Abdominal Necrotising Fascitis Mimicking Peritonitis in a Gatka Playing Indian Male: A Case Report
Sonika Jha1, Devinder Pal Singh2
1 Junior Resident, Department of General Surgery, Government Medical College and Rajindra Hospital, Patiala, Punjab, India.
2 Professor, Department of General Surgery, Government Medical College and Rajindra Hospital, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sonika Jha, Girls Hostel1 Rajindra Hospital, Patiala-147001, Punjab, India.
E-mail: sonikajha29@gmail.com
The present case report is of abdominal Necrotising Fascitis in a young Gatka player. The patient was clinically diagnosed to have peritonitis with plan for laparotomy but since ultrasound abdomen showed no free intra-abdominal fluid and any other pathology a Contrast Enhanced Computed tomography (CECT) abdomen was done. CECT showed fluid collections in rectus sheath and superficial fascia. Patient was thus, diagnosed as having abdominal myofascitis and treated accordingly. A review of literature showed that such a clinical presentation of this disease is quite rare and can lead to unnecessary laparotomy and delay in diagnosis leading to morbidity.
Constipation, Debridement, Myofascitis
Case Report
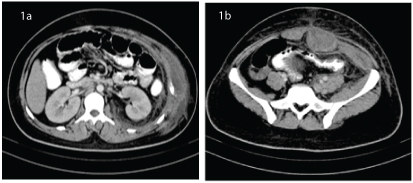
A 25-year-old previously healthy male Gatka enthusiast was referred to the Surgery emergency with a day old lower abdominal, constant, severe and non-radiating pain. He had a history of constipation. The patient also had fever since, the past few days. He was a Gatka player since 2 years and used to sprain abdominal muscles whilst training which according to him was never bothersome. There was no history of vomiting, colicky abdominal pain or urinary urgency, frequency or burning micturition. There was no previous history of minor or major surgery. He had no history of diabetes, Rheumatic Heart Disease (RHD), intravenous drug abuse. On presentation, he was conscious and in significant pain. His pulse was 110 beats per minute, blood pressure was 110/70mmhg and respiratory rate was 28/min. The body temperature was 100°F. Abdomen was slightly distended but normal in appearance. It was rigid and excruciatingly tender to palpation in all regions, especially in the hypogastric region. Bowel sounds were absent. Per rectal examination was normal. An abdominal paracentesis yielded hazy fluid which was sent for bacteriological examination. A working diagnosis of peritonitis was made. Patient was catheterised. He was given Ceftriaxone plus Sulbactam 1.5 gm IV and Ciprofloxacin 500mg IV with Metronidazole 100ml IV along with adequate analgesia. Skiagram chest and abdomen did not show any significant finding. Ultrasound abdomen showed no free fluid in the abdomen, normal peristaltic gut loops and no organ injury. However, the pancreas could not be adequately assessed due to overlying gas shadows. Complete Blood Count (CBC) showed leucocytosis with predominant polymorphs. Blood Urea and serum Creatinine were normal. Serum amylase and lipase were normal. A Contrast Enhanced Computed Tomography (CECT) of the abdomen showed fluid collection in abdominal wall involving bilateral rectus sheaths below the umbilicus [Table/Fig-1a,b]. There was no intra-abdominal pathology.
(a)-CECT abdomen showing fluid in myofascial plain extending laterally up to right flank. (b)-CECT Abdomen at the level of iliac crest showing fluid in superficial fascial planes and large fluid collection in underlying sheath.
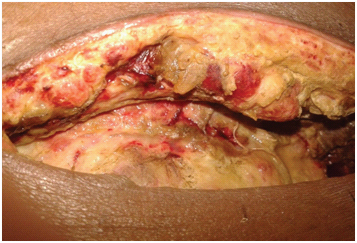
A diagnosis of abdominal wall necrotising fascitis was made. Debridement was done under sedation and short general anaesthesia. A transverse incision approximately 4-cm centred on the midline was given and all necrosed easily separable and avascular tissues were removed [Table/Fig-2]. Two lateral vertical incisions were given along the anterior axillary line centred at the level of the first incision and debridement was done. The cavities thus, created were washed and irrigated with warm normal saline copiously and diluted hydrogen peroxide solution and washed again with warm normal saline.
Diffuse myonecrosis of abdominal muscles and superficial fascia with avascular necrotic tissue but overlying healthy skin.
The culture report showed no growth after 48 hours of incubation. However, an anaerobic culture is not routinely done in our setup.
After 48 hours, patient had persistently raised total leukocyte count and fever with tachycardia. His blood urea, serum creatinine and serum electrolytes were normal. Chest X-ray showed hazy infiltrate but the saturation was maintained at a respiratory rate of 22/min. Considering persistent sepsis, he was started on injection Meropenem 1g IV TDS and Ofloxacin and Ornidazole 100ml IV TDS. A second debridement was done under sedation. After 48 hours, the patient had improved vital signs and the blood counts decreased.
After 11 days of in hospital stay, he was discharged with a healthy wound and advised for alternate day dressing [Table/Fig-3]. The abdominal wounds were closed secondarily after 27 days. He was advised to wear appropriate protective gear while practicing Gatka.
Granulation tissue in the same wound after regular dressing and two debridements.

Discussion
Abdominal necrotising fascitis has been considered to be a disease of the very young or the very old. Risk factors include multiple co-morbidities like malnutrition, uncontrolled diabetes mellitus, poor personal hygiene, history of surgery or instrumentation, immunocompromised state or source of infection like severe pyoderma and lastly penetrating or blunt trauma [1,2]. Abdominal necrotising fascitis is statistically quite unlikely in a young male without these risk factors [3]. Since, the successful outcome is dependent on early diagnosis a high index of suspicion is imperative to early treatment. One of the risk factors for necrotising fascitis is the presence of haematomas. Consideration of sports (Gatka) related wall haematomas lead us to this diagnosis in our patient with local, infra-umbilical pain and systemic signs of sepsis.
Gatka is a Sikh martial art where blunt sticks and swords are used in simulative combat. A common move in Gatka is jumping high with both hips rapidly flexed and the trunk stabilised as the opponents weapon swoops across underneath the jumper, initially aimed at the legs. The jumper simultaneously aims at the opponent’s abdomen. This can entail a significant amount of stretching of anterior abdominal musculature. If repeatedly done, it also leads to formation of small haematomas in the muscle bulk.
While most sports related abdominal injuries either involve the groin or intra-abdominal organs, wall haematomas leading to necrotising fascitis in sportspersons are virtually unheard of [4].
The emergency ultrasound which does not use a superficial probe may miss fluid in the subcutaneous space and appear normal unless there are overlying skin changes which suggest soft tissue infection. Balius et al., have shown how examination with a superficial probe can prove diagnostic in wall related injuries commonly seen in sportspersons. Wall haematomas diagnosed early respond to immobilisation and graded rehabilitation [5]. Wall haematomas present with local signs and symptoms but if accompanied with systemic signs of tachycardia, fever and leucocytosis can indicate abdominal necrotising fascitis as seen in our case. These warrant debridement through an infra umbilical incision and can lead to long term sequelae of decreased sports performance.
We advised a CT to rule out intra-abdominal pathology because we didn’t consider abdominal necrotising fascitis to be likely in our patient. However, an average CECT in our setup requires at least 3-4 hours and leads to delay in definitive life saving debridement thus, worsening prognosis [6]. The first debridement of the patient was done 8 hours after arrival. Delaying debridement to more than twelve hours increases mortality to 30% [7,8]. However, CT did help in planning our incision over the largest fluid collection.
Like many patients with necrotising fascitis our patient also required more than one debridement and culture was negative. This might be due to the fact that, our patient had received intravenous antibiotics before referral.
Conclusion
In conclusion, we can say that a relatively early arrival to our centre, lack of co morbidities, consideration of necrotising fascitis, quick investigation and early debridement and adjunctive antibiotic support and re-look debridement on worsening of general conditions lead us to helping this patient get rid of a deadly disease with a grim prognosis without the need of extensive plastic surgery.
Thus, this case report shows that, Necrotising Abdominal Fascitis can occur even in the young without co-morbidities who are considered statistical outliers often leading to delay in debridement and worsening of prognosis.
[1]. Elliott DC, Kufera JA, Myers RAM, Necrotizing soft tissue infections risk factors for mortality and strategies for managementAnnals of Surgery 1996 224(5):672-83. [Google Scholar]
[2]. Hasham S, Matteucci P, Stanley PRW, Hart NB, Necrotising fasciitisBMJ 2005 330(7495):830-33. [Google Scholar]
[3]. Sadasivan J, Maroju NK, Balasubramaniam A, Necrotizing FasciitisIndian J Plast Surg 2013 46(3):472-78. [Google Scholar]
[4]. Barrett C, Smith D, Recognition and management of abdominal injuries at athletic eventsInt J Sports Phys Ther 2012 7(4):448-51. [Google Scholar]
[5]. Balius R, Pedret C, Pacheco L, Gutierrez JA, Vives J, Escoda J, Rectus abdominis muscle injuries in elite handball players: management and rehabilitationJ Sports Med 2011 2:69-73. [Google Scholar]
[6]. Wong CH, Chang HC, Pasupathy S, Khin LW, Tan JL, Low CO, Necrotizing fasciitis: clinical presentation, microbiology and determinants of mortalityJ Bone Joint Surg Am 2003 85-A:1454-60. [Google Scholar]
[7]. Dapunt U, Klingmann A, Schmidmaier G, Moghaddam A, Necrotising fasciitisBMJ Case Rep 2013 2013:bcr2013201906Published online 2013 Dec 10 [Google Scholar]
[8]. Heitmann C, Pelzer M, Bickert B, Menke H, Germann G, Surgical concepts and results in necrotizing fasciitisChirurg 2001 72(2):168-73. [Google Scholar]