Pancreatic Tuberculosis: A Puzzle for Physicians. A Rare Case and Review of Literature
Prashanth Ashok Kumar1, Gursharan Singh2, John Biku Joseph3, S Swaminathan4, L Venkatakrishnan5
1PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
2 HOD, Department of Liver Transplant Surgery, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
3 Consultant, Department of Liver Transplant Surgery, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
4 Consultant, Department of Liver Transplant Surgery, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
5 HOD, Department of Gasteroenterology, PSG Institute of Medical Sciences and Research, Coimbatore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prashanth Ashok Kumar, No. 20 A/10, Gopalakrishnan Street, Indira Devi Apartments, T. Nagar, Chennai-600017, Tamil Nadu, India.
E-mail: wizardakp@ymail.com
Pancreatic Tuberculosis is an uncommon form of extra pulmonary tuberculosis that resembles malignancy of pancreas and serve as a diagnostic challenge for physicians. Conservative management with Anti Tuberculosis Therapy (ATT) will suffice for pancreatic tuberculosis whereas a malignancy may require major surgeries which may lead to significant morbidity. Here, we discuss the case of a female patient who presented with abdominal pain and vomiting and is a known case of chronic calcific pancreatitis. Radiological findings were that of malignancy of the pancreas. Enteroscopy showed pus flowing out from the duodenum. Endoscopic Ultrasound (EUS) guided Fine Needle Aspiration Cytology (FNAC) of the pancreas revealed acid fast bacilli. The patient was treated successfully with ATT. Timely diagnosis of this rare form of extra pulmonary tuberculosis can thus help avoid unwanted resections done for presumed malignancy, for which a high index of suspicion is needed.
Anti tuberculosis therapy, Endoscopic ultrasound, Pancreas
Case Report
A 57-year-old female patient presented with complaints of abdominal pain and persistent vomiting for one month. The abdominal pain was predominantly in the epigastrium, non-radiating and associated with post prandial vomiting. The pain was relieved after the bout of vomiting. The patient had occasional febrile episodes and loss of appetite. The patient was a known case Chronic Calcific Pancreatitis and Diabetes Mellitus with both exocrine and endocrine deficiency. She was on pancreatic supplements and human insulin for the past 5 years. On examination, mild epigastric tenderness was present.
Blood picture showed normochromic normocytic cells. Prothrombin Time (PT), Liver Function Tests (LFT), Thyroid Function Tests (TFT), serum calcium and Parathormone levels were normal. Serum amylase and lipase were within normal range. Cancer Antigen 19-9 (CA 19-19) was not elevated. Random Blood Sugar and Glycated Haemoglobin (HbA1c) were high. Urine showed glycosuria but urinary ketones were negative. Blood and Urine cultures were sterile.
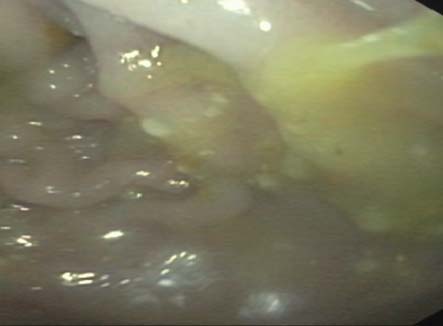
Chest X-Ray was normal. Ultrasound abdomen showed chronic calcific pancreatitis with dilated Main Pancreatic Duct (MPD) and tiny intraductal calculi. Common Bile Duct (CBD) was dilated with dilated Inta Hepatic Biliary Radicles. Upper GI endoscopy showed reflux esophagitis with bile reflux. CECT of abdomen showed calcifications in pancreatic head, body and tail with atrophic parenchyma, dilated MPD and multiple intraductal calculi [Table/Fig-1]. A mass was suspected to be present inferiomedial to the head of the pancreas. Intestinal obstruction was confirmed as Barium meal and follow through showed narrowing in the second part of duodenum. Endoscopy showed pus oozing out from the second part of the duodenum [Table/Fig-2]. Biopsy from the periampullary region of the duodenum showed that there was chronic nonspecific duodenitis with no evidence of invasive malignancy. EUS guided FNAC was done and revealed that the head of pancreas had features of chronic pancreatitis with a few acid fast bacilli. This enabled to arrive at the diagnosis of Tuberculosis of the pancreas.
CT whole abdomen showing calcification of head, body and tail of pancreas as shown by arrow.

Endoscopy showing pus oozing out of the duodenum.
She was started on ATT and Naso Jejeunal (NJ) feeds. She was given Streptomycin, Ethambutol, Isoniazid, Pyrizinamide and Rifampicin in compliance with standardized treatment regimes. She tolerated the treatment well. Repeat LFTs were done and were normal. Her condition progressively improved and she was started on oral feeds. Once she became stable, she was advised to continue Diabetic NJ and oral feeds and was asked to be on regular follow up.
Discussion
Tuberculosis is very prevalent in the developing areas of Asia and Africa, especially in India [1]. Abdominal tuberculosis is the most common extra pulmonary manifestation of the disease [1]. Pancreatic tuberculosis was first described by Auerbach in 1944 [2]. A study conducted by Nagar et al showed that among patients with abdominal tuberculosis in India, 8.3% had pancreatic involvement [3]. Pancreatic tuberculosis is a rare entity. As such, there are no studies to show its incidence, but it is uncommon even in the developing world where Tuberculosis is rampant [4].
Pancreatic tuberculosis most commonly involves the head and uncinate process of the pancreas [5]. It presents as vague and non-specific symptoms, with apparently normal examination findings [4]. Most common presenting symptoms include abdominal pain, jaundice, vomiting, anorexia and weight loss [6]. There may be palpable liver, gallbladder or abdominal mass [6]. Pancreatic tuberculosis may also present with peri-pancreatic lymphadenitis [1]. The disease is an enigma for doctors as it mimics other dis-orders of the pancreas, most importantly Pancreatic Malignancy. Abdominal lymphadenitis can also present similarly and mimic it [1].
Endoscopic Ultrasound (EUS), Fine Needle Aspiration Cytology (FNAC), Contrast Enhanced CT (CECT) and Laporotomy are the modalities used in the diagnosis. It has conspicuous radiological findings which resembles malignancy of the pancreas, due to which many cases have only been diagnosed on histopathological analysis of the pancreatic specimen after resection [5]. CA-19-19 alone is not a reliable marker of Pancreatic Carcinoma and cannot be used to differentiate it from tuberculosis [7,8]. The condition has no specific mass lesion features and even evidence of vascular invasion does not distinguish a malignancy from pancreatic tuberculosis [5]. Thus cytological analysis becomes inevitable for the diagnosis of pancreatic tuberculosis [9].
The following [Table/Fig-3] compares recently published indexed cases of pancreatic tuberculosis [9–17].
Indexed cases of pancreatic tuberculosis and their important features [9–17].
| Case | Age/Sex | Presentation | Investigation and findings | Diagnosis/Treatment/Outcome |
|---|
| Yamada et al., [10] | 57/M | Weight loss | CT- Pancreatic head mass with CBD stenosisEUS-FNAC- Granulomas with caseous necrosisQuantiferon gold assay positive | Pancreatic tuberculosis/ATT/Treated successfully |
| Choudhary et al., [11] | 20/F | Weight loss | CT- Mass probably from head of pancreasEUS- Mass near duodenal bulb compressing CBD. Pancreas and pancreatic duct normalFNAC- Granulomas with caseous necrosis. Acid fast bacilli visualised. | Tubercular lymphadenopathy/ATT/Treated successfully |
| Waintraub et al., [12] | 31/M | Fever, epigastric pain | MRI- Periportal lymphadenopathy indenting pancreatic head and uncinate process and compressing CBDCA 19 19, CA 125 negativeEUS- irregular, hypoechoic mass with poorly defined borders in the pancreatic head. Anechoic lesion in the pancreatic tail, suggestive of a cyst or pseudocyst.FNAC- Granulomas with caseous necrosis and Acid fast bacilli in head mass but not in cyst | Pancreatic tuberculosis/ATT/Treated successfully |
| Rana SS [13] | 42/F | Abdominal pain, weight loss | CECT- Pancreatic head mass with enhancing noduleEUS- Mass in head of pancreas, Subcarinal lympadenopathyFNAC- noncaseating necrosis and epithelioid granulomas in both pancreas and lymph node | Pancreatic tuberculosis/ATT/Treated successfully |
| YaminiCitra et al., [14] | 22/M | Abdominal pain, weight loss | CECT- Pancreatic head mass, peripancreatic and periportal lymphadenopathyEUS- Mass in head of pancreas with multiple peripancreatic nodesFNAC- noncaseating necrosis with langhans giant cell in pancreas, mesocolic tissue and lymph node. | Pancreatic tuberculosis/ATT/Treated successfully |
| Yadav AK [15] | 24/F | Abdominal pain, Jaundice, weight loss | Volume Perfusion Computed Tomography (VPCT) - Hypodense mass lesion in pancreatic head and uncinate process abutting the superior mesenteric vein. Perfusion parameters reduced compared to normal parts of pancreas.On-table frozen section- multiple necrotizing epitheloid cell granulomas with lymphocytic infiltration and destruction of pancreatic acini. | Pancreatic tuberculosis/Roun-en-Y hepaticojejunostomy and ATT/Treated successfully |
| Yadav AK [15] | 35/M | Abdominal pain, anorexia, weight loss | CECT - Multiple hypodense lesions encasing the celiac axis and its branches in the pancreatic body region.VPCT- Perfusion parameters of the pancreatic lesions significantly reduced compared to the normal pancreas.FNAC- necrotizing epitheloid cell granulomas with lymphocytic infiltration. | Pancreatic tuberculosis/ATT/Treated successfully |
| Chavadi et al., [16] | 39/M | Epigastric pain, fever | CT- Cystic lesion in the pancreas. Splenic artery was noted within the lesion. Multiple peripancreatic and retroperitoneal lymph nodes.CT guided aspiration- microscopy of pus showed AFB | Pancreatic tuberculosis/ATT/Treated successfully |
| George SZ et al., [9] | 60/M | Epigastric pain, weight loss | CECT- Pancreatic head mass encasing portal veinEUS- Necrotic pancreatic head massFNAC- multiple granulomas, epitheloid cells and occasional multinucleated giant cells with acid fast bacilli.Mantoux Positive | Pancreatic tuberculosis/ATT/Treated successfully |
| Ebrahimian R et al., [17] | 52/M | Epigastric pain, weight loss | CT- Pancreatic head massIntra op frozen section- Granuloma seen | Pancreatic tuberculosis/ATT/Treated successfully |
The management of pancreatic tuberculosis is mainly conservative with Anti Tuberculosis Therapy (ATT) [7,8]. Tuberculosis of the pancreas can be managed conservatively, but a malignancy usually needs to be resected. Thus the proper diagnosis of Pancreatic tuberculosis becomes imperative as it can avoid untoward surgical interventions like Whipples surgery which itself may contribute to significant morbidity and mortality [9]. Tubercular lymphadenitis which presents similar to pancreatic tuberculosis is also treated with ATT alone in majority of the cases [11]. Pancreatic tuberculosis patients having obstructive symptoms like biliary tract obstruction may require surgical intervention [6]. However, invariably most cases of pancreatic tuberculosis are diagnosed peri operatively on the table [1,6]. Thus, a high index of suspicion is needed if it has to be diagnosed early. EUS guided FNAC seems to be the preferred investigation of choice for detecting pancreatic tuberculosis [7]. Thus, it should be noted that pancreatic tuberculosis should be ruled out by FNAC in case of a vague mass or inflammation of the pancreas, especially in endemic areas.
Conclusion
Pancreatic tuberculosis is an unusual presentation of extra pulmonary tuberculosis that can be treated with ATT and has an excellent prognosis. EUS guided biopsy is the investigation of choice to detect it. It is important to diagnose it promptly so as to avoid unwanted surgical procedures. A high index of suspicion is needed, especially in tuberculosis endemic areas for its early diagnosis.
[1]. Shabnam S, Mohammad BM, Mohammad TS, Amir HMA, Pancreatic Tuberculosis: An Overview. JOPJ Pancreas (Online) 2015 16(3):232-38. [Google Scholar]
[2]. Auerbach O, Acute Generalized Miliary TuberculosisAm J Pathol 1944 20:121-36. [Google Scholar]
[3]. Nagar AM, Raut AA, Morani AC, Sanghvi DA, Desai CS, Thapar VB, Pancreatic tuberculosis: a clinical and imaging review of 32 casesJ Comput Assist Tomogr 2009 33:136-41. [Google Scholar]
[4]. Pramesh CS, Heroor AA, Gupta SG, Krishnamurthy S, Shukla PJ, Jagannath P, Pancreatic tuberculosis: an elusive diagnosisHPB (Oxford) 2003 5(1):43-45. [Google Scholar]
[5]. Surinder SR, Vishal S, Sathosh S, Ravi S, Bhagwant RM, Deepak KB, Vascular invasion does not discriminate between pancreatic tuberculosis and pancreatic malignancy: a case seriesAnn Gastroenterol 2014 27(4):395-98. [Google Scholar]
[6]. Sundeep SS, Sukanta R, Sujoy P, Manu K, Deep NS, Peush S, Hepatobiliary and pancreatic tuberculosis: A two decade experienceBMC Surgery 2007 7:10 [Google Scholar]
[7]. Nikhil S, Sayantan R, Partha P, Avishek S, Arunansu T, Fine needle aspiration diagnosis of isolated pancreatic tuberculosis: A case reportWorld J Clin Cases 2013 1(5):181-86. [Google Scholar]
[8]. Jasna T, Ljubomir M, Mladen P, Svetlana S, Borislava N, Biljana K, Evaluation of imaging techniques and CA 19-9 in differential diagnosis of carcinoma and other focal lesions of pancreasArch Oncol 2004 12(2):104-08. [Google Scholar]
[9]. George SZ, Rajany A, Sandesh K, Thazhath MR, Isolated pancreatic tuberculosis masquerading as pancreatic cancerGastroenterol Rep 2014 2(2):154-57. [Google Scholar]
[10]. Yamada R, Inoue H, Yoshizawa N, Kitade T, Tano S, Sakuno T, Peripancreatic Tuberculous Lymphadenitis with Biliary Obstruction Diagnosed by Endoscopic Ultrasound-guided Fine-needle Aspiration BiopsyIntern Med 2016 55(8):919-23. [Google Scholar]
[11]. Choudhary NS, Guleria M, Puri R, Sud R, Tubercular lymph nodal mass mimicking pancreatic malignancy with extrahepatic biliary obstruction in a young womanEndoscopy 2015 47(Suppl 1):UCTN:E53-54. [Google Scholar]
[12]. Waintraub DJ, D’Souza LS, Madrigal E, Harshan M, Ascunce GI, A Rare Case of Isolated Pancreatic TuberculosisACG Case Rep J 2016 3(4):e91 [Google Scholar]
[13]. Rana SS, Gupta R, Ranjan R, Srinivasan R, Bhasin DK, Pancreatic tuberculosis mimicking cystic tumor of pancreasJ Dig Endosc 2016 7:30-32. [Google Scholar]
[14]. Yamini Chitra V, Paramesh KN, An unusual cause of pancreatic head mass: Primary pancreatic tuberculosisEdorium J Gastroenterol 2015 2:7-12. [Google Scholar]
[15]. Yadav AK, Nadarajah J, Kandasamy D, Sharma R, Gamanagatti S, Garg PK, Volume perfusion computed tomography as an aid to diagnosis of pancreatic tuberculosisTropical Gastroenterology 2014 35(4):264-66. [Google Scholar]
[16]. Chavadi CV, Kory S, Rao P, Mahale A, Pancreatic tuberculous abscess mimicking as cystic neoplasm: A rare initial manifestation of AIDS-defining illnessJ HIV Hum Reprod 2015 3:20-22. [Google Scholar]
[17]. Ebrahimian R, Tasa D, A patient with isolated pancreatic tuberculosis: Case reportTehran University Medical Journal 2015 73(6):462-67. [Google Scholar]