Introduction
Peroral extrusion of peritoneal part of Ventriculoperitoneal Shunt (VPS) catheter is an extremely rare complication following VPS implantation.
Aim
To review the options available for the management of peroral extrusion of VPS catheter.
Materials and Methods
PubMed, Medline, PMC (PubMed Central), Embase, Google scholar databases search was performed to retrieve the published/available data relating to the peroral extrusion of VPS catheter. The keywords employed were “peroral extrusion of ventriculoperitoneal shunt catheter”, “transoral extrusion of ventriculoperitoneal shunt catheter”, and “oral extrusion of ventriculoperitoneal shunt catheter”. The maiden description of peroral extrusion of VPS catheter was reported in the year 1987, and the data relating to peroral extrusion of VPS were retrieved from that period to June 30, 2016, and those were available in English literature.
Results
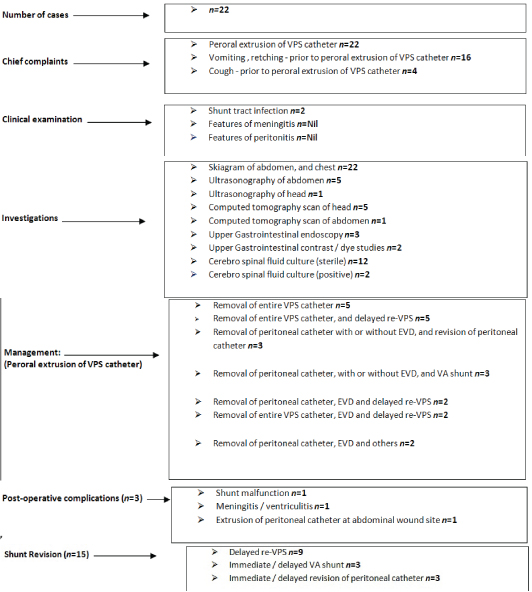
Twenty-two published manuscripts (n) were available on the topic relating to peroral extrusion of VPS catheter. All were cases and were included for the review. This review included n=10; 45.45% male and n=12; 54.54% female. All of them were reported in children below 12-year of the age, except two case reports in adult that occurred at the age of 27-year and 47-year, respectively. Overall, the mean age at the time of peroral extrusion of VPS catheter was 6.94 ± 10.87 years. The interval from VPS insertion or last shunt revision to the occurrence of peroral extrusion of VPS catheter ranged from 10-days to 10-year, with a mean of 20.31 ± 28.37 months. More than two-third (n=15; 68.18%) of the case occurred within one-year of VPS insertion/last shunt revision. Clinical diagnosis was obvious in all the cases due to peroral extrusion of VPS catheter. The site of perforation by the VPS catheter was stomach in 15, jejunum in 1, diaphragm/trachea in 1, while the site of bowel perforation was not mentioned in 5 cases. Surgical procedures opted by authors in order of frequency were: (a) removal of entire VPS catheter n=5; (b) removal of entire VPS catheter, and delayed re-VPS n=5; (c) removal of peritoneal catheter with or without External Ventricular Drainage (EVD), and revision of peritoneal catheter n=3; (d) removal of peritoneal catheter, with or without EVD, and VA shunt n=3; (e) removal of peritoneal catheter, EVD and delayed re-VPS n=2; (f) removal of entire VPS catheter, EVD and delayed re-VPS n=2; (g) removal of peritoneal catheter, EVD and others n=2. Two deaths are also reported during the management of peroral extrusion of VPS catheter.
Conclusion
Peroral extrusion of peritoneal part of VPS catheter is an extremely rare complication following VPS insertion, and most frequently observed in children, although also reported in adults. In more than two-third of the cases it occurred within one-year of the VPS placement or last shunts revision, so a close follow-up is a must during this period following VPS placement. Management of such a case depends upon many factors such as presence or absence of shunt tract infection, peritonitis, meningitis, and cerebro spinal fluid infection.
Children, Hydrocephalus, Infant, Oral extrusion, Ventriculoperitoneal shunt complication
Introduction
Ventriculo-Peritoneal Shunt (VPS) implantation is routinely employed for shunting Cerebrospinal Fluid (CSF) in management of hydrocephalus across all age groups [1–6]. Complications following VPS implantation are known to occur in approximately one-fifth to four-fifth of all implanted cases [2,4,7,8]. Commonly encountered complications include shunt malfunction or obstruction, over drainage, infections and abdominal complications [2,4,7,8]. Most of these necessitate multiple shunt revisions [2,4,7,8]. Abdominal complications including, but not limited to bowel obstruction, volvulus, ileus, perforation, peritoneal pseudocysts are well documented [7]. Colon perforation with extrusion of the VPS catheter via rectum is known to occur in 0.1 to 2.5% of cases [3,7,9]. However, peroral extrusion of VPS catheter is rare with limited isolated reports [10–31]. With paucity of literature highlighting this seldom encountered complication, i report my findings from a systematic review of the literature to highlight the demographics, clinical characteristics and managements.
Materials and Methods
PubMed, Medline, PMC, Embase, Google scholar database search was performed to retrieve the published/available data relating to the peroral extrusion of VPS catheter. The key-words employed during online search were “peroral extrusion of ventriculoperitoneal shunt catheter”, “transoral extrusion of ventriculoperitoneal shunt catheter”, and “oral extrusion of ventriculoperitoneal shunt catheter”. The maiden description of peroral extrusion of VPS catheter was reported by Griffith et al., in 1987 [10], and the data relating to peroral extrusion of VPS catheter were retrieved from that period to June 30, 2016, and those were available in English literature. One case report relating to peroral extrusion of VPS catheter in which the title was in English language but detail was published in Spanish, was also included for review. The detail for this manuscript was obtained through personal request to the corresponding author through ResearchGate. Cases of peroral extrusion of VPS catheter following VPS placement published/available in language other than English, was not included in this review. This review included only the cases those at had bowel perforation and presented as peroral extrusion of VPS catheter. Cases those had gastric perforation/bowel perforation, but not presented as peroral extrusion of VPS catheter were excluded for review. Screening of the articles was done by reviewing full texts of the manuscripts relating to peroral extrusion of VPS catheter. The types of manuscript included in this review were: (a) case reports n=15 (68.15%); (b) letter to editor n=3 (13.63%); (c) original/clinical article also included one case of peroral extrusion of VPS catheter n=1 (4.54%); (d) case series also included one case of peroral extrusion of VPS catheter n=1 (4.54%); (e) case report as surgical technique n=1 (4.54%); and (f) images n=1 (4.54%). All the manuscripts included for review relating to peroral extrusion of VPS catheter were published manuscripts, and none were conference proceedings.
Results
There were 22 isolated reports/published manuscripts available on the topic relating to the peroral extrusion of VPS catheter. The maiden depiction of peroral extrusion of VPS catheter was reported by Griffith et al., in 1987 [10]. The demographics and clinical characteristics of all reported cases are tabulated in [Table/Fig-1] [10–31]. Overall, the mean age at the time of peroral extrusion of VPS catheter was 6.94±10.87 years. The incidence was more in female (n=12/22; 54.54%) with female to male ratio of 1.2:1. An age related trend for peroral extrusion of VPS catheter was noted, commonly occurring in children 12-year-old or younger (n=20/22; 90.9%) with exception of two reports in adults at ages 27 and 47 years respectively. The age at the time of peroral extrusion of VPS catheter were; 0-2 year n=12 (54.54%), 3-5 year n=2 (9.09%), 6-12 year n=6 (27.27%), and more than 12 year n=2 (9.09%). The interval from VPS insertion or last shunt revision to the occurrence of peroral extrusion of VPS catheter ranged from 10-days to 10-year, with a mean of 20.31 ± 28.37 months. More than two-third n=15 (68.18%) of the cases occurred within one-year and of these n=9 (40.9%) occurred within 6-months, n=5 (22.72%) occurred after one year to 5-year, and only 2 cases (9.09%) reported after 5-year of VPS insertion/last shunt revision. Clinical diagnosis was obvious in all the cases due to peroral extrusion of VPS catheter. The site of bowel perforation by the peritoneal part of VPS catheter is given in [Table/Fig-2].
Demographics of case reports published relating to peroral extrusion of VPS catheter.
| Authors(Year Published) | Primary Diag-nosis | Age / SexVPS Surg | Age - Peroral Extrusion | IntervalVPS Surg /VPS Revision | His-toryGI Surg | His-tory VPS Revision | ShuntTract Infection | (Pre-op)MeningitisPeritonitis | CSF Infection | Site of Perforation | Management of Peroral Extrusion of VPS Catheter | (Post-op)Complication | Follow - up | Remark |
|---|
| Griffith JA, et al.,(1987) | Tuberculous meningitis with Hydrocephalus | 9.6 yr / F | 9.9 yr | 3 m | Yes | Yes | No | NoNo | No | Stomach | (I) Removal of part of peritoneal catheter + EVD,(II) Delayed VA shunt | Shunt malfu-nction | 1m | Death |
| Danismend N, et al.,(1988) | Congenital Hydrocephalus | 8 m / F | 18 m | 10 m | No | Yes | No | NoNo | No | Stomach | (I) Exp lap, removal of peritoneal catheter and VA Shunt | Nil | - | Well |
| Fermin S, et al.,(1996) | Congenital Hydrocephalus | 8 m / F | 14 m | 6 m | No | No | No | NoNo | No | Diaphragm + trachea | (I) Exp lap, removal of part of peritoneal catheter + re-insertion in to peritoneal cavity | Nil | - | Well |
| Park CK, et al.,(2000) | Post-haemorrhagicHydrocephalus | 1 yr / F | 5 yr | 4 yr | No | No | Yes | NoNo | No | Stomach | (I) EVD + UGI endoscopic removal of part of peritoneal catheter +(II) Delayed Re-VPS | Nil | 12 m | Well |
| Jiménez Moya A,et al.,(2001) | Medulloblastoma | 9.11 yr/ F | 11.2 yr | 2 m | Yes | Yes | No | NoNo | No | Stomach | (I) Removal of entire VPS catheter, and(II) Delayed re-VPS | Nil | - | Well |
| Kothari PR, et al.,(2006) | Congenital Hydrocephalus | 1 m / M | 18 m | 17 m | No | No | No | NoNo | Yes | Not mentioned | (I) Removal of entire VPS catheter,(II) Delayed re-VPS | Nil | - | Well |
| Odebode TO.(2007) | Congenital Hydrocephalus | 9 m / F | 15 m | 6 m | No | No | Yes | NoNo | No | Jejunum | (I) Exp lap, removal of entire VPS catheter,(II) Delayed re-VPS | Nil | - | Well |
| Berhouma M, et al., (2008) | Myelomenigocele and Congenital Hydrocephalus | 9 m / M | 2 yr | 15 m | No | No | No | NoNo | Yes | Not mentioned | (I) Removal of peritoneal catheter and EVD | Bacterial ventri-culitis | - | Death |
| Murali R, et al., (2008) | Congenital Hydrocephalus | 6 m /M | 6 yr | 5.6 yr | No | No | No | NoNo | No | Stomach | (I) Removal of part of peritoneal catheter +EVD, (II) Removal of cranial catheter tried - failed, etc | Nil | 24 m | Well |
| Sridhar K, et al., (2009) | Meningitis with Hydrocephalus | 2 m /F | 8 m | 6 m | No | No | No | NoNo | No | Stomach /Jejunum | (I) Removal of entire VPS catheter | Nil | 12 m | Well |
| Sinnadurai M, et al., (2009) | Hydrocephalus due to arachnoid cyst | 12 yr / F | 27 yr | 2 week | No | Yes | No | NoNo | No | Stomach | (I) Removal of part of peritoneal catheter +EVD,(II) Delayed revision of peritoneal catheter | Nil | 2 m | Well |
| Low SW, et al., (2010) | Meningitis with Hydrocephalus | 6 m / M | 1 yr | 6 m | Yes | No | No | NoNo | No | Stomach | (I) Removal of entire VPS catheter + EVD,(II) Delayed re-VPS | Nil | 12 m | Well |
| Dua R, et al., (2011) | Myelomenigocele and Congenital Hydrocephalus | 20 day /M | 8 m | 7 m | No | No | No | NoNo | No | Stomach | (I) Removal of part of peritoneal catheter +EVD,(II) Delayed re-VPS | Nil | 12 m | Well |
| Agarwal M, et al., (2011) | Congenital Hydrocephalus | 4 m /M | 1 yr | 8 m | No | No | No | NoNo | No | Not mentioned | (I) Removal of entire VPS catheter,(II) Delayed re-VPS | Nil | 12 m | Well |
| Gupta M, et al., (2012) | Congenital Hydrocephalus | 6 m /M | 4 yr | 3.6 yr | No | No | No | NoNo | No | Stomach | (I) Removal of entire VPS catheter | Nil | 12 m | Well |
| Kundal VK, et al., (2012) | Post-meningitis Hydrocephalus | 6 yr / M | 7 yr | 1 yr | No | No | No | NoNo | No | Not mentioned | (I) Removal of entire VPS catheter,(II) Delayed re-VPS | Nil | 18 m | Well |
| Yilmaz MB, et al., (2013) | Pseudotumor cerebri | 37 yr / F | 47 yr | 10 yr | No | Yes | No | NoNo | No | Stomach | (I) UGI Endoscopy +Exp lap + removal of entire VPS catheter | Nil | - | Well |
| Gupta R, et al., (2014) | Congenital Hydrocephalus | 1 yr / M | 11 yr | 7 m | No | Yes | No | NoNo | No | Stomach | (I) Removal of entire VPS catheter | Nil | 10 m | Well |
| Mandhan P, et al., (2015) | Myelomenigocele and Hydrocephalus (Arnold-Chiari malformation) | Infancy /F | 11 yr | 4.5 yr | Yes | Yes | No | NoNo | No | Stomach | (I) UGI Endoscopy +Laparoscopic removal of peritoneal catheter, (II) Delayed removal of cranial catheter | Nil | 3 m | Well |
| Thiong’o GM, et al., (2015) | Congenital Hydrocephalus | 10 days/F | 3 m | 80 days | No | No | No | NoNo | No | Not mentioned | (I) Removal of entire VPS catheter + EVD, (II) Delayed re-VPS | Nil | 12 m | Well |
| Sohal AS, et al., (2015) | Congenital Hydrocephalus | ?/ M | 11 m | 10 days | Yes | Yes | No | NoNo | No | Stomach | (I) Removal of part of peritoneal catheter +EVD,(II) Delayed VA Shunt | Nil | - | Well? |
| Ghritlaharey RK. (2015) | Infective / Congenital Hydrocephalus | 1 yr /F | 2 yr | 9 m | No | Yes | No | NoNo | No | Stomach? | (I) Removal of part of peritoneal catheter +EVD,(II) Delayed revision of peritoneal catheter | Extrusion of peritoneal catheter at abd wound | 2 m | Well |
CSF - Cerebro Spinal Fluid; Exp lap - Exploratory laparotomy; EVD - External Ventricular Drainage; F - Female; GI Surg - Gastrointestinal Surgery; M - Male; m - months; Pre-op - Pre-operative; Post-op - Post-operative; Surg - Surgery; UGI - Upper Gastro-Intestinal; VA shunt - Ventriculo-Atrial shunt, VPS - Ventriculo-Peritoneal Shunt; yr – year
Site of bowel perforation by VPS catheter (n=22).
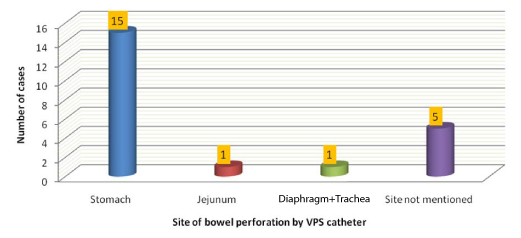
Clinical presentation, investigations ordered, and the surgical procedures executed for the management of peroral extrusion of the VPS catheter by various authors are given in [Table/Fig-3]. None of the case had peritonitis either in pre-operative period, or developed peritonitis following removal of peroral extruded part of VPS catheter or otherwise. During the management of peroral extrusion of VPS catheter there were two deaths; one due to shunt malfunction leading to brain stem herniation and in second case death occurred due to bacterial ventriculitis [10,17].
Clinical presentation, investigation and treatment done for peroral extrusion of VPS catheter.
Discussion
Hippocrates, (460–377 BC), is thought to be the first physician to attempt and document the treatment of hydrocephalus [32]. Kausch in 1908 introduced the use of peritoneal cavity for CSF absorption in VP shunting, and since then VPS implantation is amongst the most frequently performed operation in the management of hydrocephalus [1–8]. Complications are known to occur following VPS insertion and reportedly occured in approximately one-fifth to four-fifth of the cases, and many of them require shunt revisions [1,2,4–8]. Bowel perforation and peroral extrusion of distal/peritoneal part of VPS catheter is an extremely rare complication following VPS insertion. Twenty of 22 (90.9%) reported cases were children, and one of the reason for more number of complications, including peroral extrusion of VPS catheter occurring in children than adult population following VPS placement may be due to the fact that the number of VPS insertion done in infants and children are many fold more as compared to the VPS placement done in adult population. Extrusion of VPS catheter through vaginal orifice and urethra has also been reported in literature [33,34].
Regarding interval of peroral extrusion of VPS catheter, in 40% (n=9) of the cases it occurred within 6-months of VPS insertion/last shunt revision. This observation was quite similar to the fact that in the cases of extrusion of VPS catheter through rectum/anal canal following colon perforation, approximately 50% of the cases reported within 6- months following VPS insertion/last shunt revision [3,7,29,35–37]. On review of 22 cases of peroral extrusion of VPS catheter, all of them presented with extrusion of peritoneal part of the VPS catheter through mouth, and none of them had features of peritonitis at the time of presentation. Occurrence of peritonitis following bowel/colon perforation by VPS catheter is not a rule, and not reported in most of the cases [3,7,9,29,33,35–37]. Rarely peritonitis is there following colon perforation and extrusion of VPS catheter through anal canal [38]. Possibly for similar reasons like colon perforation and per-rectal extrusion of VPS catheter there were no peritonitis even though there was perforation of stomach (most commonly), and jejunum by the VPS catheter in the cases of peroral extrusion of VPS catheter [10–31].
Although the clinical diagnosis of peroral extrusion of VPS catheter was obvious in all the cases, but investigations were needed to confirm or exclude the continuity of the shunt catheter, presence or absence of gas under the diaphragm, and peritoneal fluid collections. Skiagram of the abdomen and chest was amongst the most commonly advised investigation by the authors. In selected cases cranial CT scan was also advised [10–31]. Upper Gastrointestinal (GI) endoscopic evaluation was also done in 3 of the cases, and was helpful in confirming that the shunt catheter pierced the stomach and extruded per-orally [13,26,28]. CSF sample were usually obtained while doing shunt removal or otherwise. Laparoscopic technique was also used once for the diagnosis and therapy for the gastric perforation followed by peroral extrusion of VPS catheter [28]. Various mechanisms are given for the occurrence of the peroral extrusion of VPS catheter and are age (infants and child), malnutrition, shunt infection, prior abdominal surgery, prior shunt revision, shunt allergy, muscle weakness, length of peritoneal catheter, and shunt material [10–31]. Past history of shunt revisions and prior history of abdominal or GI surgery also play an important role for the occurrence of bowel perforation and peroral extrusion of VPS catheter. Nine (40.9%) of 22 had past history of shunt revision, n=7 (31.8%) had prior history of abdominal/GI surgery, and only n=2 (9.09%) had shunt tract infection.
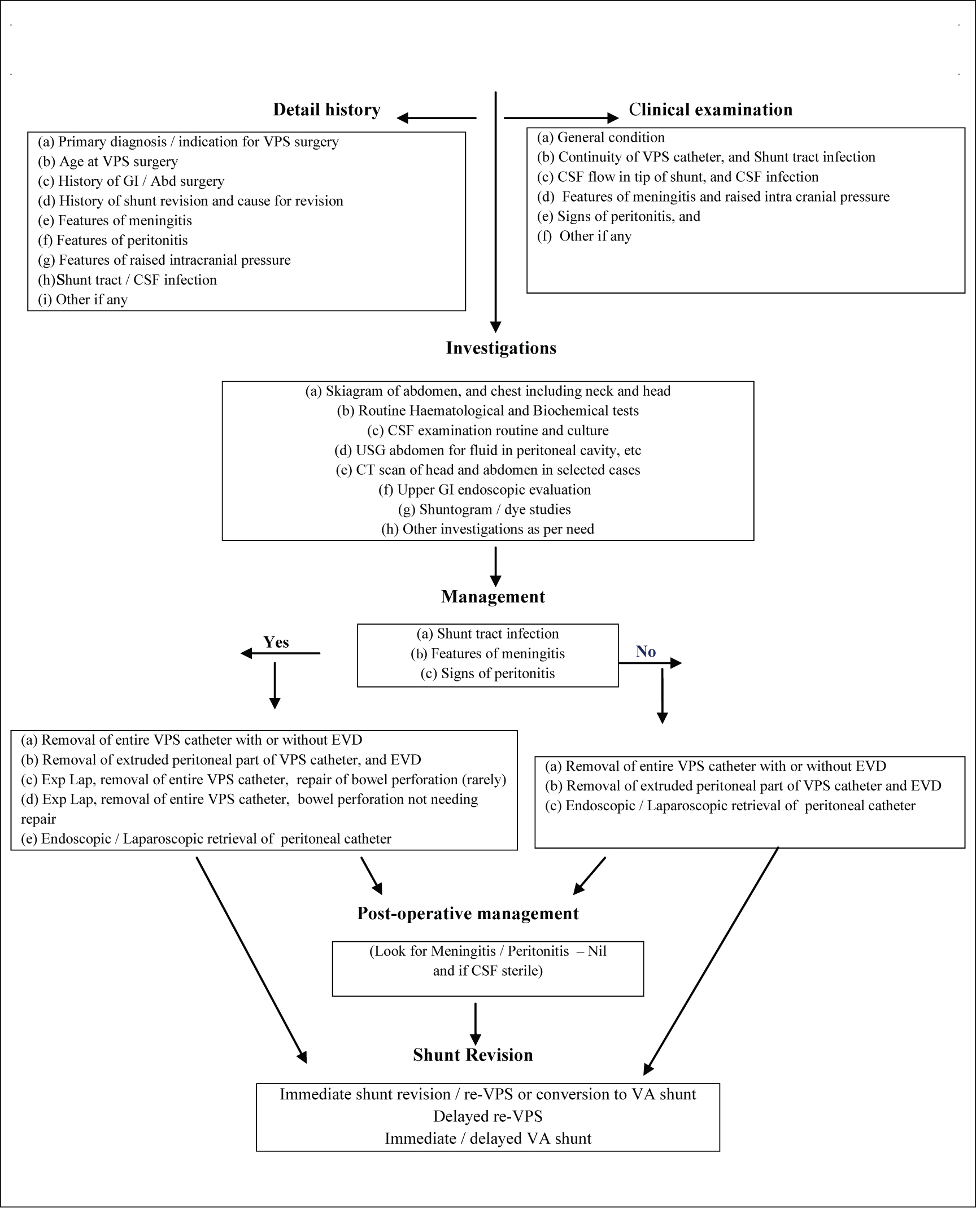
Management of peroral extrusion of VPS catheter differed from case to case and depends upon the presence or absence of shunt or shunt tract infection, CSF infection, meningitis, and peritonitis. A standard guideline or protocol is not available on how to manage a case of peroral extrusion of VPS catheter, and therefore authors used different modalities for managing the case. Various techniques used to treat the cases of peroral extrusion of VPS catheter by authors in order of frequency are given in [Table/Fig-3]. The main objective during the management of peroral extrusion of VPS catheter was to remove the per-orally extruded part of VPS catheter, with or without External Ventricular Drainage (EVD) and delayed re-VPS or shunt revision. During postoperative period none of the case developed peritonitis, although bowel perforation was repaired only at two occasions. Laparoscopic techniques are also frequently used not only for the placement of distal catheter during VPS insertion, but also for the management of abdominal complication of VPS and during shunt revisions. The advantages of doing laparoscopic assisted placement of peritoneal catheter or revision of distal part of VPS catheter is that it is less invasive, allow better catheter positioning, and during revision surgery it also provide better vision for adhesiolysis of the fibrotic adhesions, and also associated with fewer complications than laparotomies done for VPS catheter insertion, or during revision surgery [5,39,40–42]. Laparoscopic retrieval of distal part of VPS catheter was employed only by one author for the management of peroral extrusion of VPS catheter. This laparoscopic technique helped in adhesiolysis of fibrous adhesions and visualization of the site of perforation (stomach) by the shunt catheter, although authors used upper GI endoscopy for shunt catheter retrieval prior to laparoscopic procedure, but failed [28].
A management plan is proposed for the management of peroral extrusion of VPS catheter, and detail described in [Table/Fig-4]. This plan is based on the findings of this review. The basic objectives of management in such a case are: (a) removal of per-orally extruded part of VPS catheter or removal of entire VPS catheter; (b) EVD; and (c) delayed re-VPS or shunt revision. It would be a better option to minimally explore; preferably at abdominal site (site used for insertion of peritoneal catheter) under local anaesthesia, pull out the distal part of peritoneal catheter for a few inches, and cut it into two parts: (a) cranial and (b) distal; part (b) distal part / per-orally extruded part of VPS catheter can be now easily pulled out proximally, and part (a) cranial part of the VPS catheter may be used as EVD if CSF is draining well. If removal of entire VPS catheter is required, incision at cranial site is preferable. It is must to obtain CSF sample at this time, and observe the patient for 2-3 days prior to starting oral feeds. Once CSF is sterile (if infected) and have no signs of peritonitis, one may consider for delayed re-VPS/shunt revision. If there is meningitis/CSF infection, it is mandatory to wait for few more days to weeks. Formal exploratory laparotomy is not advisable for shunt removal and also not preferable to mini-laparotomy during re-VPS/shunt revision. Laparoscopic technique with its added advantages is a promising tool for placement of peritoneal catheter during re-VPS/shunts revision.
Proposed management plan for peroral extrusion of VPS catheter by R K Ghritlaharey (2016).
VPS - Ventriculoperitoneal shunt; EVD - External Ventricular Drainage; GI - Gastrointestinal; Abd - Abdomen; CSF - Cerebrospinal Fluid; USG - Ultrasonography; VA - Ventricular Atrial; Exp Lap - Exploratory laparotomy; C/S - Culture/Sensitivity
Limitations of this review are that the number of the cases was limited and various authors have used different ways for managing the case of peroral extrusion of VPS catheter following VPS placement. As defined guidelines for management of such cases is lacking, I believe that authors have managed their cases based on their personal experience in dealing with other VPS related complications. The exact cause and mechanism for stomach being the commonest site for entry by peritoneal part of VPS catheter is not known. In n=5 (22.7%) of the reviewed cases the entry site in bowel by peritoneal part of VPS catheter was not known. Cases of peroral extrusion of VPS catheter following VPS placement, published/available in language other than English, were not included in this review, except one.
Conclusion
Peroral extrusion of peritoneal part of VPS catheter is a rare complication following VPS insertion. In more than two-third of the cases it occurred within one-year of the VPS placements or last shunt revision, so a close follow-up is a must during this period following VPS placement. Clinical diagnosis was obvious due to peroral extrusion of VPS catheter. Defined guidelines does not exist for the management of peroral extrusion of VPS catheter, and management mainly relies upon presence or absence of shunt tract infection, CSF infection, peritonitis, and meningitis.
CSF - Cerebro Spinal Fluid; Exp lap - Exploratory laparotomy; EVD - External Ventricular Drainage; F - Female; GI Surg - Gastrointestinal Surgery; M - Male; m - months; Pre-op - Pre-operative; Post-op - Post-operative; Surg - Surgery; UGI - Upper Gastro-Intestinal; VA shunt - Ventriculo-Atrial shunt, VPS - Ventriculo-Peritoneal Shunt; yr – year
[1]. Smith JL, Management of neural tube defects, hydrocephalus, refractory epilepsy, and central nervous system infections. Coran AG, Adzick NS, Krummel TM, Laberge JM, Shamberger RC, et al (eds)In: Pediatric Surgery 2012 7th edElsevier Inc:1673-97. [Google Scholar]
[2]. Wang JY, Jackson EM, Jallo GI, Ahn ES, Shunt revision requirements after posthemorrhagic hydrocephalus of prematurity: insight into the time course of shunt dependencyChilds Nerv Syst 2015 31:2123-30. [Google Scholar]
[3]. Ghritlaharey RK, Budhwani KS, Shrivastava DK, Gupta G, Kushwaha AS, Chanchlani R, Trans-anal protrusion of ventriculo-peritoneal shunt catheter with silent bowel perforation: report of ten cases in childrenPediatr Surg Int 2007 23:575-80. [Google Scholar]
[4]. Notarianni C, Vannemreddy P, Caldito G, Bollam P, Wylen E, Willis B, Congenital hydrocephalus and ventriculoperitoneal shunts: influence of etiology and programmable shunts on revisionsJ Neurosurg Pediatr 2009 4:547-52. [Google Scholar]
[5]. Naftel RP, Argo JL, Shannon CN, Taylor TH, Tubbs RS, Clements RH, Laparoscopic versus open insertion of the peritoneal catheter in ventriculoperitoneal shunt placement: review of 810 consecutive casesJ Neurosurg 2011 115:151-58. [Google Scholar]
[6]. Nigim F, Critchlow JF, Schneider BE, Chen C, Kasper EM, Shunting for hydrocephalus: analysis of techniques and failure patternsJ Surg Res 2014 191:140-47. [Google Scholar]
[7]. Ghritlaharey RK, Budhwani KS, Shrivastava DK, Srivastava J, Ventriculoperitoneal shunt complications needing shunt revision in children: a review of 5 years of experience with 48 revisionsAfr J Paediatr Surg 2012 9:32-9. [Google Scholar]
[8]. Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ, Revision rate of pediatric ventriculoperitoneal shunts after 15 yearsJ Neurosurg Pediatr 2013 11:15-9. [Google Scholar]
[9]. Hai A, Rab AZ, Ghani I, Huda MF, Quadir AQ, Perforation into gut by ventriculoperitoneal shunts: A report of two cases and review of the literatureJ Indian Assoc Pediatr Surg 2011 16:31-33. [Google Scholar]
[10]. Griffith JA, DeFeo D, Peroral extrusion of a ventriculoperitoneal shunt catheterNeurosurgery 1987 21:259-61. [Google Scholar]
[11]. Danismend N, Kuday C, Unusual complication of ventriculoperitoneal shuntNeurosurgery 1988 22:798 [Google Scholar]
[12]. Fermin S, Fernández-Guerra RA, Sureda PJ, Extrusion of peritoneal catheter through the mouthChilds Nerv Syst 1996 12:553-55. [Google Scholar]
[13]. Park CK, Wang KC, Seo JK, Cho BK, Transoral protrusion of a peritoneal catheter: a case report and literature reviewChilds Nerv Syst 2000 16:184-89. [Google Scholar]
[14]. Jiménez Moya A, Penela Vélez De Guevara T, Gracia Remiro R, Romero Escós D, Santana Rodríguez C, Reig Del Moral C, Extrusion of a ventriculoperitoneal shunt catheter through the mouthAn Esp Pediatr 2001 54:609-10. [Google Scholar]
[15]. Kothari PR, Shankar G, Kulkarni B, Extruded ventriculo-peritoneal shunt: An unusual complicationJ Indian Assoc Pediatr Surg 2006 11:255-56. [Google Scholar]
[16]. Odebode TO, Jejunal perforation and peroral extrusion of a peritoneal shunt catheterBr J Neurosurg 2007 21:235-36. [Google Scholar]
[17]. Berhouma M, Messerer M, Houissa S, Khaldi M, Transoral protrusion of a peritoneal catheter: a rare complication of ventriculoperitoneal shuntPediatr Neurosurg 2008 44:169-71. [Google Scholar]
[18]. Murali R, Ravikumar V, Transoral migration of peritoneal end of ventriculoperitoneal shunt: A case report of a rare complication and review of literatureJ Pediatr Neurosci 2008 3:166-68. [Google Scholar]
[19]. Sridhar K, Karmarkar V, Peroral extrusion of ventriculoperitoneal shunt: Case report and review of literatureNeurol India 2009 57:334-36. [Google Scholar]
[20]. Sinnadurai M, Winder MJ, Silicone spaghettiJ Clin Neurosci 2009 16:1348-50. [Google Scholar]
[21]. Low SW, Sein L, Yeo TT, Chou N, Migration of the abdominal catheter of a ventriculoperitoneal shunt into the mouth: A rare presentationMalays J Med Sci 2010 17:64-7. [Google Scholar]
[22]. Dua R, Jain R, Peroral extrusion of ventriculoperitoneal shunt: a case report and review of the literatureCent Eur Neurosurg 2011 72:107-08. [Google Scholar]
[23]. Agarwal M, Adhana R, Namdev H, Yadav R, Agrawal T, Transoral extrusion of the ventriculo-peritoneal shunt: A case report and review of literatureJ Pediatr Neurosci 2011 6:149-51. [Google Scholar]
[24]. Gupta M, Digra NC, Sharma N, Goyal S, Agrawal A, Peroral extrusion of the peritoneal catheter in an infantN Am J Med Sci 2012 4:290-91. [Google Scholar]
[25]. Kundal VK, Gajdhar M, Sharma C, Agrawal D, Kundal R, Wandering distal end of ventriculo-peritoneal shunt: Our experience with five cases and review of literatureJ Nepal Paediatr Soc 2012 32:266-69. [Google Scholar]
[26]. Yilmaz MB, Egemen E, Tonge M, Kaymaz M, Transoral protrusion of a peritoneal catheter due to gastric perforation 10 years after a ventriculoperitoneal shunting: case report and review of the literatureTurk Neurosurg 2013 23:285-88. [Google Scholar]
[27]. Gupta R, Mala TA, Gupta A, Paul R, Malla SA, Gupta AK, Transoral migration of peritoneal end of ventriculoperitoneal shunt with perforation of gastro-esophageal junction: a case report of a rare complicationBangladesh J Med Sci 2014 13:492-95. [Google Scholar]
[28]. Mandhan P, Wong M, Samarakkody U, Laparoscopic removal of peroral extrusion of a ventriculoperitoneal shuntAsian J Endosc Surg 2015 8:95-97. [Google Scholar]
[29]. Thiong’o GM, Luzzio C, Albright AL, Ventriculoperitoneal shunt perforations of the gastrointestinal tractJ Neurosurg Pediatr 2015 16:36-41. [Google Scholar]
[30]. Sohal AP, Whittle V, Nicholson C, Kisler J, Where did the oral tube originate from?J Paediatr Child Health 2015 51:738-40. [Google Scholar]
[31]. Ghritlaharey RK, Extrusion of ventriculoperitoneal shunt catheter through mouth in a two-year-old girl: A case reportInt J Clin Pediatr Surg 2015 1:1-4. [Google Scholar]
[32]. Lifshutz JI, Johnson WD, History of hydrocephalus and its treatmentsNeurosurg Focus 2001 11:E1 [Google Scholar]
[33]. Kumar B, Sharma SB, Singh DK, Extrusion of ventriculo-peritoneal shunt catheterIndian J Pediatr 2010 77:336 [Google Scholar]
[34]. Kataria R, Sinha VD, Chopra S, Gupta A, Vyas N, Urinary bladder perforation, intra-corporeal knotting, and per-urethral extrusion of ventriculoperitoneal shunt in a single patient: case report and review of literatureChilds Nerv Syst 2013 29:693-97. [Google Scholar]
[35]. Mohta A, Jagdish S, Spontaneous anal extrusion of ventriculoperitoneal shuntAfr J Paediatr Surg 2009 6:71-72. [Google Scholar]
[36]. Vuyyuru S, Ravuri SR, Tandra VR, Panigrahi MK, Anal extrusion of a ventriculo peritoneal shunt tube: Endoscopic removalJ Pediatr Neurosci 2009 4:124-26. [Google Scholar]
[37]. Bansal H, Gupta G, Gupta M, Kaushal R, Unusual ventriculoperitoneal (VP) shunt tube extrusion through anus in a child with Dandy Walker malformation: A rare case reportJ Clin Diagn Res 2015 9:PD25-26. [Google Scholar]
[38]. Chiang LL, Kuo MF, Fan PC, Hsu WM, Transanal repair of colonic perforation due to ventriculoperitoneal shunt—case report and review of the literatureJ Formos Med Assoc 2010 109:472-75. [Google Scholar]
[39]. Pinto FC, de Oliveira MF, Laparoscopy for ventriculoperitoneal shunt implantation and revision surgeryWorld J Gastrointest Endosc 2014 6:415-18. [Google Scholar]
[40]. Abouhashem S, Taha MM, Ismail A, El Rashed M, Laparoscopic revision of the distally obstructed ventriculoperitoneal shuntTurk Neurosurg 2013 23:61-6. [Google Scholar]
[41]. Johnson BW, Pimpalwar A, Laparoscopic-assisted placement of ventriculo-peritoneal shunt tips in children with multiple previous open abdominal ventriculo-peritoneal shunt surgeriesEur J Pediatr Surg 2009 19:79-82. [Google Scholar]
[42]. Phan S, Liao J, Jia F, Maharaj M, Reddy R, Mobbs RJ, Laparotomy vs minimally invasive laparoscopic ventriculoperitoneal shunt placement for hydrocephalus: A systematic review and meta-analysisClin Neurol Neurosurg 2016 140:26-32. [Google Scholar]