Multidisciplinary Restoration of Traumatized and Displaced Maxillary Central Incisor by Bent Wire System-A Novel Approach
Shilpa S Sasalawad1, Vivek Jogani2, Suryakanth M Pai3, Rashmi C Chour4, Deepti V Balehosur5
1 Assistant Professor, Department of Pedodontics and Preventive Dentistry, College of Dental Sciences, Davangere, Karnataka, India.
2 General Practioner, Dr. Jogani’s Dental Clinic, Mumbai, Maharastra, India.
3 General Practioner, Densure Clinic, Mangaluru, Karnataka, India.
4 Assistant Professor, Department of Pedodontics and Preventive Dentistry, PMNM Dental College, Bagalkot, Karnataka, India.
5 Assistant Professor, Department of Pedodontics and Preventive Dentistry, College of Dental Sciences, Davangere, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shilpa S Sasalawad, Assistant Professor, Department of Pedodontics and Preventive Dentistry, College of Dental Sciences, Pavallion Road, Davangere-577004, Karnataka, India.
E-mail: shilpa.sasalawad@gmail.com
Management of traumatic injuries to teeth is a challenge to dental practice, as it occurs when dentists are least prepared for it. The direction and the force of the object or the fall significantly affects the diagnosis, treatment plan and therefore the outcome of the treatment. These traumatic injuries may present with different clinical situations which demand immediate attention and assessment by the clinician. The maxillary central incisor crown fractures are the most common variant of trauma, because of the anterior and protrusive positioning. This case report describes the novel method to produce expansion of the dental arches to correct the post-traumatic displacement of the central incisor along with aesthetic and functional rehabilitation of Ellis Class IV fracture of permanent maxillary central incisor.
Holistic approach, Prevention, Traumatic injury
Case Report
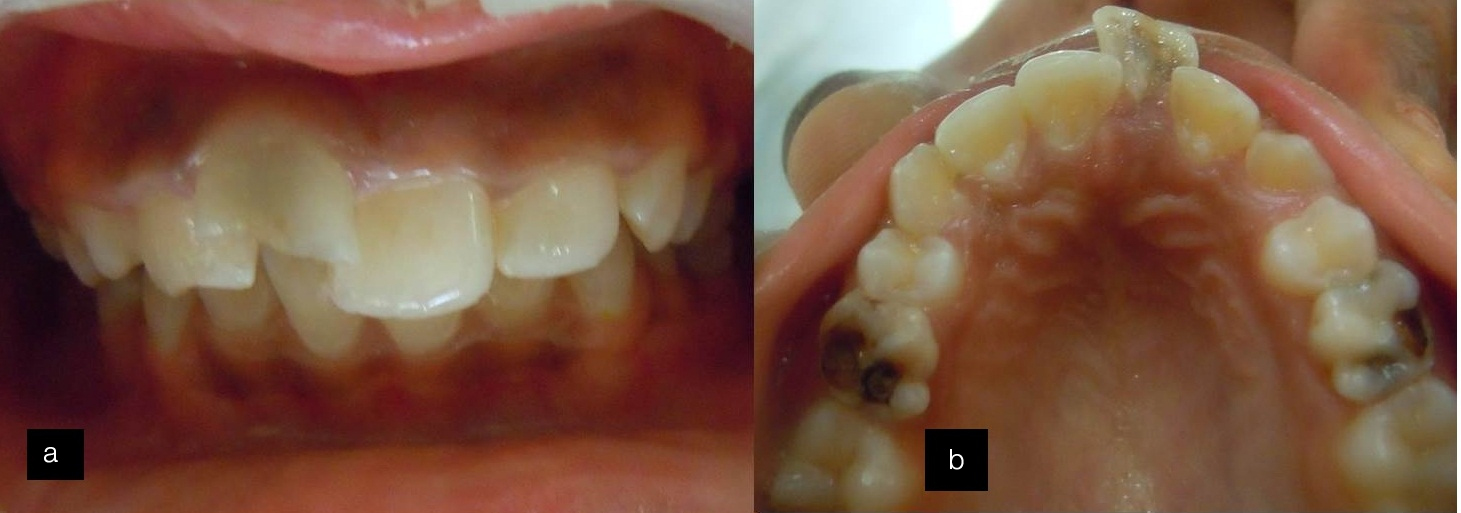
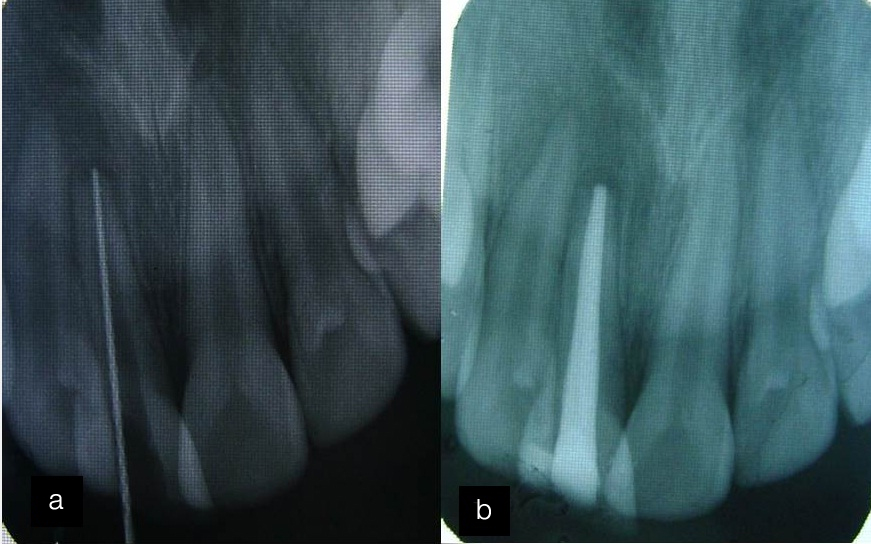
A 10-year-old female patient reported to the Department of Pedodontics and Preventive Dentistry, with a chief complaint of discolored and broken front teeth. History of present illness stated trauma to upper front teeth two years back due to self-fall on road. The teeth were painful and there was bleeding at the site of trauma. The parents could not retrieve the broken piece. Her medical history was non–contributory. Past dental history reveled that parents had consulted a local dentist for first aid treatment but, they could not keep up the regular appointments. On extra-oral examination, patient had potentially competent lips, convex profile and hyperactive mentalis muscle [Table/Fig-1]. Intra-oral examination revealed Ellis Class IV fracture of tooth #11, Ellis Class I fracture of tooth #12, along with labial displacement of tooth #11. Occlusal caries were seen in tooth #55, 65 which exhibited pre-shedding mobility. Patient had deep bite and proclined maxillary anterior teeth [Table/Fig-2a,b]. An Intra-Oral Periapical Radiograph (IOPAR) of tooth #11, showed resorption of the root with slight widening of the apex [Table/Fig-3]. After evaluating the data, multidisciplinary approach for aesthetic rehabilitation of the traumatized teeth was planned. The first step was to carry out the root canal treatment for the non-vital teeth. At the same appointment, root canal treatment was initiated, access cavity was prepared and working length was determined using radiographic method. In the next appointment biomechanical preparation was done followed by obturation with gutta-percha [Table/Fig-4a,b]. Next step was to align the displaced tooth in the arch by using Bent Wire System (BWSTM) designed by Myoresearch Company.
Extra-oral photographs (a) Frontal view; (b) Lateral view.

Intra-oral photographs illustrating (a) Discolored and fractured tooth #11; (b) Labial displacement of tooth #11.
Intra-oral periapical radiograph showing resorption of the root with slight widening of the apical opening.

Intra-oral periapical radiographs (a) Working length determination; (b) Obturation with gutta-percha.
Fabrication of the appliance: The permanent maxillary first molars were banded and a lingual sheath was spot welded to them following which the bands were cemented to the respective teeth with Type I glass ionomer cement. The bent wire component was made from 0.7mm stainless steel wire. The anterior section was shaped according to ideal arch. At the distal end of the canines, “S” bend was formed around the first premolar or the deciduous first molar using hollow jaw pliers. Using the loop forming pliers a “U” loop of 5-7mm wide was formed between deciduous molar and permanent first molar. All bends should be in single plane. In the present case, loop was made in the maxillary anterior region to gain more space for the retroclination of the incisors and was little modified for this patient with acrylic button and brackets embedded in them to train the tongue along with a labial bow for alignment of anterior teeth [Table/Fig-5a,b].
Placement of bent wire system (a) Maxillary arch view; (b) Frontal view.
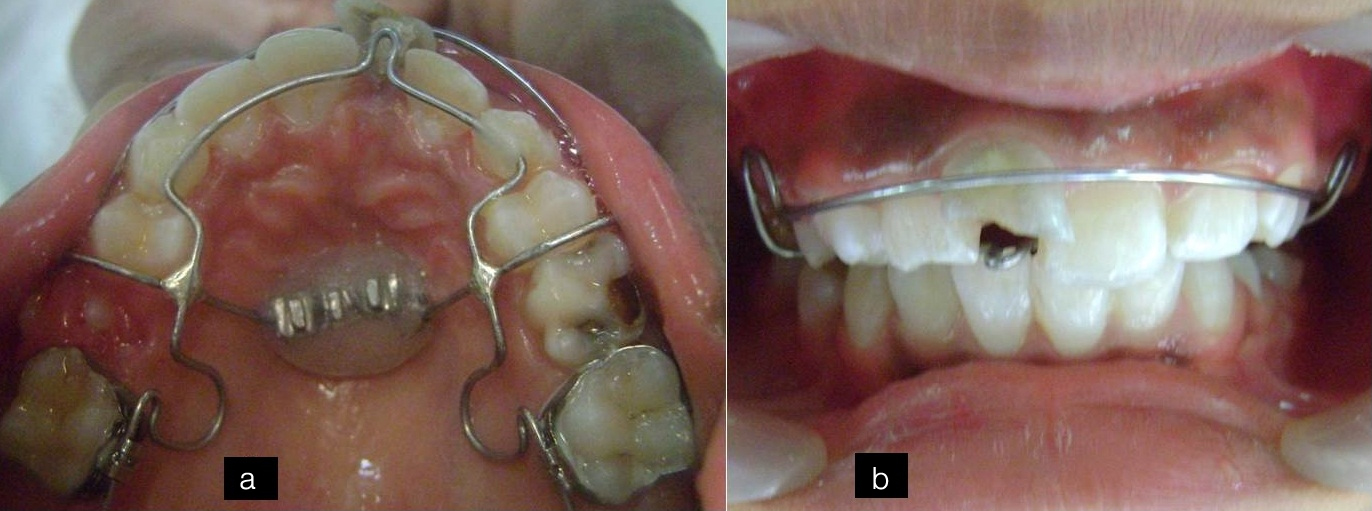
Activation of the Appliance: After delivery of the appliance, the patient was called every week for activation of the appliance by opening the loop in the anterior and posterior region. Activation of the loops should be no more than 1mm initially, subsequently 1-2mm every 3-4 weeks.
Follow-up: After five months, the maxillary central incisors were aligned into proper position in the arch [Table/Fig-6a,b]. The positions of the teeth were retained with the help of Hawley’s appliance for one year. After one year of retention, the aesthetic rehabilitation of the tooth was planned. Crown preparation was done following which polycarbonate crown was cemented and patient was recalled every six months, but patient reported with repeated failure of the temporary crowns, following which the placement of Porcelain Fused to Metal (PFM) crown was decided as tooth was already non-vital and root canal treated. PFM crown was fabricated, cemented [Table/Fig-7a-c] and radiographic assessment was done by IOPAR [Table/Fig-8]. Composite restoration was done in tooth #12 which exhibited Ellis Class I fracture. The patient was happy and satisfied with functional and aesthetic rehabilitation.
After five months follow-up (a) Maxillary arch view showing well aligned of the incisors; (b) Frontal view of the anterior teeth.

Esthetic rehabilitation of central incisor (a) Tooth preparation (b) Cementation of PFM crown (c) Arch view of the crown.

Intra-oral periapical radiograph after the cementation of the PFM crown with tooth #11.

Discussion
Oro-facial trauma occurs often and constitutes 5% of all injuries for which people seek treatment. In pre-school children, the percentage is, as high as 18% [1]. The dental trauma is a serious problem in children and adolescents; its prevalence has increased in recent decades as reported by some studies. Most of the traumatic injuries of teeth constitute coronal fractures which account for 26%-76% of dental injuries and 16% of which are complicated fractures involving pulp [2]. The prevalence of dental traumatic injuries ranges from 13.8-15.1%. The most common causes for traumatic dental injury are falls and collision. The maxillary central incisors are the most common teeth affected during trauma [3]. More than 20% of children experience damage to their permanent dentition by 14 years of age, with men outnumbering women (2:1) and peak incidence at 8 to 10 years of age. Aesthetic and functional rehabilitation is the primary goal of treatment of fractured tooth [4].
An external impact on tooth, direct or indirect leads to traumatic injuries. Assault to teeth may lead to luxation injuries, injury to vital organ of the tooth i.e., pulp, with or without the loss of tooth structure, or fracture of the root. Enamel fractures account for 67% of all dental injuries; subsequently enamel-dentin fractures with 25.3%. The severity of the injury may vary from simple crown fractures to complicated crown root fractures [5]. Dental trauma is an accidental event and an emergency situation in young patients, as young permanent teeth are in process of development. Any damage to tooth at this stage may compromise the development and overall life of the tooth involved. Besides representing a considerable proportion of dental emergencies, these injuries cause aesthetic and psychological problems in children [6].
In the present case, BWSTM was used as it is a new and noble appliance to gain the space in the anterior segment. It is a light wire appliance that offers additional arch development. It is best suited for patients between 8-15 years of age. The majority who require treatment in the late-mixed, early permanent dentition often require arch expansion. The BWSTM is an effective appliance to gain the space in the anterior segment of the arch, when used along with myobrace and trainer systems. The simple nature of the BWSTM makes it possible to assemble in-house, can be constructed “in office”, avoiding the fees that accompany laboratory-constructed appliances [7].
The system has been developed by Myofunctional Research Co. (MRC), Queensland, Australia, as a simpler method for expansion of arches. It produces better stability with simultaneous correction of habit. An advantage of this system is that it does not involve using acrylic in the palatal vault which allows the free movement of the tongue [8]. There is a controversy regarding the ideal time for performing the expansion. Sari Z et al., reported that rapid maxillary expansion by means of fixed screws (e.g., Hyrax) produces better results when it is performed in the early permanent dentition [8]. Although this statement is supported by other authors [9–11], but it can also be successfully done in adults [12–14]. Nevertheless, maxillary and mandibular expansion rises up as one of the important phase of orthodontic treatment producing arch perimeter increase, and so, avoiding extraction of teeth [15]. In this case, space was needed for the alignment of displaced incisor, instead of making the child wait till the eruption of all permanent teeth and subject the patient to fixed orthodontic treatment. We decided to align the teeth in the arch using this novel approach.
Although controversy has persisted over the stability of these techniques, definitely there is increasing trend towards “non-extraction”. The BWSTM is an excellent alternative form of treatment in those cases where arch development is required to align teeth, patients want to minimize or even avoid brackets and extractions, soft tissue dysfunction is present and treatment needs to be performed in a reasonable period of time.
Conclusion
Dental trauma is an unanticipated event that requires professional preparation. The management of dental injuries is an evolving science. Some traditional treatment options have stood over the years. With advancement in technology and science, new materials and methods evolve to prove, disprove or facilitate approaches to management of these injuries. Practioners need to be always aware of changes that occur from time to time. Traumatic injuries to teeth need immediate attention. Therefore, pre-school teachers and parents should have thorough knowledge about preventive measures and first aid management of these traumatic injuries.
[1]. Poi WR, Cardaso LC, Castro JCM, Cintra LTA, Gulinelli JL, Lazari JAB, Multidisciplinary approach for crown fracture and crown-root fracture-A case reportDent Traumatol 2007 23:51-55. [Google Scholar]
[2]. Martos J, Nascimento CN, Collares KF, Silveira LF, Trauma in permanent central incisor with crown fracture treated by direct restorationJ Pediatr Dent 2013 1:24-26. [Google Scholar]
[3]. Mishra L, Kumar M, Rehabilitation of fractured tooth by a custom made fibre reinforced composite postInt J Odontostomat 2012 6(3):323-26. [Google Scholar]
[4]. Moule AJ, Moule CA, Minor traumatic injuries to the permanent dentitionDent Clin North Am 2009 53(4):639-59. [Google Scholar]
[5]. Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, International Association of Dental Traumatology, International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teethDent Traumatol 2012 28(1):2-12. [Google Scholar]
[6]. Moule AJ, Moule CA, The endodontic management of traumatized permanent anterior teeth: A reviewAust Dent J 2007 52(1 Suppl):S122-37. [Google Scholar]
[7]. Stuart DA, Wilkshire WA, Rapid palatal expansion in the young adult: Time for a paradigm shift?J Can Dent Assoc 2003 69:374-77. [Google Scholar]
[8]. Sari Z, Uysal T, Usumez S, Basciftci FA, Rapid maxillary expansion. Is it better in the mixed or in the permanent dentition?Angle Orthod 2003 73:654-61. [Google Scholar]
[9]. Chung CH, Font B, Skeletal and dental changes in the sagittal, vertical and transverse dimensions after rapid palatal expansionAm J Orthod Dentofacial Orthop 2004 126:569-75. [Google Scholar]
[10]. Housley JA, Nanda RS, Curier GF, McCune DE, Stability of transverse expansion in the mandibular archAm J Orthod Dentofacial Orthop 2003 124:288-93. [Google Scholar]
[11]. Spillane LM, McNamara JA Jr, Maxillary adaptation to expansion in the mixed dentitionSemin Orthod 1995 1:176-87. [Google Scholar]
[12]. Stuart DA, Wilkshire WA, Rapid palatal expansion in the young adult: Time for a paradigm shift?J Can Dent Assoc 2003 69:374-77. [Google Scholar]
[13]. Iseri H, Ozzoy S, Semirapid maxillary expansion – a study of long term transverse effects in older adolescents and adultsAngle Orthod 2004 74:71-78. [Google Scholar]
[14]. Lima RM, Lima AL, Case report: Long-term outcome of Class II, division 1 malocclusion treated with rapid palatal expansion and cervical tractionAngle Orthod 2000 70:89-94. [Google Scholar]
[15]. German O, Ramirez-Yanez Chris Farrell, How to avoid extractions when treating malocclusions using MRC’S Bent wire system and trainer system for arch developmentOrtho Tribune U S Edition 2012 7(4):3-6. [Google Scholar]