The loss of protective airway reflexes and obstruction of the upper airway after general anaesthesia can be potentially life-threatening [1]. With the advent of supra-glottic airway devices such as the Proseal Laryngeal Mask Airway (PLMA) which not only provides a tight seal against glottis without increasing mucosal pressure but also has a port for gastric drain tube that prevents aspiration of gastric contents [2].
Untoward effects such as gagging, swallowing, coughing, laryngospasm and movements of the head and limbs may occur while inserting PLMA if adequate jaw relaxation and suppression of airway reflexes is not attained [3]. Various induction agents such as Thiopentone sodium [4], sevoflurane [3], propofol [3] have been used in the past for smooth insertion of PLMA. Propofol has a short duration of action and adequately suppresses pharyngeal and laryngeal reflexes. However, it causes dose-dependent cardio-respiratory depression [5] and still causes undesirable events when used alone for PLMA insertion. Different adjuvants such as opioids, benzodiazepines, low dose muscle relaxants etc., [6–8] have been used with propofol to improve insertion conditions of PLMA. However, opioids may increase and enhance the respiratory depression and haemodynamic depression of propofol. Selective alpha-2 agonist, dexmedetomidine has been used for co-induction with propofol to evaluate the insertion conditions of Classic LMA.
In the present study, we aimed to evaluate the effects of dexmedetomidine versus fentanyl with propofol co-induction on insertion conditions of PLMA and total propofol requirement using the Modified Scheme of Lund and Stovener insertion criteria.
Materials and Methods
After the institutional ethics committee approval, this prospective randomized double-blind study was conducted in 60 ASA I and II patients of either sex scheduled for short surgical procedures under general anaesthesia from January 2013 to January 2014 were included. Patients with neck and facial burns, reduced mouth opening, BMI≥30, on B-blocker therapy, basal heart rate ≤60 and known egg allergy were excluded from the study.
Patients were randomly divided into two groups Group D receiving dexmedetomidine with propofol and Group F receiving fentanyl with propofol using block method of randomization. Participants were recruited in 6 different blocks as follows: FFDD, FDFD, FDDF, DFF, DFDF, DDFF. It was ensured that half of the participants within each block were allocated to group D and other half to group F. The next step was to randomly select amongst these 6 blocks. The random selection was done by pulling out chits that were numbered from 1-10. A sequence of random numbers was drawn and noted by the statistician. Since there were only six different blocks, all numbers outside the range of 1 to 6 were dropped. The investigator as well as the patient was blinded to this sequence.
After the written informed consent, patient was wheeled inside the operation theatre and baseline heart rate, mean arterial pressure, oxygen saturation and respiratory rate were noted. Premedication with glycopyrrolate was administered and study drug,1μg/kg (dexmedetomidine in Group D or fentanyl in group F) was given slowly intravenously by an infusion pump over 10 minutes, by anaesthesia personnel not involved in the study. Midazolam 0.02mg/kg was then given over four minutes intravenously in either group.
Following preoxygenation for 5 minutes after stopping study drug infusion, patient was induced with propofol upto 2.5mg/kg till clinical end point of induction i.e., loss of eyelash reflex followed by centralisation of pupils was achieved [9] which indicated an adequate depth of anaesthesia for airway manipulation. A blinded investigator with experience of atleast 50 PLMA insertions inserted the PLMA (Introducer- technique [10]) in “sniffing morning air” position. A 12 F Gastric drain tube was inserted through the PLMA after confirming gas leak during ventilation by placing a bolus of clear water-soluble lubricanton its proximal end. The confirmation of gastric tube placement was done by auscultation of epigastric air when injected through its proximal end. Ease of insertion of PLMA was assessed by the extent of jaw relaxation by “Young’s criteria” [Table/Fig-1].
Jaw relaxation according to Young’s criteria.
| Absolutely relaxed muscle tone | I |
| Moderately relaxed muscle tone | II |
| Poorly relaxed muscle tone | III |
The overall PLMA insertion conditions were assessed with respect to swallowing, gagging, coughing, head or limb movements, lacrimation, laryngospasm etc., according to “Modified Scheme of Lund and Stovener” [Table/Fig-2]. If any of these were present at the first attempt of PLMA insertion, a further dose of 0.5mg/kg of propofol was administered. Time taken for PLMA insertion was calculated from the induction till the confirmation of correct PLMA positioning. Anaesthesia was continued with 1.5% isoflurane and oxygen-nitrous oxide 50:50 on spontaneous-assisted mode of ventilation.
Overall insertion conditions by Modified scheme of Lund and Stovener.
| Coughing and gagging | Grade I (nil) | Grade II (mild) | Grade III (severe) |
| Laryngospasm | Grade I (nil) | Grade II (mild) | Grade III (severe) |
| Limb and head movements | Grade I (nil) | Grade II (mild) | Grade III (severe) |
| Overall PLMA insertion conditions |
| Excellent: No gagging or coughing, no laryngospasm, no patient movement |
| Good: mild to moderate gagging or coughing, no laryngospasm, mild to moderate patient movement |
| Poor: Moderate to severe gagging or coughing, no laryngospasm, moderate to severe patient movement |
| Unacceptable: Severe gagging or coughing, laryngospasm, severe patient movement |
Haemodynamic parameters during PLMA insertion were also noted at intervals of baseline, 1, 3, 5, 10, 15 and 20 minutes. At the end of surgery, PLMA was removed when the patient was able to open mouth on command and was inspected for blood stains. The mask of airway was inspected with the litmus paper for any gastric contents to rule out regurgitation. Any injury to lips, teeth and tongue was also noted.
Mean and standard deviation for all the values were calculated and compared between two groups D and F. The demographic data was analysed using Mann Whitney-test and Fisher-exact test. Ordinal categorical data such as PLMA insertion conditions and number of attempts were analysed by Fisher-exact or Chi-square test and haemodynamic parameters were analysed using the unpaired t-test or Mann-Whitney test. A p-value <0.05 was accepted as statistically significant.
Results
With reference to the demographic data such as age (p=0.23), gender (p= 0.99), height (p=0.66), weight (p=0.68), and BMI (p=0.39), both the groups were comparable. Adequacy of mouth opening and difficult airway assessment was done by the Modified Mallampatti Test which was comparable (p=0.36), the groups D and F.
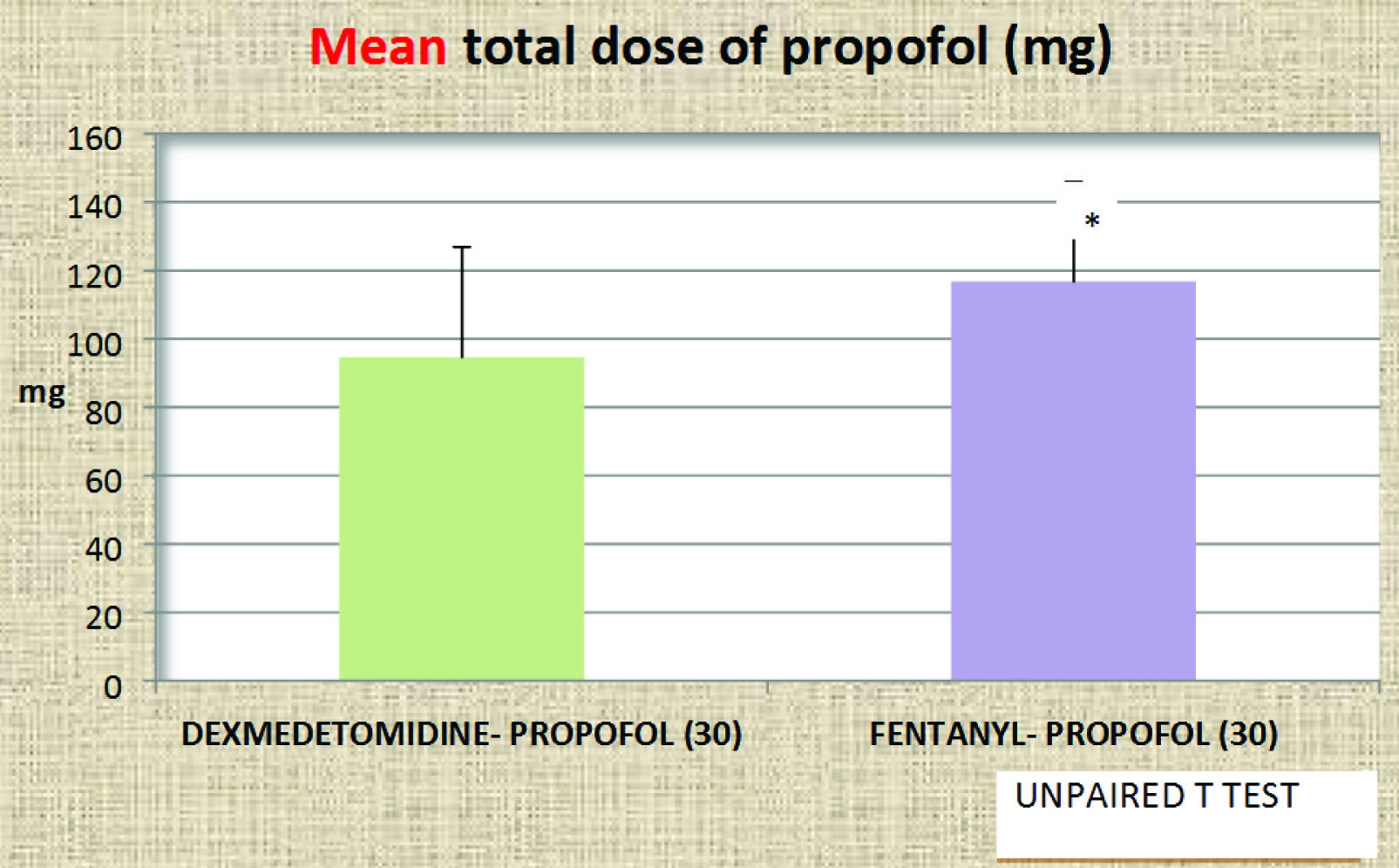
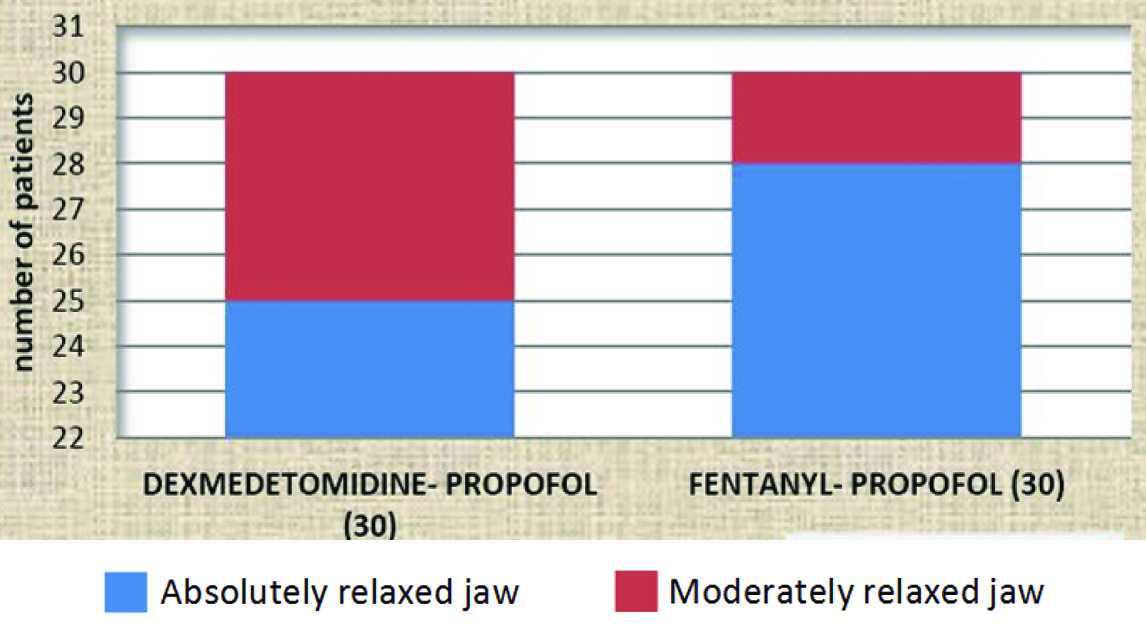
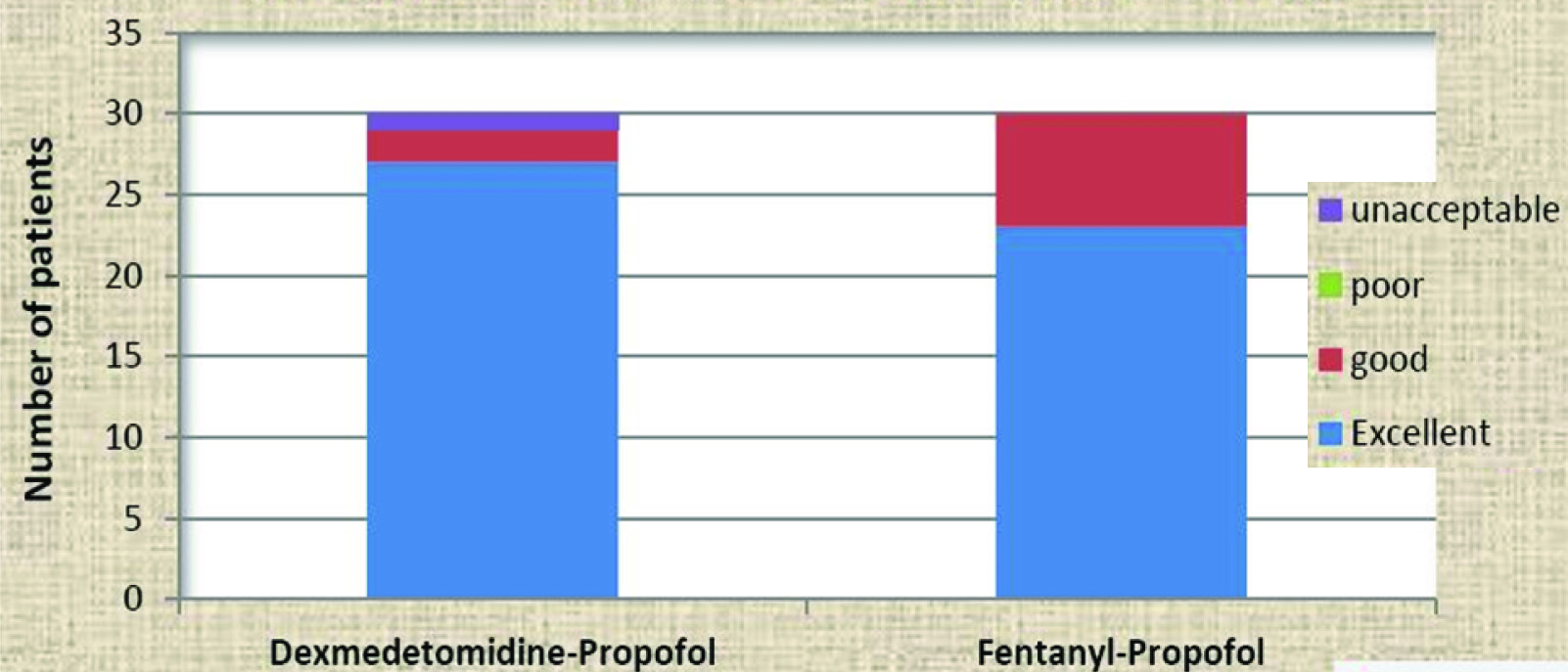
Induction dose and increments of propofol required in group D was significantly lower (p<0.001), than in group F [Table/Fig-3]. Apnoea, more than 30 seconds, after induction occurred in both groups and was comparable. Three cases in group D and six in group F required two attempts for PLMA insertion. Jaw relaxation as assessed by Young’s criteria was comparable (p=0.41), between the two groups [Table/Fig-4]. The overall PLMA insertion conditions as assessed by the “Modified scheme of Lund and Stovener” were also comparable and statistically not significant (p=0.12), between groups D and F [Table/Fig-5]. The ease of gastric tube insertion in the two groups was comparable.
Mean total dose of propofol [Induction dose + Incremental dose] in mg in group D and group F.
Comparison of Jaw relaxation by Young’s Criteria between groups D and F (Fischer’s-exact test).
Comparison of Overall insertion conditions by Modified scheme of Lund and Stovener between groups D and F (Chi-square test).
Haemodynamically, heart rate variation and mean arterial pressure were not statistically significant between two groups. Evidence of trauma to lips during PLMA insertion was noted in 2 patients of group F but was not statistically significant.
Discussion
PLMA is a relatively new device providing a good glottic seal at low mucosal pressure and facilitates insertion of a drain tube and hence, preferred for positive pressure ventilation. Its insertion necessitates adequate depth of anaesthesia, jaw relaxation and mouth opening.
Different induction agents like thiopentone sodium, propofol, etomidate and sevoflurane have been used for safe insertion of PLMA [3–5]. In the studies conducted by Parasa and Bapat et al., propofol was found to be a better induction agent for PLMA insertion as compared to thiopentone sodium [11,12]. Moreover, Krishnappa et al., found that 2.55 mg/kg of propofol gave adequate LMA insertion conditions in terms of absence of motor response to jaw thrust [13]. Propofol when used singly requires a very high dose for achieving satisfactory insertion conditions but such high doses can cause cardiorespiratory depression [14]. Addition of co-induction agents such as benzodiazepines, opioids, ketamine or low dose muscle relaxants to propofol have provided better jaw relaxation without significant haemodynamic changes [8,15,16].
We have compared fentanyl and dexmedetomedine as co-induction agents with propofol to have optimal PLMA insertion conditions. Dutt et al., and ASB Tan et al., in their respective studies found that 1 μg/kg of fentanyl gave more haemodynamic stability than a higher dose of 2 μg/kg while having similar insertion conditions [17,18]. F Uzumcugil found comparable LMA insertion conditions using dexmedetomidine and fentanyl along with propofol [19]. In our study, we administered dexmedetomidine in group D and fentanyl in group F at the rate of 1μg/kg over ten minutes. Anxiolysis with 0.02mg/kg midazolam was given over four minutes after the infusion. The sequence of drug dosing and timings were adjusted to attain peak onsets at similar range of time for PLMA insertion.
We required a significantly lower mean induction dose of propofol of 91.52±27.81mg (1.54±0.26mg/kg) in group D as compared to group F 111.15±24.25 mg (1.86±0.27mg/kg). We found a reduction in the requirement of induction dose of propofol below our maximum pre-decided dose of 2.5 mg/kg following both fentanyl and dexmedetomidine. As compared to previous studies [6,18,19] which suggested an induction dose of propofol as 2.5 mg/kg for optimal insertion conditions for LMA, we required lesser dose probably because our end point of propofol induction was centralization of pupils as against jaw relaxation.
Three patients in group D and six in group F required a second attempt for PLMA insertion. This is in contrary to the study by Lande et al., where only one patient of dexmedetomidine group had a second attempt and five from fentanyl group [20]. After each unsuccessful attempt, an incremental dose of 0.5 mg/kg each of propofol was given. Patients who required more than three attempts were excluded from the study. The total dose of propofol (i.e., induction dose + incremental dose) was significantly higher in the group F as compared to group D. This may also be due to the more number of patients requiring second attempt in group F.
PLMA insertion conditions were assessed only after the first attempt by the Young’s criteria [Table/Fig-1]. The overall conditions were summed up by the Modified scheme of Lund and Stovener [21]. In our study, 28/30 patients of group F and 25/30 in group D had absolutely relaxed jaw. Four out of five patients in group D who had moderately relaxed jaw had BMI of >25 kg/m2 which could explain the jaw relaxation criteria between study groups. This was an incidental finding in our study which is discordant with findings of Lande et al., that stated the dexmedetomidine group had a more relaxed jaw than fentanyl group [20].
In the present study, 3 out of 30 patients from group F had single episode of mild coughing during PLMA insertion while no patient from group D had coughing. Though statistically not significant, they are clinically significant episodes of coughing probably provoked by intravenous fentanyl rather than simply being a response to PLMA insertion. Gupta et al., had 13 out of 30 and 1 out of 30 in fentanyl group who experienced mild and severe coughing respectively [21]. Wong CM et al., in his study stated that a higher dose of fentanyl notably induces coughing [22]. Limb and head movements which occurred in few patients did not hamper the insertion of PLMA in our study. Laryngospasm was noted in one case of group D that could have occurred due to lighter planes of anaesthesia which disappeared after incremental propofol.
Similar to findings of apnoea in the study by Jayaram et al., there was higher incidence of apnoea in fentanyl group in our study too [14]. However, the percentage of patients with apnoea in our study was lower than that in former study because we required smaller induction dose of propofol.
Dexmedetomidine and fentanyl have been used for attenuating haemodynamic responses to laryngoscopy and intubation [23]. We found that heart rate decreased in both study study groups from baseline after their infusion but there was a transient rise in heart rate during PLMA insertion followed by a reduction below the baseline heart rate. The rise in heart rate was higher in fentanyl group as compared to dexmedetomidine group and this finding was similar to study by Lande et al., [20]. Mean arterial blood pressure changes were comparable between the two groups. There was no evidence of gastric regurgitation as assessed by the litmus test upon removal of PLMA.
Limitation
Assessment of the depth of anaesthesia for PLMA insertion using BIS monitor would have been a more appropriate alternative. However, it was not feasible in our set up due to its non-availability at the time when the study was conducted. Similarly, PLMA insertion conditions may be assessed more accurately by the effect-site concentration of propofol using target controlled infusion.
Conclusion
Propofol is the suitable induction agent of choice for insertion of a supraglottic airway device such as the PLMA. When used singly, higher dose is required and that can give rise to haemodynamic instability. Dexmedetomidine 1μg/kg as co-induction agent with propofol not only gives excellent overall insertion conditions and haemodynamic stability but also significantly reduces the requirement of induction as well as incremental doses of propofol.