An Unusual Case of Septic Arthritis of the Hip
Ujjwayini Ray1, Soma Dutta2, Arpita Sutradhar3
1 Consultant, Department of Microbiology, Apollo Gleneagles Hospitals, Kolkata, West Bengal, India.
2 Junior Consultant, Department of Microbiology, Apollo Gleneagles Hospitals, Kolkata, West Bengal, India.
3 Junior Consultant, Department of Pathology, Apollo Gleneagles Hospitals, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ujjwayini Ray, Consultant, Department of Microbiology, Apollo Gleneagles Hospitals, Kolkata-700054, West Bengal, India.
E-mail: dr_uray@rediffmail.com
Non-typhoidal Salmonella, particularly Salmonella enterica serovar typhimurium is food borne pathogen causing mild self-limiting diarrhoea in healthy adults. It can occasionally cause extraintestinal focal infection in susceptible patients. Salmonella, as the aetiological agent of osteomyelitis and septic arthritis is rare and has been mostly reported in patients with sickle cell disease or thalassaemia. We report a case of septic arthritis by Salmonellatyphimurium in an immunocompromised patient who was successfully treated following timely isolation and identification of the aetiological agent.
Immunocompromised, Non-Typhoidal Salmonella, Salmonella typhimurium
Case Report
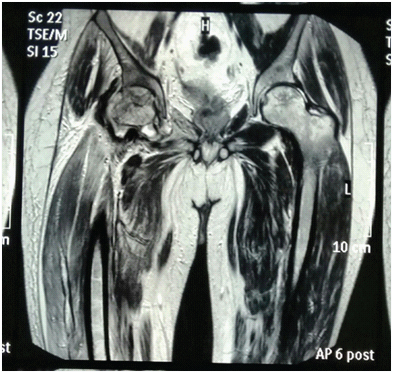
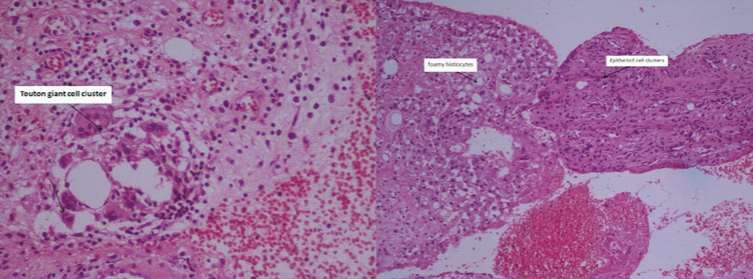
A 39-year-old male patient of right tempero-parietal high grade glioma who completed treatment two months back (surgery followed by chemotherapy and radiotherapy) presented with one week of severe pain and swelling in the right hip region radiating towards the foot accompanied by fever and chills. There was no history of local trauma, diarrhoea, dysentery, vomiting, pain abdomen in the recent past. Laboratory investigations revealed an elevated Erythrocyte Sedimentation Rate (ESR) (97mm in 1sthour) and rest all other haematological parameters were unremarkable (WBC count 7980mm3, neutrophils 72%). Magnetic Resonance Imaging (MRI) of the hip joint showed bilateral avascular necrosis of the hip joints with effusion and inflammatory changes in the right hip joint [Table/Fig-1]. The patient was taken up for surgery and synovectomy of the right hip joint was done with debridement of necrotic tissue. Histopathological examination of the debrided tissue showed mixture of acute and chronic inflammatory cells with a few ill-defined granulomas suggestive of a possible tubercular aetiology [Table/Fig-2]. Culture of the debrided tissue in Mac-Conkey’s agar grew gram negative non lactose fermenting bacilli after overnight incubation at 37°C. The bacterium was identified as Salmonella species by conventional biochemical reactions and agglutination with group specific antisera (Salmonella Poly O and Poly H) as well as by the automated system (Vitek, Biomerieux). The organism was further characterized as Salmonella enterica subspecies enterica serovar typhimurium (Salmonella poly O, Group 04, Hi; 1,2) by National Institute of Cholera and Enteric Diseases (NICED), Kolkata. In-vitro susceptibility testing by the broth microdilution method using the VITEK system revealed susceptibility to cetazidime, cefepime, minocycline and moderately susceptible to ciprofloxacin and levofloxacin. The strain was susceptible to ampicillin, chloramphenicol, tetracycline, co-trimoxazole, cefotaxime, ceftriaxone and resistant to nalidixic acid according to the Kirby-Bauer disc diffusion method. Blood, urine and stool cultures and Human Immunodeficiency Virus (HIV) test were all negative. Haemoglobin electrophoresis did not reveal any haemoglobinopathies.
MRI picture shows collapse of the femoral head associated with oedema of the femoral head and neck, and of the acetabular region of the right hip along with oedema of the right thigh and pelvic muscles indicative of infective aetiology. There is also avascular necrosis of the left femoral head.
Multiple sections show several haemorrhagic areas surrounded by foamy and epitheloid histiocytes and touton giant cells against a background of dense mixed acute and chronic inflammatory cells.
Following isolation of S. typhimurium, the initial antibiotics were replaced with ceftriaxone (1g i.v. OD). The patient gradually improved over the next few days with subsidence of fever and pain. The patient was discharged after two weeks of ceftriaxone therapy. At the time of discharge the patient was able to walk with the help of a walker. He was advised to continue ceftriaxone for two more weeks followed by oral amoxicillin (500mg QDS) for four months. Radiographic examination revealed satisfactory outcome at 6 months follow-up.
Discussion
Non Typhoidal Salmonellosis (NTS) typically manifests as self-limiting enterocolitis, with approximately 5% of individuals developing bacteremia. Typhimurium is one of the top three serotypes isolated worldwide over many decades from humans, domestic and wild animals, food stuffs and the environment with cattle and poultry being important sources of infection for humans [1].
The most important risk factors for invasive infection with non-typhoidal Salmonella in low income countries like sub Saharan Africa are HIV infection in adults, and malaria, HIV, and malnutrition in children [2]. In high income countries, non-typhoidal Salmonella bacteraemia is mostly seen in patients who are immunosuppressed because of HIV infection, steroid use, malignancy, chronic renal or liver disease and diabetes [3]. Patients with underlying structural abnormalities, such as valvular heart disease, aneurysms or atherosclerosis, biliary or urinary tract abnormalities, bony abnormalities, or prostheses are at risk of developing focal or metastatic infection with non-typhoidal Salmonella at these sites [4]. Invasive infection with non-typhoidal Salmonella may prove to be fatal. Invasive strains of non-typhoidal Salmonella are one of the predominant causes of blood stream infection in African adults and children with associated case fatality of 20%-25% [2]. In a hospitalised case series from Spain which is one of the developed countries, mortality in adults was found to be around 12.2% [5]. Amongst the extra intestinal complications, osteomyelitis and septic arthritis due to Salmonella (typhi and non typhi combined) is estimated to be less than 1% and 0.1% to 0.2% respectively [6]. In the present case, it is likely that a mild gastrointestinal infection which went unnoticed led to occult bacteraemia in an immunocompromised patient resulting in focal infection of a damaged joint (patient had bilateral avascular necrosis of the femoral head, possibly as a complication of high dose steroids which he received for his primary condition). Salmonella sp. has predilection for bones and joints is evident from the large number of cases of osteomyelitis due to this bacteria (both typhoidal and non-typhoidal) reported in the literature [7]. Salmonellaosteomyelitis is a well-known entity in children with sickle cell disease [8]. Jones TF et al., has reported an incidence of 0.04% for bone and joint infections due to non-typhoidal Salmonellosis in the United States [9]. Although incidence of Salmonella infection is on the decline in the developed world through improvement in food hygiene and provision of safe drinking water but it is still a major problem for the developing countries [10].
The laboratory markers of pyogenic infection such as leukocytosis and neutrophilia is often absent in sepsis due to Salmonella species [11]. Leucocytosis which is seen in septic arthritis is often absent in Salmonella infection and histopathological examination may mimic chronic infections such as tuberculosis [12]. So, isolation and identification of the organism becomes important for optimum management. Another area of concern is the growing incidence of drug resistance in Salmonella sp., quinolone resistance is widespread and so is the occurrence of multi drug resistant strains (resistance to chloramphenicol, amoxycillin, doxycycline, cotrimoxazole). Ceftriaxone is considered the drug of choice for invasive infection but there are reports of emergence of extended spectrum beta-lactamase producing strains in Salmonella [13,14]. In the present case, the strain showed reduced susceptibility to ciprofloxacin but retained sensitivity to other group of drugs. So ceftriaxone followed by the oral amoxycillin was prescribed to eliminate the infection. In our patient, identifying the bacterial strain and performing antibiotic susceptibility contributed to choosing the appropriate antibiotic for the successful eradication of infection. Salmonellosis in humans is generally contracted through the consumption of contaminated food of animal origin (mainly eggs, meat, poultry and milk), although other foods, including green vegetables contaminated by manure, have also been implicated in its transmission. Basic food hygiene practices, such as "cook thoroughly", is recommended as a preventive measure against Salmonellosis. Avoidance of raw milk and products made from raw milk is also advocated.
Conclusion
NTS, a food borne pathogen and causative agent of self limiting diarrhoea of healthy adults can cause serious infections in patients with underlying risk factors. Bone and joint infections are particularly debilitating as they require surgical interventions and prolonged courses of antibiotic therapy. The emergence of antibiotic resistance in this group of bacteria has further compounded the problem. Food counselling should be part of the medical care of these high risk patients to avert such potentially debilitating infections.
[1]. Palmer SR, Rowe B, Trends in Salmonella infectionsPHLS Microbiol Digest 1985 3:18-21. [Google Scholar]
[2]. Feasey NA, Dougan G, Kingsley RA, Heyderman RS, Gordon MA, Invasive non-typhoidal Salmonella disease: An emerging and neglected tropical disease in AfricaLancet 2012 379(9835):2489-99. [Google Scholar]
[3]. Gordon MA, Salmonella infections in immunocompromised adultsJ Infect 2008 56:413-22. [Google Scholar]
[4]. Cohen JI, Bartlett JA, Corey GR, Extra-intestinal manifestations of Salmonella infectionsMedicine (Baltimore) 1987 66:349-88. [Google Scholar]
[5]. Galofré J, Moreno A, Mensa J, Analysis of factors influencing the outcome and development of septic metastasis or relapse in Salmonella bacteremiaClin Infect Dis 1994 18:873-78. [Google Scholar]
[6]. Pegues DA, Miller S, Salmonella species, including typhoid feverIn Principles and Practice of Infectious Diseases 2010 Seventh editionNew YorkChurchill Livingstone Inc:2887-2903.Edited by Mandell GE, Douglas RG, Bennett JE [Google Scholar]
[7]. Chen PL, Lee HC, Lee NY, Wu CJ, Lin SH, Shih HI, Non-typhoidal Salmonella bacteraemia in elderly patients: An increased risk for endovascular infections, osteomyelitis and mortalityEpidemiol Infect 2012 140(11):2037-44. [Google Scholar]
[8]. Adeyokunnu AA, Hendrickse RG, Salmonella osteomyelitis in childhood. A report of 63 cases seen in nigerian children of whom 57 had sickle cell anaemiaArch Dis Child 1980 55:175-184. [Google Scholar]
[9]. Jones TF, Ingram LA, Cieslak PR, Vugia DJ, Tobin-D’Angelo M, Hurd S, Salmonellosis outcomes differ substantially by serotypeJ Infect Dis 2008 198:109-14. [Google Scholar]
[10]. Salem KH, Salmonella osteomyelitis: A rare differential diagnosis in osteolytic lesions around the kneeJ Infect Public Health 2014 7(1):66-69. [Google Scholar]
[11]. Ao TT, Feasey NA, Gordon MA, Keddy KH, Angulo FJ, Global burden of invasive nontyphoidal Salmonella disease, 2010Emerg Infect Dis 2015 21(6):941-49. [Google Scholar]
[12]. Szilagyi A, Mendelson J, Portnoy J, Miller B, Caseating granulomas in chronic osteomyelitis: salmonellosis, tuberculosis or both?Can Med Assoc J 1979 120:963-65. [Google Scholar]
[13]. Chen HM, Wang Y, Su LH, Chiu CH, Nontyphoid Salmonella infection: microbiology, clinical features, and antimicrobial therapyPediatr Neonatol 2013 54:147-52. [Google Scholar]
[14]. Dunne EF, Fey PD, Kludt P, Reporter R, Mostashari F, Shillam P, Emergence of domestically acquired ceftriaxone-resistant Salmonella infections associated with AmpC β lactamaseJAMA 2000 284:3151-56. [Google Scholar]