Cystic Pheochromocytoma Presenting as Adrenal Cyst
Mohammed Shafi Abdulsalam1, Vijaya Ganapathy2, Priyanka Satish3, Raghunath Keddy Janakiraman4, Shivshankar Singh5
1 Postgraduate Student, Department of General Medicine, Apollo Main Hospital, Chennai, Tamilnadu, India.
2 Senior Consultant Endocrinologist, Apollo Main Hospital, Chennai, Tamilnadu, India.
3 Student, Stanley Medical College, Chennai, Tamilnadu, India.
4 Senior Consultant General Surgeon, Apollo Main Hospital, Chennai, Tamilnadu, India.
5 Senior Medical Specialist, GB Pant Hospital, Port Blair, Andaman and Nicobar Islands, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vijaya Ganapathy, Senior Consultant Endocrinologist, Greams Road, Apollo Main Hospital, Chennai-600006, Tamilnadu, India.
E-mail: drvijaya_endo@yahoo.com
Pheochromocytomas are usually solid tumours. But it can present as cystic lesions in the adrenal gland. Cystic lesions in adrenal gland with hypertension needs attention to rule out pheochromocytoma. If ignored, it may lead to hypertensive emergency, multisystem crisis and death. Early diagnosis with biochemistry, Computed Tomography (CT) or Magnetic Resonance Imaging (MRI) of abdomen, proper functional imaging like Meta Iodo Benzyl Guanidine (MIBG) scan is essential. Proper preoperative preparation is important to prevent hypertensive crisis during and after surgery. We are reporting a case of cystic pheochromocytoma in a young male.
Endocrine emergency, Multisystem crisis, Pulmonary edema
Case Report
A 43 years old male, not a diabetic or hypertensive presented with history of intermittent colicky abdominal pain lasting 5-10 minutes with 1-2 episodes/month for the past one and half years . During those episodes, he was found to have high blood pressure. For the last two months, these episodes of abdominal pain were associated with sweating, palpitation and syncope. He denied any history of breathing difficulty, loss of weight, loss of appetite or back pain. He was not a smoker or alcoholic. There was no history of any long term medications intake. He had one episode of pulmonary edema and high blood pressure prior to admission in our hospital. He was treated for pulmonary edema and high blood pressure. He was referred here for further workup.
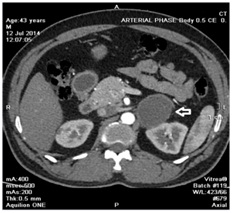
On clinical examination, pulse rate was 88/min, regular and blood pressure was 150/90mm Hg. Electrocardiogram showed sinus rhythm with heart rate of 80/min. His blood counts, liver function tests and renal function tests were within normal range. Transthoracic echocardiogram showed mild left ventricular hypertrophy with Left Ventricular Ejection Fraction (LVEF) of 69%. Serum amylase and lipase were within normal range. HbA1C was 6.5%. TSH was 9.4mIU/L, 24 hrs urine metanephrine and normetanephrine were significantly elevated [Table/Fig-1]. The 320 slice CT of abdomen showed 5cm x 4.3cm x 4.3cm cyst in the left adrenal gland with fine septations inside and cholelithiasis [Table/Fig-2]. In view of possibility of pheochromocytoma, MIBG scan was done, which showed faint MIBG concentration in the left adrenal cyst. MRI of abdomen showed left adrenal mass (4.3cm x 4.4cm x 4.8cm), acute calculous cholecystitis and probable early pancreatitis.
| Variables | Values |
|---|
| Calcium | 8.8 mg/dl |
| Phosphorous | 2.5 mg/dl |
| Fasting blood sugar | 147 mg/dl |
| Postprandial blood sugar | 208 mg/dl |
| HbA1C | 6.5% |
| Thyroid stimulating hormone (TSH) | 9.4, 9.1, 7.7 m IU/L |
| Parathormone (PTH) | 19.8 pg/ml |
| 24 hrs urine metanephrine(<350 μ gm/24hrs *) |
| Before surgery | 1939 μ gm/24hrs |
| After 1month | 98 μ gm/24hrs |
| After 10 month | 88 μ gm/24hrs |
| 24 hrs urine normetanephrine(<600 μ gm/24hrs *) |
| Before surgery | 1248 μ gm/24hrs |
| After 1month | 385 μ gm/24hrs |
| After 10 month | 426 μ gm/24hrs |
* Normal reference range
CT scan image showing adrenal cyst.
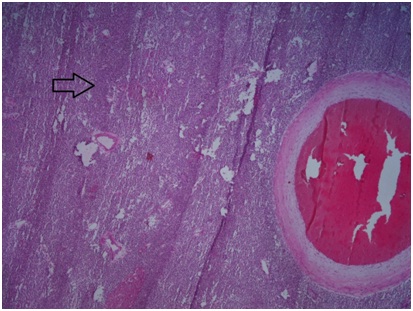
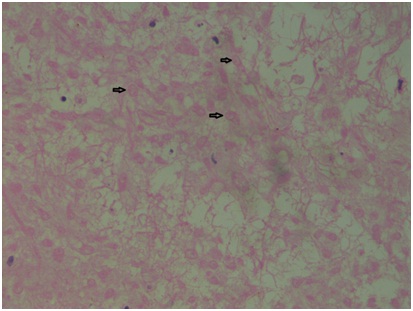
After controlling blood pressure with alpha blocker and following volume expansion, laparoscopic left adrenelectomy and cholecystectomy were done. Post operative period was uneventful. Post operatively the patient was kept under observation in surgical intensive care unit. Excised adrenal cystic tumour measuring 5.5cm x 5.5cm x 2cm showed smooth external surface attached with fibroadipose tissue. Cut surface appeared capsulated and tan to yellowish brown in colour. Histopathology showed completely infarcted left adrenal tumour [Table/Fig-3]; within the necrotic foci some ghost outlines of cells were seen [Table/Fig-4]. Multiple sections from completely processed tissue showed similar features. After 10 months of follow-up, he was doing well and his 24 hours urine metanephrine and normetanephrine were within normal range.
Completely infracted left adrenal tumor with extensive necrosis.
Within the necrotic foci some ghost outlines of cells were seen.
Discussion
Pheochromocytoma is a tumor arising from adrenomedullary chromaffin cells that commonly produce one or more catecholamines: Epinephrine, Norepinephrine and Dopamine [1]. Pheochromocytomas can present as cystic lesions, which may mislead the diagnosis. Pheochromocytoma should be considered in patients presenting with nonspecific symptoms and an incidental cystic adrenal mass, even in the absence of hypertension [2]. A typical solid pheochromocytoma can be easily diagnosed with available diagnostic methods. However, it is difficult to diagnose cystic pheochromocytoma since it structurally resembles a benign adrenal cyst. Structural imaging may be inconclusive. Functional imaging like MIBG scan is essential to prove the presence of sympatho-adrenal tissue [3].
Our patient presented with abdominal pain associated with high blood pressure and had a cystic lesion in the left adrenal gland. Biochemical analysis showed increased 24 hour urinary Metanephrine and Normetanephrine. MIBG scan showed faint uptake in the cystic lesion. High index of suspicion must be there to find out pheochromocytoma. Sometimes biochemical analysis may not be helpful, since cystic pheochromocytoma can show normal urinary metanephrine and normetanephrine levels.
Andreoni et al., studied 31 patients with pheochromocytoma. Six patients had cystic pheochromocytoma and three of them were asymptomatic [4]. Formation of cystic pheochromocytoma might be due to intralesional haemorrhage, necrosis and later cyst formation. Patients with cystic pheochromocytoma are more likely to be asymptomatic and tend to have a negative biochemical evaluation. Symptomatic patients tend to have abdominal pain [2,4]. Our patient had 5cm cystic lesion, where as cystic pheochromocytoma measuring more than 15cm has been reported in literature [5]. Cystic pheochromocytomas are rare and usually present as unilateral cystic lesion. It can be bilateral also [6].
Our patient was found to have completely infarcted adrenal tumour on histopathology. Unless surgically removed, pheoc-hromocytomas can lead to hypertensive crisis and several cardiovascular complications. Malignant cystic pheochromocytoma with normal biochemistry and metastasis to liver has been reported in literature [7]. Our patient had elevated urine metanephrine and normetanephrine with no metastasis. He had abdominal pain, pulmonary edema, leucocytosis, mildly elevated creatine phosphokinase, serum amylase and lipase. He also had cholecystitis and early pancreatitis on imaging. Early diagnosis was made and the patient was taken up for surgery after adequate preparation. If the patient was not diagnosed on time or a delay in surgery, there was a greater likelihood of going into multisystem crisis and death.
Pheochromocytoma multisystem crisis is a life-threatening condition. Spontaneous rupture is another life threatening condition. Spontaneous rupture of cystic pheochromocytoma leading to adrenergic crisis has been reported [8]. Gundgurthi et al., reviewed 27 articles in which more than one third of the patients died due to multisystem crisis [9]. Early diagnosis and treatment is essential in that situation, since mortality is high. Our patient was doing well at 10 months of follow-up; his urinary metanephrine and normetanephrine were within normal range.
Conclusion
In any patient presenting with abdominal pain, hypertension and adrenal cystic lesion, pheochromocytoma should be suspected. Careful history and clinical examination will help to diagnose pheochromocytoma. Urine metanephrine and normetanephrine assay must be done prior to imaging. CT or MRI will provide information about the structural lesions. Functional imaging like MIBG scan will be clearly able to define the aetiology as pheochromocytoma. Early surgical intervention, following blood pressure control with alpha blocker and adequate volume expansion is essential in saving the patient. Periodical monitoring of these patients is very important since they may develop other manifestations of multiple endocrine neoplasia or new pheochromocytoma in the other adrenal gland later in their life.
* Normal reference range
[1]. Lloyd RV, Tischler AS, Kimura N, Adrenal tumours:Introduction. In: DeLellis RA, Lloyd RV, Heitz PU, et al. editorsPathology and Genetics of Tumours of Endocrine Organs; IARC WHO Classification of Tumours 2004 Lyon, FranceIARC Press:137-38. [Google Scholar]
[2]. Erem C, Kocak M, OnderErsoz H, Ersoz S, Yucel Y, Epinephrine-secreting cystic pheochromocytoma presenting with an incidental adrenal mass: a case report and a review of the literatureEndocrine 2005 28:225-30. [Google Scholar]
[3]. Wang Yuh-Feng, Shiou-Chi Cherng, Tsu-Kang Jen, Wen-Sheng Huang, Cystic pheochromocytoma-an unusual presentation of the adrenal massAnn Nuli Med Sci 2000 13:121-24. [Google Scholar]
[4]. Andreoni C, Krebs RK, Bruna PC, Goldman SM, Kater CE, Alves MT, Cystic pheochromocytoma is distinctive subgroup with special clinical, imaging and histological features that might mislead the diagnosisBJU Int 2008 101:345-50. [Google Scholar]
[5]. Pan Z, Repertinger S, Deng C, Sharma P, A giant cystic pheochromocytoma of the adrenal glandEndocr Pathol 2008 19(2):133-38. [Google Scholar]
[6]. Gayathri S, Baruah B P, Kumar S, Garg P, Bilateral cystic pheochromocytoma: An incidental finding and a rare case entityIndian J Cancer 2011 48:260-62. [Google Scholar]
[7]. Soufi M, Lahlou MK, Benamr S, Massrouri R, Mdaghri J, Essadel A, Giant malignant cystic pheochromocytoma: A case reportIndian J Surg 2012 74:504-06. [Google Scholar]
[8]. Miura K, Kanno T, Nakamae K, Kubota M, Nishiyama R, Okada T, A case of adrenergic crisis caused by spontaneous rupture of cystic pheochromocytomaHinyokika Kiyo 2015 61(11):427-32. [Google Scholar]
[9]. Gundgurthi A, Gupta S, Garg MK, Ganguly P, Bhardwaj R, Unsuspected pheochromocytoma multisystem crisis: a fatal outcome in a young male patientJ Assoc of Physicians India 2012 60:53-60. [Google Scholar]