova or cyst | 1.423 | 0.642 | 0.027 | 4.150 | 1.180 | 14.598 |
| Number of pads per day | 1.119 | 0.329 | 0.001 | 3.063 | 1.606 | 5.841 |
| Hand washing after toilet | -21.676 | 19033.363 | 0.999 | 0.00 | 0.00 | |
| Hand washing before food intake | -1.876 | 0.708 | 0.008 | 0.153 | 0.038 | 0.613 |
| Regular usage of foot wear | -3.164 | 1.543 | 0.040 | 0.042 | 0.002 | 0.870 |
| Jaggery intake | 0.381 | 1.342 | 0.777 | 1.464 | 0.105 | 20.323 |
Discussion
Anaemia is the major public health problem among adolescent girls of age 10-19 years. The reason for high incidence of anaemia among the adolescent girls are increased requirement during growth spurt, menstrual loss, low intake of iron rich food, erratic eating habits [19].
In the present study 257 adolescent girls of age 10-19 years were included. Majority of them 144 (56%) belongs to 10-13 years of age.
Prevalence of anaemia: In the present study prevalence of anaemia among the study subjects were found to be 21%. A study which was conducted among undergraduate students of government medical college, Kottayam revealed that the prevalence of anaemia was 19.13% [11]. Another study which was conducted among tribal women in Wayanad district shown that the prevalence of anaemia was found to be 96.5% [12]. Under-nutrition among tribal women was the major cause identified from the study. In a study conducted in Tamilnadu showed the prevalence of anaemia among 10-15 year old adolescent girls were found to be 58.4% [10]. Another study conducted in Andhra Pradesh showed the prevalence of anaemia among adolescent girls was 77.33% [9].
Even though prevalence of the present study was at the lower range still it is a moderate public health problem as per WHO classification [20]. Hence, this indicated the importance of adding adolescent girls in the risk group to improve their haemoglobin status.
Prevalence of anaemia according to severity: In the present study, prevalence of mild anaemia was higher with 19.1%, that of moderate anaemia was 1.9% and none of them had severe anaemia. In a study which was conducted in Wayanad district prevalence of mild anaemia was 30.5%, that of moderate anaemia was 55.9% and that of severe was 10.1% [12]. Similar results were obtained in a study conducted among adolescent girls in Andhra Pradesh with prevalence of mild anaemia was 28.7%, that of moderate anaemia 39.33% and that of severe anaemia 9.33% [9].
The high prevalence of mild and moderate anaemia demands due emphasis on iron and folic acid supplementation, iron rich food intake, health education regarding personal hygiene and periodical deworming to reduce the burden of anaemia among adolescent girls.
Peripheral smear study and hematological parameters: Even though most of the study subjects have normocytic normochromic anaemia, the mean values of PCV, MCV, MCH and MCHC were significantly lower among anaemic subjects compared to normal subjects. This finding is agreement with study conducted by Dr. Manjula et al., [11]. As iron deficiency progress the cells become more microcytic with marked fall in MCV, MCH and MCHC [11].
Factors associated with anaemia: In the present study prevalence of anaemia was more or less equally distributed in all socio-economic category, with highest among upper class 33% and least among upper lower class with 20.5%. Most of the studies conducted in various parts of India show the high prevalence in lower socio-economic category compared to upper categories. But in our study prevalence is comparatively lesser in lower socio-economic group. This may be due to iron and folic acid supplementation through peripheral health institutions and in government schools which were better utilized by lower socio-economic groups than a higher socio-economic groups. Then the poor dietary pattern followed by higher socio-economic group with more of snacks and junk foods, which lack micro-nutrients explaining the higher prevalence of anaemia among them [21].
In the present study, prevalence of anaemia was higher among those who used more number of pads, as it indirectly indicates increased amount of blood loss during menstruation.
In this study, prevalence of anaemia was higher among obese 37.5%, followed by overweight 26.1%, then normal 21.4%, thin 16.1% and severely thin 7.7%. This may be due to up-regulated hepcidin expression in obese individuals which hampering iron absorption. This result is consistent with the study conducted in United States by Dr. Nead KG et al., with 2.1% for normal weight, 5.3% for at risk for overweight and 5.5% for overweight [22]. But the result was discordant with the study conducted in rural Wardha by S. Kaur et al., where prevalence was higher among under nourished (< 5th percentile) with 66.7% [23].
In the present study, prevalence of anaemia was higher among those who were occasional hand washers after toileting 43.8% and before food intake 29.3%.
In this study, occasional foot wear users had higher proportion of anaemia (50%) when compared to regular users (19.8%). Poor hand hygiene and improper foot wear usage are the important factors which favor worm infestation among adolescents which in turn leads to anaemia. In the present study prevalence of worm infestation among study subjects were (52/132) 40.2% it comes under mild prevalence area as per WHO guidelines [24]. This is lower than the study conducted in Madhya Pradesh with 57% [25] and in Tamilnadu 63% [26]. Prevalence of anaemia among those who had ova or cyst in their stool sample was (29/53) 54.7% compared to stool negative subjects with only (23/79) 29.1%. This result was concordant with the study conducted in Madhya Pradesh with 83% among stool positive subjects and 53% among stool negative subjects [25].
A significant association between anaemia and factors like personal hygiene (hand hygiene and footwear usage) and worm infestation shows the area needed to be focused among adolescent girls. A programme focusing on improving personal hygiene and periodical deworming is needed for them.
Limitation
Food frequency questions were asked retrospectively so there is a chance for recall bias.
Only 132 adolescent girls were given their stool sample for examination. Hence data regarding the stool sample were missing for rest of them.
Conclusion
Prevalence of anaemia was found to be 21% among the study population. The major factors associated with anaemia were menstruation, improper personal hygiene like hand washing before food intake and after toileting, worm infestation, improper foot wear usage and decreased intake of jaggery. Information, Education and Communication (IEC) activities regarding personal hygiene and promotion of healthy nutritional practices should be implemented. Promotion of proper utilization of iron and folic acid supplementation via Weekly Iron and Folic Acid Supplementation (WIFS) programme and biannual deworming are recommended.
*Packed cell volume, † Mean Corpuscular Volume, ‡ Mean Corpuscular Haemoglobin, § Mean Corpuscular Haemoglobin Concentration