A Case of Surgical Site Infection Caused by Mycobacterium fortuitum, following Herniorrhaphy
NS Madhusudhan1, A Malini2, Mima Maychet B Sangma3
1 Assistant Professor, Department of Microbiology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
2 Associate Professor, Department of Microbiology, Indira Gandhi Medical College and Research Institute, Puducherry, India.
3 Associate Professor, Department of General Surgery, Indira Gandhi Medical College and Research Institute, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. NS Madhusudhan, Assistant Professor, Department of Microbiology, Indira Gandhi Medical College and Research Institute, Puducherry - 605001, India.
E-mail: drnsmadhu98@gmail.com
Rapidly Growing Mycobacteria (RGM) are opportunistic pathogens found in the environment. Mycobacterium fortuitum, M. chelonae and M.abscessus are the important human pathogens of this group. They cause wound infections, disseminated cutaneous disease, pulmonary infection in patients with cystic fibrosis or bronchiectasis, bone and joint infections and keratitis. Infections due to these Non-Tuberculous Mycobacteria (NTM) are increasingly reported. Post laparoscopic wound infections, mesh site infections and other surgical site infections due to M. fortuitum and M. chelonae have been reported. Usually wound infections due to atypical mycobacteria have delayed onset and do not respond to conventional antibiotics. Identification of RGM can be done by a set of cumbersome biochemical tests, High Performance Liquid Chromatography (HPLC), molecular methods using DNA probes or by Polymerase Chain Reaction (PCR). We here report a case of post-herniorrhaphy wound infection due to M. fortuitum which was identified by molecular method (HAIN mycobacterial species system). This case report underscores the importance of examining Ziehl-Neelsen (ZN) stain of all exudates with sterile culture on day one for non fastidious bacteria. Timely identification can lead to prompt therapy of patients preventing further complications.
Atypical mycobacterium, Ciprofloxacin, Ziehl-Neelsen
Case Report
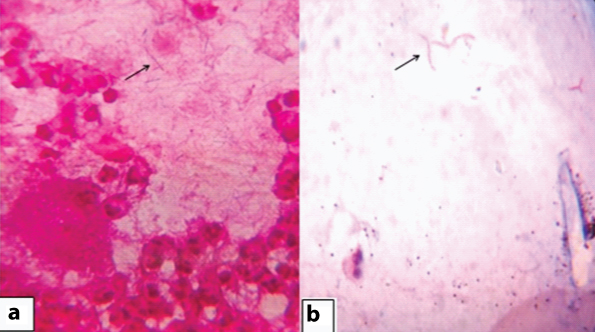
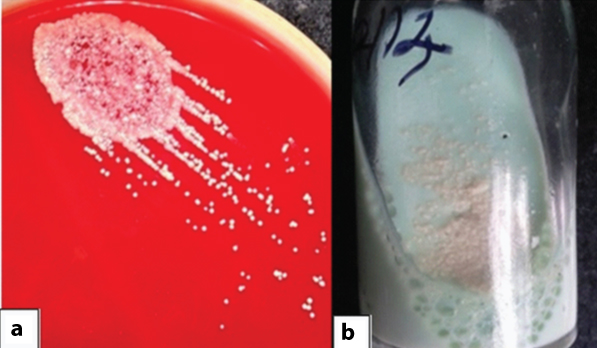
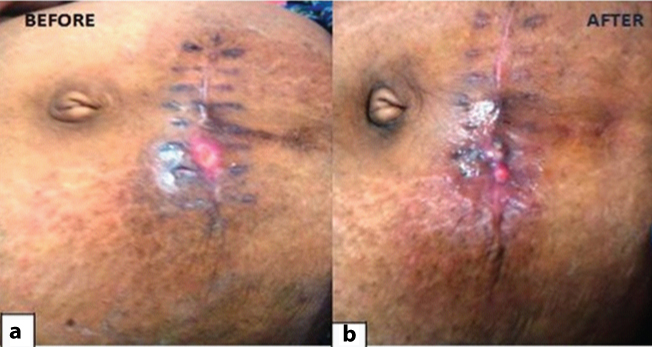
A 28-year-old non diabetic lady with no identifiable immunosuppressive condition presented with low grade fever and discharge from a herniorrhaphy wound since five days to the surgical outpatient department. She had undergone hernioplasty for infraumbilical hernia one month earlier. On examination, a swelling about 2cm x1cm in size, fluctuant, and tender with defined borders was noted along the suture line from which purulent discharge was aspirated. The gram stain from the aspirate showed gram positive bacilli with numerous pus cells [Table/Fig-1a]. ZN stain revealed presence of faintly acid fast, elongated, branching bacilli [Table/Fig-1b]. Culture on Blood agar and Lowenstein Jensen (LJ) medium grew non-chromogenic buff colored colonies on fifth day [Table/Fig-2]. Suspecting the bacterium to be atypical mycobacterium, it was sent to Kasturba Medical College, Manipal for further identification. The patient was treated with oral cotrimoxazole and intravenous ceftriaxone for 5 days. The symptoms improved and she was discharged with the advice to continue cotrimoxazole for four weeks and follow up after a week. The bacterium was identified as Mycobacterium fortuitum by HAIN MYCOBACTERIAL speciation system after 15 days. Three months later, patient returned with foul smelling mucopurulent minimal discharge since two days from the same site. Aerobic bacterial culture of the swab taken from discharge yielded no growth. The patient was admitted and treated with intravenous amikacin (intramuscular 15 mg/kg body weight) and ciprofloxacin (400mg oral OD) for 15 days, following which the ulcer healed. She was then discharged with the advice to continue ciprofloxacin for two more weeks. She was followed up for 4 weeks, and the wound healed completely [Table/Fig-3], and she did not return with similar complaints.
Direct gram stain showing gram variable bacilli and ZN stain demonstrating acid fast bacilli with rudimentary branches.
Blood agar plate and LJ medium showing smooth white colonies.
Healthy healing wound from surgical incision site following amikacin and ciprofloxacin therapy.
Discussion
Being ubiquitous in nature, NTM is found in both clean and sewage water. It is transmitted by aerosol, soil, dust, water, ingestion or by skin inoculation, whereas it’s person to person spread is rare [1].
This was a sporadic case we encountered, a post surgical infection following herniorrhaphy with mesh placement. Lahiri et al., have reported a series of five cases of post surgical infections due to M. fortuitum, in patients who underwent laparoscopic tubectomies or herniorrhaphy [2].
Typically surgical site infections due to atypical mycobacteria have long incubation periods, as evident in our case where the patient presented with discharge one month after the surgery [3].
Initially, the post-operative wound seemed to have healed, but later turned erythematous and gradually developed into a discharging wound. There was no fever, pain or any other systemic symptoms. A chronic non-healing wound may therefore present a confusing picture and in such cases mycobacterial infection should always be ruled out. Atypical mycobacteria were isolated from 80% of the cases of delayed post-operative wound healing [3].
Hybridization with DNA probes (Accuprobe system) is the most common molecular method used for identification of NTM [4]. GenoType kits (HAIN system) combine the principle of amplification and hybridization technology [4]. The advantage of genotype kit is the ability to detect mixed infections and also helps in the rapid identification within 6 hours. The major drawbacks are the high cost and the need to have a fully-grown culture to obtain reliable results. INNO-LiPA Mycobacteria v2 assay, a molecular method based on reverse hybridization principle permits simultaneous identification of 16 species of mycobacteria, including RGM [5].
Cutaneous infections with NTM require a combination of clarithromycin and amikacin or fluoroquinolones with amikacin for long term [1]. A study from North East India showed that seven out of 25 cases with delayed wound infections due to NTM were cured with clarithromycin and amikacin for 2-3 months along with vigorous surgical debridement [3]. A case of chronic discharging sinus due to M. fortuitum was successfully treated with ofloxacin and amikacin in PGI, Chandigarh [6]. In our case, the patient was treated with ciprofloxacin and amikacin for 8 weeks and was followed up for one month with no recurrence.
Conclusion
This case report underscores the importance of routinely examining ZN stain on all exudates with sterile culture, keeping a vigilant eye on atypical mycobacteria that can cause smoldering post-operative infection. NTM should be kept in mind in wounds showing delayed healing and not responding to conventional antibiotics. Early aetiological diagnosis helps in appropriate therapy and prevention of complications in such cases.
[1]. Nag VL, Rahman W, Maurya AK, Kumar M, Kumar Dhole TN, Non healing post surgical wound due to NTM (Mycobacterium fortuitum) in immunocompetent patient treated by conservatively in tertiary care centreJ Biomed Sci and Res 2010 2:227-30. [Google Scholar]
[2]. Lahiri KK, Jena J, Pannicker KK, Mycobacterium fortuitum Infections in surgical woundsMJAFI 2009 65:91-92. [Google Scholar]
[3]. Kalita JB, Rahman H, Baruah KC, Delayed postoperative wound infections due to non-tuberculous MycobacteriumIndian J Med Res 2005 122:535-39. [Google Scholar]
[4]. Couto I, Machado D, Viveiros M, Rodrigues L, Amaral L, Identification of nontuberculous Mycobacteria in clinical samples using molecular methods: a 3-year studyClin Microbiol Infect 2010 16:1161-64. [Google Scholar]
[5]. García-Agudo L, Jesús I, Rodríguez-Iglesias M, García-Martos P, Evaluation of Inno-lipa Mycobacteria v2 assay for identification of rapidly growing MycobacteriaBrazilian Journal of Microbiology 2011 42:1220-26. [Google Scholar]
[6]. Sethi S, Arora S, Gupta V, Kumar S, Cutaneous Mycobacterium fortuitum Infection: successfully treated with amikacin and ofloxacin combinationIndian J Dermatol 2014 59:383-84. [Google Scholar]