Introduction
Abdominal aortic disease is an important cause of clinical disability that requires early detection by imaging methods for prompt and effective management. Understanding regional disease pattern and prevalence has a bearing on healthcare management and resource planning. Non-invasive, conclusive imaging strategy plays an important role in the detection of disease. Multi-Detector Computed Tomography (MDCT) with its technological developments provides affordable, accurate and comprehensive imaging solution.
Aim
To evaluate regional demography of abdominal aortic disease spectrum detected using MDCT imaging data in a tertiary hospital.
Materials and Methods
A descriptive study was conducted based on MDCT imaging data of patients who were investigated with clinical diagnosis of abdominal aortic disease, from March 2008-2010, over a period of 24 months. Patients were examined with the contrast-enhanced MDCT examination. Morphological diagnosis of the aortic disease was based on changes in relative aortic caliber, luminal irregularity, presence of wall calcification, dissection or thrombus and evidence of major branch occlusion. Patients were categorized into four groups based on imaging findings. MDCT information and associated clinical parameters were examined and correlated to management of patient. Descriptive statistical data, namely mean, standard deviation and frequency of disease were evaluated.
Results
A total of 90 out of 210 patients (43%) were detected with the abdominal aortic abnormality defined by imaging criteria. Group I, comprising of patients with atherosclerosis –including those with complications, constituted 65.5% of the patients. Group II represented patients with aneurysms (45.5%). Group III, consisting of 32.2% of the patients, contained those with dissections. The rest of the patients, including patients with aorto-arteritis, were classified as group IV. Eight patients with aneurysm and one patient with aorto-arteritis were considered for surgical treatment. Ten patients with dissection underwent endovascular procedure. Rest of the patients was managed conservatively.
Conclusion
Aortic disease was observed in 43% of investigated patients. Atherosclerosis with and without aortic aneurysm constituted the largest group. MDCT provided comprehensive information about the lesion and associated complications. In view of the wider availability and desired imaging qualities, MDCT provided optimal information for diagnosis and management of aortic pathology. Majority of our patients (90%) were treated conservatively.
Introduction
The abdominal aorta is a major vascular structure, integrity of which ensures the viability and function of vital abdominal organs and caudal half of the body. Subtle abnormality in the abdominal aorta and its branches can be reflected in the end organs, can present as either acute or chronic condition. Wide spectrum of diseases can be seen in abdominal aorta; some commonly encountered entities include atherosclerosis, aneurysm, dissection and aorto-arteritis [1–7]. Aetiology and classification of abdominal aortic disease confirms to pattern of disease in rest of vascular tree. Often classification of thoracic and abdominal aortic disease is grouped together in view of similarity of disease spectrum [8]. List of entities are presented in [Table/Fig-1], based on the recommendation of European society of Cardiology publication on aortic disease [8]. In the present study grouping of patients was based on the classification, minimally modified to suit regional disease spectrum. Imaging information helps to stratify disease for management purpose and identify lesions that lead to complication. Imaging also plays an important role in early detection (screening) and follows up of these conditions. Essentially anatomic imaging is required for abdominal aorta, either needed as a screening tool for screening aneurysm in high-risk patients or as a definitive procedure for diagnosing aortic disease.
Classification of abdominal aortic disease.
| Category | Entities |
|---|
| Genetic diseasesaffecting the aorta | Marfans syndrome |
| Ehlers Danlas Syndrome |
| Turner syndrome |
| Arterial Tortuosity Syndrome |
| Coarctation of aorta |
| Atherosclerotic lesions of the aorta | Thromboembolic aortic disease |
| Mobile aortic thrombosis |
| Atherosclerotic aortic occlusion |
| Calcified aorta |
| Acute thoracic aortic syndrome | Acute aortic dissection |
| Intramural haematoma |
| Penetrating aortic ulcer |
| Aortic pseudoaneurysm |
| Traumatic aortic injury |
| Iatrogenic aortic dissection |
| Aortic aneurysms |
| Aortitis | Takayasu Disease |
| Becet’s Disease |
| Giant cell arteritis |
| Buerger disease, Kawasaki disease, |
| Aortic tumours | Angiosarcoma, Leiomyosarcoma |
(Adapted from the ESC 2014 guidelines on aortic disease [8]).
Invasive contrast study of aorta is the gold standard for anatomic imaging technique. High-spatial (0.1–0.2 mm) and temporal (10 mSc) resolution provided by the technique is not yet achieved by noninvasive techniques [9]. Invasive angiography becomes necessary for guiding proper management. New technical developments of Multi-Detector Computed Tomography (MDCT) scanners have made non-invasive computed tomography a comprehensive, affordable, practical, technology [10–13]. State of the art MDCT provides major advantages over earlier CT techniques and conventional angiography, by allowing acquisition of large volume of thin-sections within a short breath hold during contrast injection [14–18]. MDCT utility has been further supplemented by versatile, fast volumetric post-processing techniques, like Maximum-Intensity Projection (MIP), Curvilinear Reformation (CVR), Volume Rendering (VR), Surface Shaded Display (SSD) and Virtual Intravascular Endoscopy (VIE) [14,16,19].
MDCT generally serves as one-stop shop from diagnostic standpoint. Small number of patients may need additional catheter angiography, when a specific issue like small vessel occlusion has to be sorted out. This presentation presents a spectrum of diseases of the abdominal aorta at a tertiary hospital setup evaluated by MDCT angiography. MDCT angiography is preferred over MRA for anatomic imaging of abdominal aorta, although MRA has definite advantage in young women to avoid radiation exposure, in patients with renal impairment and postoperative/poststent imaging. Generally MRI technique includes gated or non-gated free-breathing 3D volume acquisition. High-field MR, 16-32-channel coils with high parallel imaging decrease image acquisition time. T1/T2 spin/gradient preparations and different pulsed sequences to increase signal/contrast-to-noise ratios. High-resolution non-contrast bright- blood techniques provide high contrast diagnostic images without the need for potentially nephrotoxic contrast agents [9]. Contrast enhanced MRA is an additional tool for global vascular assessment when there are no contraindication for contrast.
Aim
The present study was carried out to evaluate regional demographic assessment of abdominal aortic disease spectrum, in a tertiary hospital setting using MDCT imaging data.
Materials and Methods
A descriptive study was performed from March 2008-March 2010 over a period of 24 months. MDCT imaging data of patients were analysed for imaging diagnosis of abdominal aortic disease. The study was approved by the institutional review board.
CT was performed with GE Light speed, VCT. (GE Medical systems Milwaukee, Wisconsin, USA). Technical parameters were as follows: KV-120, effective mAs 250–790, time-0.35sec, detector collimation - 0.625mm, Slice Thickness-0.625-5mm, Matrix size 512 x 512. Examination was performed without oral contrast. Iohexol 350mg/ml or low osmolar (visipaque) contrast medium was used. A total of 1.2ml/kg body weight, of contrast was injected at the rate of 3.5-4.5 ml/second using Mallinckrodt optistat pressure injector. An 18-gauge intravenous canula was used for contrast injection, preferably in the left antecubital vein. Data was processed on GE advanced workstation, Advantage Windows 4.2 P. Conventional axial images, 3-Dimentional (3D), Multi-Planar Reformations (MPR) sagittal, oblique views, coronal, thick and thin Maximum Intensity Projection (MIP), volume rendered images and vessel analysis techniques were utilized. Patients who had contraindication for contrast CT examination or radiation procedure were excluded. Morphological diagnosis of the aortic disease was based on changes in relative aortic caliber, luminal irregularity and presence of wall calcification, dissection or thrombus and evidence of major branch occlusion. Patients were categorized into four groups based on imaging findings:
Group I - Showing changes of atherosclerosis.
Group II - Patients with aortic aneurysm.
Group III - Consisting of aortic dissection.
Group IV- Consisting of patients with aorto-arteritis, other aortic disease and postoperative patients.
The non-imaging data, which consisted of the diabetic status, blood pressure correlation and lipid profile, were obtained for all patients. Patients who were considered for surgical management and needed additional information underwent conventional angiography.
Results
Total of 210 patients were investigated for abdominal aortic disease. Patients with normal abdominal aorta or those with minor plaques, calcification or reduction of aortic lumen less than 30% were excluded from the study. A total of 90 patients were diagnosed with significant abdominal aortic abnormality based on predefined imaging criteria [Table/Fig-2,3].
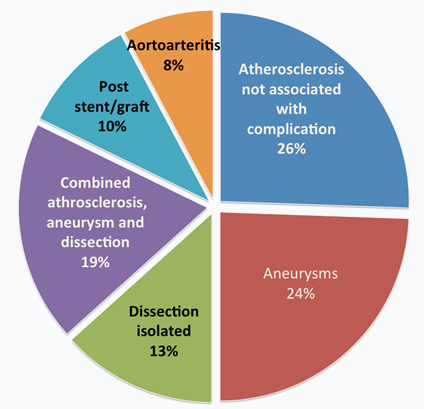
Shows relative incidence of abdominal aortic disease.
| Type of disease | Number | Percentage % |
|---|
| Group I: Atherosclerosis (Total) | 59 | 65.5% |
| Atherosclerosis not associated with complications | 23 | 25.5% |
| Atherosclerosis associated with complications | 36 | 40.0% |
| Group II Aneurysms (Total) | 41 | 45.5% |
| Aneurysms | 22 | 24% |
| Aneurysm associated with dissection | 17 | 18.8% |
| Aneurysm with aorto-arteritis | 2 | 2.2% |
| Group III: Dissection(Total) | 29 | 32.2% |
| Dissection isolated | 12 | 13.3% |
| Dissection associated with aneurysm | 17 | 18.8% |
| Combined aneurysm and dissection | 17 | 18.8% |
| Group IV: Post stent/graft | 9 | 10.0% |
| Aortoarteritis | 7 | 7.7% |
| Total | 90 | 100% |
Pie chart showing distribution of aortic disease spectrum.
In the study, cohort 80% were males and 20% were female. Age range was 40-80yrs, 34.7% in 61-70 years and 26% in 41-50 years group. Rest as nearly equal number of cases in 31-40, 51-60 and 71-80 years age group. Overall 56/90(57.7%) patient had history of DM. HTN and smoking history was seen in 46/90 (51.1%) and 42/90(46.6%), respectively. Dyslipidemia was seen in 32/90(35.5%).
Diffuse atherosclerosis was seen in 59/90(65.5%) patients in association with aneurysms, dissections and in poststent-graft patients. A total of 57 patients (96.6 %) showed involvement of infra-renal segment [Table/Fig-4] with renal and suprarenal segmental involvement in 55 (93.2%) and 52 (88.1%) patients respectively. Penetrating atherosclerotic ulcers were seen in 9 cases, located at infra-renal segment (77.7%), renal (55.5%) and suprarenal segmental (33.3%) respectively [Table/Fig-5]. Fusiform aneurysms were most frequent (90.24%) [Table/Fig-6] and saccular aneurysms were seen in 9.7% cases [Table/Fig-7]. Infra-renal aorta was the most common segment involved Mural thrombus was seen in 58.5%. Wall calcifications were seen in 65.8% patients. Impending and contained ruptures were seen in 2 patients each (4.8%). Rupture was seen in only 1 patient (2.4%). Dissection was seen in 29/90 (32.2%), predominantly in male (75.8%) [Table/Fig-8]. Type A dissection was found in 20/29 (69%) [Table/Fig-9], Type B dissection was seen in 9/29 (31%) cases. Enhancement of the false lumen was seen in 27 (93.1%) and true lumen in 24 (82.7%). Continuity of false lumen with true lumen was established in 21 (72.4%) cases. Displacement intimal calcification was observed in 17/29 (58.6%) cases. Thrombosis of false lumen was seen 31% and true lumen was seen 20.6% [Table/Fig-10a]. Cobwebs were seen in only 13.7% cases. Right renal artery was the most common occluded vessel [Table/Fig-10b], involved in 37.9% cases; followed by 27.5% occlusion of left renal artery.
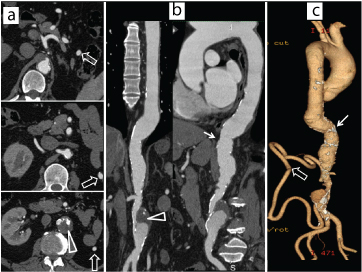
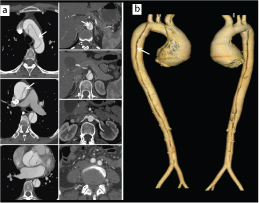
Axial contrast enhanced (a) axial, (b) curved coronal and sagittal, (c) VR images show atheromatous aorta (arrow) with significant luminal stenosis due to a thrombus (triangle) of the infrarenal segment. Also, note a large collateral between the supra and infrarenal segments (open arrow).
Group I: Table illustrating clinical associations, disease location and special imaging features of Group I of aortic disease observed in our study.
| Atherosclerosis (Group I) |
|---|
| Observations | No | % | Additional Features |
| Total cases | 59 | 65.50% | Atherosclerosis 23 (18:5) |
| Age between 61-70yr | 8 | 34.70% | Luminal stenosis(>50%) 17 (28.8%) |
| Male | 52 | 88.10% |
| Female | 7 | 11.90% |
| Risk factors |
| Hypertension | 14 | 60.80% | |
| Diabetic mellitus | 19 | 82.60% |
| Smoking | 15 | 65.20% |
| Dyslipedemia | 13 | 56.40% |
| Segmental involvement | Penetrating ulcers | 9 (15.2%) |
| Suprarenal | 52 | 88.10% | Suprarenal | 3 (33.3%) |
| Renal | 55 | 93.20% | Renal | 5 (55.5%) |
| Infrarenal | 57 | 96.60% | Infrarenal | 7 (77.7%) |
Contrast enhanced coronal & sagittal images (a,b) and VR images(c) show extensive atheromatous changes in the abdominal aorta. There is fusiform aneurysm of the infrarenal abdominal aorta (open arrows) with concentric mural thrombus. (arrows) Also note ectatic bilateral common iliac arteries.
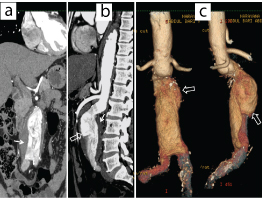
Axial contrast enhanced images (a,b), curved coronal, sagittal images(c,d) and VR images (e) show saccular aneurysm of the suprarenal abdominal aorta (arrows) and fusiform aneurysm at the level of renal arteries with a focal dissection. Also note fusiform aneurysm of the infrarenal aorta (open arrows) and extensive atheromatous changes in the abdominal aorta extending into bilateral common iliac arteries.
Group II and III a: Table illustrating clinical associations, disease location and special imaging features of Group II of aortic disease.
| Aneurysm (Group II and III) |
|---|
| Observations | No | % | Associated Features |
|---|
| Total cases | 41 | 45.50% | Type of aneurysm |
| Age between 61-70yr | 14 | 34.20% | Fusiform | 37 (90.2%) |
| Male | 39 | 95.10% | Saccular | 4 (9.8%) |
| Female | 2 | 4.90% | |
| Risk factors | Other complications |
| Hypertension | 29 | 70.20% | Mural thrombus | 24 (58.5%) |
| Diabetic mellitus | 28 | 68.20% | Wall calcification | 27 (65.8%) |
| Smoking | 26 | 63.40% | |
| Dyslipedemia | 15 | 36.50% | Dissection | 7 (17.1%) |
| Segmental involvement | | | Contained leak | 2 (4.8%) |
| Suprarenal | 18 | 43.90% | Impending rupture | 2 (4.8%) |
| Renal | 24 | 58.30% | Rupture | 1 (2.4%) |
| Infrarenal | 31 | 75.60% | |
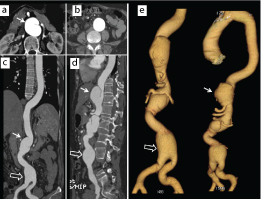
Axial post contrast images at multiple levels (a) and VR images of thoracic and abdominal aorta (b) up to common iliac arteries showing acute type of aortic dissection. Intimal flaps are demonstrated with arrows.
Multiple contrast enhanced axial images (a), sagittal (b) and coronal curved reconstruction(c) of thoracic and abdominal aorta up to common iliac arteries showing type an aortic dissection (open arrow). Note partial thrombosis of the false lumen (arrow). Celiac artery and right renal arteries are arising from the true lumen. (triangle).
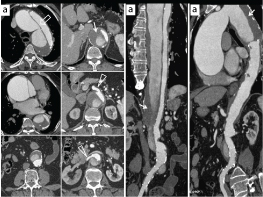
VR images of thoracic and abdominal aorta illustrate extent of dissection in different color. There is aneurysm of ascending aorta.

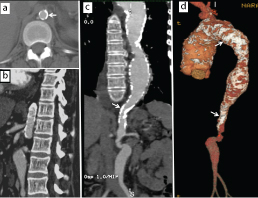
Aorto-arteritis was seen in 7/90 (7.7%). Imaging features consisted of wall thickening and wall calcifications, seen in all patients (100%) [Table/Fig-11]. Significant luminal stenosis was seen in 6/7 cases (85.7%) and luminal dilatation in 4 cases (57.1%). In association with aorto-arteritis, celiac trunk occlusion was seen in 4 cases (57.1%). SMA and RCIA (42.8%) and RRA, LRA and LCIA occlusions in (28.5%) [Table/Fig-12].
Axial post contrast image (a), sagittal (b), coronal curved reconstruction(c) and VR reformations (d) show irregular narrowing and aneurysmal segments involving the entire aorta. There is extensive wall calcification (arrows) and thickening in a case of aorto-arteritis.
Group IV: Table illustrating clinical associations, disease location and special imaging features of Group III of aortic disease.
| Aorto-arteritis (Group IV) |
|---|
| Observations | No | % | Associated features | |
|---|
| Total cases | 7 | 7.70% | Wall thickening | 7 (100%) |
| Mean age | | 57 yrs | Wall calcification | 7 (100%) |
| Male | 2 | 24.60% | Luminal stenosis | 6 (85.7%) |
| Female | 5 | 71.40% | Luminal dilatation | 4 (57.1%) |
| Risk factors |
| Hypertension | 2 | 28.50% | Occlusion of major vessels | |
| Diabetic mellitus | 2 | 28.50% | Celiac A | 4 (57.1%) |
| Smoking | 1 | 14.20% | Superior mesenteric A | 3 (42.8%) |
| Dyslipedemia | 1 | 14.20% | Inferior mesenteric A | 1 (14.2%) |
| Segmental involvement | Right common Iliac A | 3 (42.8%) |
| Suprarenal | | Variable | Left common Iliac | 2 (28.5%) |
| Renal | | | Right Renal A | 2 (28.5%) |
| Infrarenal | | | Left Renal A | 2(28.5%) |
Positive angiography confirmation was available in 12/59 patients with atherosclerosis, mostly examination were done along with coronary angiography. Angiography confirmation was also available in 7/41 patients with aneurysm/dissection and 2/7 patients with complicated aorto-arteritis. Surgical/Interventional correlation was present in 13/41 patients with aneurysm/dissection, 4/59 with atherosclerosis with complication and 2/7 patients with aorto-arteritis with vessel occlusion.
Discussion
Multidetector CT is an accurate, comprehensive modality for vascular imaging, suited for evaluation of medium and large vessels [6]. Abdominal aortic diseases like atherosclerosis, aneurysm and dissection occur frequently in adult, often elderly age group [10,20–23]. On the other hand, aorto-arteritis has a higher prevalence in younger age groups [7]. Our patients with atherosclerosis, in conformity with the reported incidence in other studies, showed male predominance and higher incidence (65.5%) in age group between 61-70 years [22,24]. Relatively younger patient with slightly higher female incidence were noted in aorto- arteritis group (1:3). Similar observations were noted in a study by RG Salkar et al., [7]. We also noted a slightly higher incidence of aneurysms (45%) in comparison with dissection (32.2%) in conformity with literature [25]. Reported incidence of infrarenal aneurysm was 88% in a series [26]. We noted infrarenal aneurysm in 75.6% of cases. Most (85%) of the patients with aneurysm were male. We also found association of smoking, diabetes and hypertension with abdominal aortic diseases, as observed in other larger studies [18,22,24].
Aortic aneurysms are known to be associated with complications like acute aortic dissections, aneurismal rupture and branch vessel occlusions [10,26–29]. These patients may present with an acute condition necessitating prompt diagnosis and management. We found acute aortic dissection as a most common cause of admission to emergency services, similar to an earlier report [30]. Types of dissection in association with aneurysm vary [20,31]. Carmen Sebastià et al., reported 60% Stanford type A and 40% were type B dissections in association with aneurysm [20]. Classical imaging signs like beak sign, cobwebs were present in both acute and chronic dissections. Intraluminal thrombus was more common in the false lumen (more frequent in chronic dissection, 86% vs. 46%) compared with the true lumen (4-6%). We found type A dissection in 69% and type B dissection in 31% cases. Beak sign was seen in all patients (100%) and cobwebs were seen only in 13.7% cases. Thrombosis of false lumen was noted in 31% and relatively higher (20.6%) number of patients showed thrombosis of the true lumen. Diagnostic accuracy with helical CT ranges from 88% to 100% in detecting the dissections and classifying the true and false lumen [31,32]. Comparison of MDCT observations with catheter angiography data and surgical correlation, in available cases, showed 100% correlation.
CT imaging has more important role to play in imaging aorto-arteritis by virtue of providing information regarding vessel wall and perivascular structures [32,33]. Yamada et al., showed that sensitivity and specificity of the helical CT was 95% and 100% in conformity with our own observations [34]. CT and MR imaging are equally effective in postoperative aorta [35]. In a study on post-operative endovascular stent-graft patients with both conventional and CT angiography, authors found that sensitivity and specificity of conventional and CT angiography in detecting the post stent-graft complications were 63% and 77% for conventional angiography and 92% and 90% for CT angiography, respectively [35]. CT angiography is the preferred method for establishing the presence of peri-graft leakage following treatment of aorto-iliac aneurysms with stent-grafts. We had a single patient with the peri-graft leak. In view of the technique without involving ionizing radiation, MR imaging with the bright blood technique has important role play in luminal assessment of postoperative aorta.
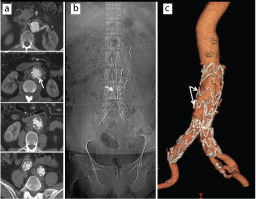
In patients with intravascular stent/graft, MDCT angiography observations can be utilized as a surrogate parameter in assessing the surgical outcome, lumen of stents and complications related to stents [Table/Fig-13]. Endoleaks is the most common complication of associated with endovascular stenting of aneurysm, Type 1 endoleaks occurring most frequently. Thin section imaging with 1 mm slice thickness provides better detection rates of endovascular leak [36,37]. Volumetric data acquisition with thin partitioning (0.625 mm) as performed in our study provides greater advantage for detection of endoleaks. In conclusion, CT angiogram proves to be best choice in preoperative assessment of the abdominal aortic disease and related complications. Measurements obtained by CT angiogram guide the vascular interventionists to decide on type and size of endovascular stents to be used.
Multiple axial post contrast images (a), scan gram of abdomen (b) and VR image(c) illustrate a stent in the infrarenal abdominal aorta (arrows) extending into bilateral common iliac arteries in an aneurysm patient. Stent is patent with no evidence of leak.
We have used standardized CT and contrast delivery techniques with automated bolus triggering technique in all patients. Varying techniques are described in the literature, some examinations intended to demonstrate contrast enhancement of the aortic wall. We had satisfactory results for evaluating vessel wall enhancement with the bolus technique. Careful matching of duration of the contrast injection and scan acquisition time was needed with the earlier generation scanners [12,13]. Generally, contrast volume of 120-170 ml is used, calculated on the patient weight. (Max 2ml/kg) [18]. Rubin et al., demonstrated that substantial reductions in contrast medium dose were possible with multi–detector row CT compared with single–detector row CT. In their study of the thoraco-abdominal aorta, the dose was determined by calculating a bolus duration that was equivalent to the scanning duration at an injection rate of 4 mL/sec. For example, for a scanning duration of 31 seconds, the total contrast medium dose administered was 124 mL [18,19].
Evaluation with the catheter angiography can additionally demonstrate subtle signs of vessel irregularity or occlusion. Slight advantage of DSA is found in some studies improving sensitivity as well as specificity [38]. State of the art MDCT evaluation is the nearly capable of the demonstrating most of medium-size vessel occlusion, along with the global assessment of the lesion as confirmed in our study.
Limitation
There are few limitations in our study. Our study was conducted at a private, tertiary hospital; hence there can be referral bias, leading to inaccurate inference on the incidence/prevalence of disease. Other limitation of the study is that we had a small number of patients with surgical/interventional confirmation and follow-up. Multiple factors were responsible for drawback that included financial considerations and limited management options.
Conclusion
Predominant abdominal aortic disease in our study was atherosclerosis with or without an abdominal aortic aneurysm. The aorto-arteritis contributed to significant number of patients in relatively younger age range. Overall incidence and pattern of disease confirm to incidence, described in literature. MDCT angiography with automated pressure injection of contrast provides optimal method for non-invasive evaluation of diseases of the abdominal aorta and its major branches. MDCT accurately delineated and differentiated various pathologies of the abdominal aorta. MDCT is the investigation of choice in the abdominal aortic emergencies and an integral tool in pre-operative evaluation of the abdominal aorta. MDCT angiography is very useful in post-operative evaluation of the intravascular repair stent/graft and its complications.
(Adapted from the ESC 2014 guidelines on aortic disease [8]).
[1]. Grainger and Allison’s textbook of radiology. Ed: Andy Adam, Adrian K. Dixon, Jonathan H Gillard, Cornelia Schaefer-Prokop, Ronald G. Grainger, and David J. Allison. The Aorta including interventions 2001 Volume 15th edition:547-70.Chapter 27 [Google Scholar]
[2]. Ho LM, Nelson RC, Thomas J, Gimenez EI, DeLong DM, Abdominal aortic aneurysms at multi–detector row helical CT: Optimization with interactive determination of scanning delay and contrast medium doseRadiology 2004 232:854-59. [Google Scholar]
[3]. Cademartiri F, Raaijmakers RH, Kuiper JW, van Dijk LC, Pattynama PM, Krestin GP, Multi–detector row CT angiography in patients with abdominal anginaRadiographics 2004 24:969-84. [Google Scholar]
[4]. Cigarroa JE, Isselbacher EM, Desanctis RW, Eagle KA, Diagnostic imaging in the evaluation of suspected aortic dissection — Old standards and new directionsNEJM 1993 328:35-43. [Google Scholar]
[5]. Varma PK, Latha M, Purushotham SN, Neelakandhan KS, Abdominal aortic occlusion due to aorto arteritisEUR J Cardiothorac Surg 2003 24:451 [Google Scholar]
[6]. Hayashi H, Kumazaki T, Multidetector-row CT evaluation of aortic diseaseRadiation Medicine 2005 23:1-9. [Google Scholar]
[7]. Salkar RG, Parate R, Taori KB, Parate TR, Salkar HR, Mahajan S, Aortoarteritis: A study of 33 central Indian patientsIndian J Radiol Imaging 2003 13:61-6. [Google Scholar]
[8]. 2014 Aortic Diseases - European Society of Cardiology. https://www.escardio.org/static_file/Escardio/.../ADEM_Aortic-Diseases_2014.pdf [Google Scholar]
[9]. Tarkin JM, Dweck MR, Evans NR, Takx RA, Brown AJ, Tawakol A, Imaging AtherosclerosisCirc Res 2016 118:750-69. [Google Scholar]
[10]. Qanadli SD, Mesurolle B, Coggia M, Barré O, Fukui S, Goeau-Brissonnière OA, Abdominal aortic aneurysm pretherapy assessment with dual-slice helical CT angiographyAJR 2000 174:181-87. [Google Scholar]
[11]. Armerding MD, Rubin GD, Beaulieu CF, Slonim SM, Olcott EW, Samuels SL, Aortic aneurysmal disease: Assessment of stentgraft treatment-CT versus conventional angiographyRadiology 2000 215:138-46. [Google Scholar]
[12]. Martin ML, Tay KH, Flak B, Fry PD, Doyle DL, Taylor DC, Multidetector CT angiography of the aortoiliac system and lower extremities: A prospective comparison with digital subtraction angiographyAJR 2003 180:1085-91. [Google Scholar]
[13]. Platt JF, Reige KA, Ellis JH, Aortic enhancement during abdominal CT angiography: correlation with test injections, flow rates, and patient demographicsAJR Am J Roentgenol 1999 172(1):53-56. [Google Scholar]
[14]. Frauenfelder T, Wildermuth S, Marincek B, Boehm T, Nontraumatic emergent abdominal vascular conditions: Advantages of multi–detector row CT and three- dimensional imagingRadiographics 2004 24:481-96. [Google Scholar]
[15]. Kohl G, The evolution and state-of-the-art principles of multislice computed tomographyProc Am Thorac Soc 2005 2(6):470-76.:499-500. [Google Scholar]
[16]. Boskamp T, Rinck D, Link F, Kümmerlen B, Stamm G, Mildenberger P, New vessel analysis tool for morphometric quantification and visualization of vessels in CT and MR imaging data setsRadiographics 2004 24:287-97. [Google Scholar]
[17]. Rubin GD, Walker PJ, Dake MD, Napel S, Jeffrey RB, McDonnell CH, Three-dimensional spiral computed tomographic angiography: an alternative imaging modality for the abdominal aorta and its branchesJ Vasc Surg 1993 18:656-65. [Google Scholar]
[18]. Rubin GD, Shiau MC, Leung AN, Kee ST, Logan LJ, Sofilos MC, Aorta and iliac arteries: single versus multiple detector-row helical CT angiographyRadiology 2000 215:670-76. [Google Scholar]
[19]. Fishman EK, Ney DR, Heath DG, Corl FM, Horton KM, Johnson PT, Volume rendering versus maximum intensity projection in CT angiography: What works best, when, and whyRadiographics 2006 26:905-22. [Google Scholar]
[20]. Sebastià C, Pallisa E, Quiroga S, Alvarez-Castells A, Dominguez R, Evangelista A, Aortic dissection: Diagnosis and follow up with helical CTRadiographics 1999 19:45-60. [Google Scholar]
[21]. Batra P, Bigoni B, Manning J, Aberle DR, Brown K, Hart E, Pitfalls in the diagnosis of thoracic aortic dissection at CT angiographyRadiographics 2000 20:309-20. [Google Scholar]
[22]. Borioni R, Garofalo M, De Paulis R, Nardi P, Scaffa R, Chiariello L, Abdominal aorticdissections anatomic and clinical features and therapeutic optionTex Heart Inst J 2005 32(1):70-73. [Google Scholar]
[23]. Kapoor V, Ferris JV, Fuhrman CR, Intimomedial rupture: A new CT finding to distinguish true from false lumen in aortic dissectionAJR 2004 183:109-12. [Google Scholar]
[24]. Hayter RG, Rhea JT, Small A, Tafazoli FS, Novelline RA, Suspected aortic dissection and other aortic disorders: multi-detector row CT in 373 cases in the emergency settingRadiology 2006 238:841-52. [Google Scholar]
[25]. Costello P, Gaa J, Spiral CT angiography of abdominal aortic aneurysmsRadiographics 1995 15:395-406. [Google Scholar]
[26]. Rakita D, Newatia A, Hines JJ, Siegel DN, Friedman B, Spectrum of CT findings inrupture and impending rupture of abdominal aortic aneurysmsRadiographics 2007 27:497-507. [Google Scholar]
[27]. Schwartz SA, Taljanovic MS, Smyth S, O’Brien MJ, Rogers LF, CT findings of rupture, impending rupture, and contained rupture of abdominal aortic aneurysmsAJR Am J Roentgenol 2007 188(1):W57-62. [Google Scholar]
[28]. Sever A, Rheinboldt M, Unstable abdominal aortic aneurysms: a review of MDCT imaging featuresEmerg Radiol 2016 23(2):187-96. [Google Scholar]
[29]. Wadgaonkar AD, Black JH, Weihe EK, Zimmerman SL, Fishman EK, Johnson PT, Abdominal aortic aneurysms revisited: MDCT with multiplanar reconstructions for identifying indicators of instability in the pre- and postoperative patientRadiographics 2015 35(1):254-68. [Google Scholar]
[30]. Olin JW, Fuster V, Acute aortic dissection: The need for rapid, accurate, and readily available diagnostic strategiesArterioscler Thromb Vasc Biol American heart association 2003 23:1721-23. [Google Scholar]
[31]. LePage MA, Quint LE, Sonnad SS, Deeb GM, Williams DM, Aortic dissection CT features that distinguish true lumen from false lumenAJR 2001 177:207-11. [Google Scholar]
[32]. Hamada S, Takamiya M, Kimura K, Imakita S, Nakajima N, Naito H, Type A aortic dissection: evaluation with ultrafast CTRadiology 1992 183:155-58. [Google Scholar]
[33]. Yoshida S, Akiba H, Tamakawa M, Yama N, Hareyama M, Morishita K, Thoracic involvement of type A aortic dissection and intramural hematoma: Diagnostic Accuracy—Comparison of emergency helical CT and surgical findings. RSNARadiology 2003 228:430-35. [Google Scholar]
[34]. Yamada I, Nakagawa T, Himeno Y, Numano F, Shibuya H, Takayasu arteritis: Evaluation of the thoracic aorta with CT angiographyRadiology 1998 209(1):103-09. [Google Scholar]
[35]. Liu Q, Lu JP, Wang F, Wang L, Tian JM, Three-dimensional contrast-enhanced MR angiography of aortic dissection: A pictorial essayRadiographics 2007 27:1311-21. [Google Scholar]
[36]. Nikolaou K, Knez A, Rist C, Wintersperger BJ, Leber A, Johnson T, Accuracy of 64-MDCT in the diagnosis of ischemic heart diseaseAJR 2006 187:111-17. [Google Scholar]
[37]. Iezzi R, Cotroneo AR, Filippone A, Di Fabio F, Santoro M, Storto ML, MDCT angiography in abdominal aortic aneurysm treated with endovascular repair: Diagnostic impact of slice thickness on detection of endoleaksAJR 2007 189:1414-20. [Google Scholar]
[38]. Subramanyan R, Joy J, Balakrishnan KG, Natural history of aortoarteritis (Takayasu’s disease)Circulation 1989 80(3):429-37. [Google Scholar]