Hematopoietic Stem Cell Transplantation (HSCT) is an emerging management modality of various haematopoietic malignant and severe immunologic disorders, haematological disorders [1]. India has come a long way in the field of HSCT. Indications of HSCT are malignant, non-malignant, storage and metabolic disorders. HSCT recipients have been limited to, studies including only small number of patients and such studies are rare in India as this facility is limited to very few hospitals [2].
The main component of bone marrow, which ensures hematopoietic regeneration, is the pluripotent stem cell - which has been characterized by immune-phenotyping. Depending upon the donor, the transplantation is called allogeneic, autologous or from an identical twin called syngenic [3].
For the procedure, the recipient and donors undergoes matching for the blood group, HLA, complete blood counts and microbiological examinations, to rule out any active infection. Complete biochemical investigations for ruling out any organ dysfunction is also done. After matching, recipient requires immunosuppression to reduce Graft versus Host Disease (GvHD). Mobilization consists of the use of growth factors or chemotherapy agents for collecting enough stem cells from donor which can be from the marrow, peripheral blood, umbilical cord and amniotic fluid. These harvested stem cells are then cryopreserved and then infused after thawing. In vitro manipulation is done primarily to reduce the relapse and GvHD. This is done by either treating the marrow cells by monoclonal antibodies reactive to T cells or leukaemia cells using complement or incubated with drugs as mafosfamide [3–5].
The conditioning is primarily aimed for eradication of the recipient clone (normal and malignant cells), to create space for the recipient stem cells and to cause immunosuppression [6].
Radiological description of the pulmonary complications reflects the immunogenic status of the patients and occurs in three periods [7–11]:
1) The neutropenic period (up to 3 weeks after the transplant) is characterized by fungal infections, notably angioinvasive aspergillosis, alveolar haemorrhage, pulmonary oedema and drug reactions;
3) Late period (>100 days post-transplant) is characterized by Bronchiolitis Obliterans (BO), Bronchiolitis Obliterans with Organizing Pneumonia (BOOP) and Chronic GvHD.
Today, continuous spiral acquisition technique is used which has replaced the older ‘incremental’ acquisition technique where 1-mm slices were acquired with an image interval of 10 mm [12].
This study primarily focuses on the radiological features of the pulmonary complication HSCT, its use for early diagnosis and treatment to reduce mortality and morbidity in the recipients.
Materials and Methods
This was a prospective observational study, conducted after clearance from the Ethical Committee, from October 2013 to March 2015. It included 52 patients who had undergone HSCT during this period in the hospital. All patients underwent complete clinical examination and laboratory investigations as Complete Blood Count (CBC), serum biochemistry, USG abdomen, chest radiography, baseline HRCT on Philips Brilliance multiphasic 16 slice HRCT chest, post transplant HRCT when suspected clinical abnormalities and either BAL (Broncho-Alveolar Lavage) and sputum examination. Patients who did not achieve engraftment and patients with evidence of pulmonary embolism were excluded from the study.
The patients were observed during the study duration on the basis of suspicion of the clinical symptoms as fever, cough and weight loss. These patients were divided into three groups on the basis of the presentation of symptoms following the HSCT: that is <30 days, <100 days and >100 days of the post HSCT period and the pattern of the abnormalities were studied [7–11].
Thorough clinical examination was done to screen for pre-transplant chemotherapy. The follow-up for any post-transplant complications was done using a 16 slice Philips CT scan. The recommended position for this study was prone; however, supine position was kept reserved to critically ill patients. One mm thick slices of helical scans were acquired from the thoracic inlet to the diaphragm with a pitch of 1.0 and image reconstruction at 0.5mm intervals with high frequency reconstruction algorithm for lung and soft tissue algorithm [12].
The radiological findings were reported by two junior radiologists of 4 years of experience and reviewed by a senior radiologist of 26 years of experience. The senior radiologist was kept unaware of the clinical background of the patients. The results were correlated with the clinical, laboratory and radiological outcomes.
Study protocol HRCT acquisition was taken from the thoracic inlet till the diaphragm. The study is done as per values and parameter [Table/Fig-1] for Philips Brilliance 16 slice CT scanner [13].
The study protocol parameters.
| Parameter | Values |
|---|
| Length | 300mm |
| Direction | Out |
| Increment and thickness | 0.5mm and 1mm |
| *kV, † mAs/Slice | 120,200 |
| Resolution | High |
| Collimation | 16 x 0.75 |
| Pitch | 0.938 |
| Rotation time | 0.5 sec |
| §FOV | 300mm |
| Window | C-400, W 1200 |
| Centre and Matrix | X 0, Y 0 and 768 |
* kV-kilovolts, † mAs/Slice- milli amperes seconds, §FOV-Field Of View
Statistical Analysis
With the help of Chi-square method different parameters studied were age group, patients chief complaints, sputum analysis and BAL correlation, ultrasound and routine investigation findings, personal history and biochemical parameters with the radiological findings.
Results
Out of the 52 patients, 35 were male and 17 were female with age varies from 1 to 72 years. There were total 9 children and 43 adults. The number of deaths noticed in the study was 2 among children and 3 among the adults (2 females and 3 males).
A total of 16 cases had normal HRCT chest, followed by non-specific findings as fibrosis, consolidation with sterile bronchial fluid, bronchiectatic changes, chronic GvHD, tuberculosis, bacterial pneumonia and viral pneumonia. Twelve cases had consolidation with sterile bronchial fluid, fibrosis, bronchiectatic changes, chronic GvHD, tuberculosis, bacterial pneumonia and viral pneumonia. Most of these findings were not observed on the conventional radiograph.
The common findings in the neutropenic patients were bilateral consolidations, mass like lesion and ground glass opacities in one patients turned fungal pneumonia later, ill defined opacities, ground glass opacities at bilateral lower lobes turned to be CMV positive pneumonia later, bilateral patchy consolidation and ground glass opacities later diagnosed as idiopathic pneumonia syndrome and patchy consolidation and ground glass opacities in one case later detected positive for Gram-negative bacilli. These cases were excluded later due to non-engraftment.
Cough was the most common presenting symptom in this study followed by fever and weight loss [Table/Fig-2]. Most of the patients had positive radiological findings after 100 days of HSCT however this is not statistically significant (p-values of all are >0.05).
Chief complaints and distribution of post-transplant HRCT (Radiological Findings).
| Symptoms | Post transplant HRCT (Radiological Findings) | Total | Chi-square value | p-value |
|---|
| PT1 | PT2 | PT3 | PT4 | PT5 | PT6 |
|---|
| Fever (number of patients) | Yes | 3 | 8 | 1 | 0 | 4 | 4 | 20 | 8.95 | 0.111 |
| No | 3 | 4 | 4 | 4 | 12 | 5 | 32 |
| Total | 6 | 12 | 5 | 4 | 16 | 9 | 52 |
| Weight (number of patients) loss | Yes | 2 | 7 | 2 | 2 | 2 | 2 | 17 | 7.67 | 0.176 |
| No | 4 | 5 | 3 | 2 | 14 | 7 | 35 |
| Total | 6 | 12 | 5 | 4 | 16 | 9 | 52 |
| Cough (number of patients) | Yes | 5 | 10 | 4 | 4 | 15 | 5 | 43 | 6.86 | 0.231 |
| No | 1 | 2 | 1 | 0 | 1 | 4 | 9 |
| Total | 6 | 12 | 5 | 4 | 16 | 9 | 52 |
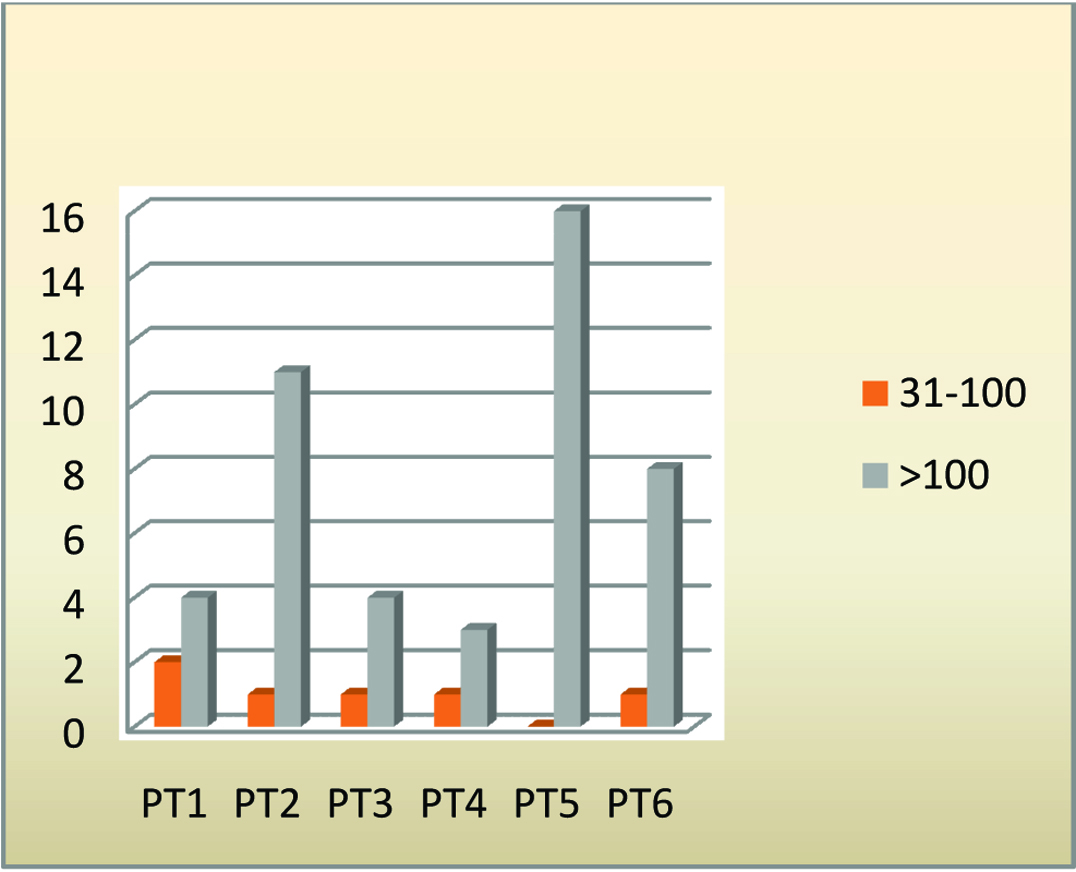
| Duration of Radiological features from transplant (days) | 31-100 | 2 | 1 | 1 | 1 | 0 | 1 | 6 | 6.06 | 0.3 |
| >100 | 4 | 11 | 4 | 3 | 16 | 8 | 46 |
| Total | 6 | 12 | 5 | 4 | 16 | 9 | 52 |
PT 1- stands for fibrotic changes
PT 2- stands for consolidation.
PT 3- stands for cavities
PT 4- stands for bronchiectatic changes and tree in bud appearence
PT 5- stands for normal.
PT 6- stands for ground glass opacities and ill defined opacities.
Most of the pulmonary complications were found at >100 days followed by <100 and <30 days respectively [Table/Fig-3]. The patients presenting with early symptoms (<30 days) were associated with prolonged neutropenia and later excluded due to non-engraftment. The patients who died in the study (in 5 patients) had consolidation as the most common lung finding (in 4 patients). Most common cause of death among the patients in the study was due to sepsis (in 3 patients) followed by low counts of all cell lines except one patient who died due to gastrointestinal tract symptoms with Venous Occlusive Disease (VOD).
Duration of radiological findings with transplant (days).
The [Table/Fig-4] demonstrates that the sputum or bronchial fluid was frequently sterile (in 32 patients) followed by fungal (in 10 patients), tubercular (in 5 patients), bacterial (in 3 patients) and of viral origin (in 2 patients). The correlation for this finding was statistically significant (p-value=0.029). In the final diagnosis the most common findings were of group1 of bronchial fluid analysis associated with group 5 of radiological findings. The final diagnosis was statistically significant with these findings (p-value 0.002).
The statistical significance between the bronchial fluid analysis and the radiological findings. The sputum fluid/ Bronchial fluid analysis are coded in five groups (GR1-5).
| Post transplant HRCT (Radiological Findings) | Total | Chi-square value | p-value |
|---|
| PT1 | PT2 | PT3 | PT4 | PT5 | PT6 |
|---|
| Sputum/bronchial fluid analysis | GR1 | 4 | 7 | 4 | 4 | 15 | 9 | 43 | 27.01 | 0.029 |
| GR2 | 2 | 0 | 1 | 0 | 0 | 0 | 3 |
| GR3 | 0 | 3 | 0 | 0 | 1 | 0 | 4 |
| GR4 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| Total | 6 | 12 | 5 | 4 | 16 | 9 | 52 |
| Final diagnosis | GR1 | 2 | 1 | 3 | 3 | 15 | 8 | 32 | 42.8 | 0.002 |
| GR2 | 2 | 1 | 2 | 0 | 0 | 0 | 5 |
| GR3 | 0 | 2 | 0 | 0 | 1 | 0 | 3 |
| GR4 | 0 | 2 | 0 | 0 | 0 | 0 | 2 |
| GR5 | 2 | 6 | 0 | 1 | 0 | 1 | 10 |
| Total | 6 | 12 | 5 | 4 | 16 | 9 | 52 |
GR1-Group 1 for sterile and non specific.
GR2-Group 2 for tuberculosis.
GR3-Group 3 for bacterial origin.
GR4-Group 4 for viral markers positive.
GR5-Group 5 for fungal origin.
The [Table/Fig-5] describes the statistical analysis of personal history with the health status of the patients. There was no statistically significant correlation of healthy and dead patients with the history of smoking (p-value=0.282), alcohol consumption (p-value=0.282) or diet (p-value=0.158). The [Table/Fig-6] describes the statistical analysis between the biochemical examinations and the follow-up health status of the patients under study. There were deaths of 2 out of 5 patients with abnormal Liver Function Test (LFT) while 3 out of 47, among patients with normal LFT. The result was statistically significant (p-value= 0.015). In the study the normal ranges considered were:
Personal history with follow-up health status till date.
| Follow-up status till date | Total | Chi-square value | p-value |
|---|
| Healthy | Death |
|---|
| Smoking | Yes | 9 | 0 | 9 | 1.16 | 0.282 |
| No | 38 | 5 | 43 |
| Total | 47 | 5 | 52 |
| Alcohol | Yes | 9 | 0 | 9 | 1.16 | 0.282 |
| No | 38 | 5 | 43 |
| Total | 47 | 5 | 52 |
| Diet | Mixed and patients on total parental nutrition | 25 | 1 | 26 | 1.99 | 0.158 |
| Vegetarian | 22 | 4 | 26 |
| Total | 47 | 5 | 52 |
Biochemical analysis with health follow-up status till date.
| Follow-up status till date | Total | Chi-square value | p-value |
|---|
| Healthy | Death |
|---|
| Liver function test | Normal | 44 | 3 | 47 | 5.88 | 0.015 |
| Abnormal | 3 | 2 | 5 |
| Total | 47 | 5 | 52 |
| Renal function test | Normal | 47 | 4 | 51 | 9.58 | 0.002 |
| Abnormal | 0 | 1 | 1 |
| Total | 47 | 5 | 52 |
| Electrolytes | Normal | 47 | 3 | 50 | 19.55 | <0.001 |
| Abnormal | 0 | 2 | 2 |
| Total | 47 | 5 | 52 |
ALT - 7 to 55 units per litre (U/L)
AST - 8 to 48 (U/L)
ALP - 45 to 115 (U/L)
Albumin - 3.5 to 5.0 (g/dL)
Total protein - 6.3 to 7.9 (g/dL)
Bilirubin - 0.1 to 1.0 (mg/dL)
GGT - 9 to 48 (U/L)
LD - 122 to 222 (U/L)
In relation to Renal Function Test (RFT), there was death of only 1 patient with abnormal RFT while 4 out of 51 among patients with normal RFT (p-value= 0.002).
In this study there was death of all the 2 patients with abnormal serum electrolytes while 3 out of 50 patients with normal serum electrolytes (p-value< 0.001).
The [Table/Fig-7] describe the role of routine imaging work up in the HSCT patients. The 5 patients who died during the study, had normal chest radiograph but there were positive findings on HRCT chest (p-value=0.001). The patients had abnormal abdominal ultrasound (USG) scan however these abnormalities were incidental.
Results of the ultrasound abdomen and X ray chest and the follow-up findings.
| Follow-up status till date | Total | Chi-square value | p-value |
|---|
| Healthy | Death |
|---|
| Chest x ray Findings | Normal | 47 | 5 | 52 | Not calculated | Not calculated |
| Total | 47 | 5 | 52 |
| USG findings | Normal | 36 | 3 | 39 | 0.664 | 0.415 |
| Abnormal | 11 | 2 | 13 |
| Total | 47 | 5 | 52 |
The [Table/Fig-8] describes the group statistics with t-test for the healthy and dead patients with their vital parameters i.e., temperature (T-F), pulse (p/minute) and respiratory rate (R/R/minute). The patients who died later had a mean body temperature 99.940F with a standard deviation of 1.29 however this was not statistically significant (p-value=0.098). The patients who died later had a mean pulse of 94.80 before death with standard deviation of 12.93 which was statistically significant (p-value =0.029). Similarly, the respiratory rate of the patient who died later had a mean of 19.00 with a standard deviation of 3.67 however, this was not statistically significant (p-values=0.132).
Vitals and its relation with Health Status of patients.
| Group Statistics |
|---|
| Follow-up status till date | N | Mean | Std. Deviation | p-value |
|---|
| Temperature (F) | Healthy | 47 | 99.19 | 0.91 | 0.098 |
| Death | 5 | 99.94 | 1.29 |
| Pulse rate (per minute) | Healthy | 47 | 81.19 | 12.84 | 0.029 |
| Death | 5 | 94.80 | 12.93 |
| Respiratory rate (per minute) | Healthy | 47 | 16.85 | 2.92 | 0.132 |
| Death | 5 | 19.00 | 3.67 |
t-test
Discussion
The results of the study demonstrate that the HRCT chest is an important and very useful investigation in the case of HSCT transplant patients as it provides an early diagnosis and thus early treatment.
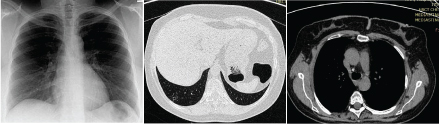
The present study states that most of the cases had normal HRCT chest, followed by non-specific finding as consolidation with sterile bronchial fluid, fibrosis, bronchiectatic changes, chronic GvHD, tuberculosis [Table/Fig-9a-c], bacterial pneumonia and viral pneumonia. Most of these findings were not observed on the conventional radiograph.
A 46-year-old female a known case of AML with chief complaints of cough. Radiographic findings 8 months after the transplant. This patient was found positive for acid fast bacilli. (a) Chest radiograph of this patient appearing normal. (b) Axial view of a patient of AML with tuberculosis showing small cavity with surrounding ground glass opacities in right lower lobe. (c) Axial view in mediastinal window showing calcified lymph node.
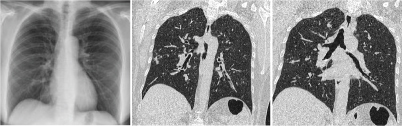
The analysis of the bronchial fluid and sputum examination was very helpful in establishing the diagnosis and were equally contributory for the radio-pathological correlation of the study. Most common findings among them were non-specific [Table/Fig-10a-c] and sterile fluid analysis followed by fungal, tubercular, bacterial and viral aetiology. These results helped to start the appropriate chemotherapeutic agent to control the complications and contributed in the early management of the complications.
A 19-year-old female known case of Fanconi’s anaemia presented with fever and weight loss after 8 months of transplant. Patient died later due to chronic graft rejection with abdominal complications. (a) Chest radiograph of the patients appears normal. (b) HRCT chest coronal view showing ground glass opacities are noted in both lungs with patchy consolidation in right upper lobe. (c) Coronal view of the patient showing few nodular lesions are noted in right upper lobe along with ground glass opacities in right middle lobe. Some scattered bronchiectatic lesions are noticed in left upper lobe and right lower lobe.
As per this study, the most common presenting symptoms was cough followed by fever and weight loss (wt loss). Most of these patients were observed with positive radiological findings after 100 days of HSCT [Table/Fig-11a,b]. Pulmonary complications are the most life threatening conditions that develop in HSCT recipients [14].
(a) Axial view showing air bronchograms at right lower lobe and collapse consolidation of the left lower lobe, the fixation screws are visible for the pathological fracture of the dorsal vertebra. (b) Bone window axial view of the patient showing multiple lytic areas in the sternum and ribs with fixation of the pathological fractures in dorsal vertebrae.
Similar findings have been described in other studies [15–20]. These findings were diagnosed and treated early in the study led to the survival rate of greater than 90 percent.
This study also proved that, the pulmonary complications of HSCT were unrelated statistically with the hobbies, personal habits like alcohol consumption or smoking and dietary habits.
The mortality appeared high in the patients with deranged liver and renal function tests; however, this was not proved in all patients who died during the study.
A study of Hatzimichael states that, the major causes of mortality were late recurrence of original malignant disease, chronic GvHD, late infections without GvHD, secondary malignancies, pulmonary and cardiac complications [5]. Up to 1/5th of long-term survivors have functional impairments for many years after HSCT. Late complications of the HSCT include treatment regimen toxicities, immune deficiency, autoimmune syndromes, and growth impairment in children, cognitive dysfunction, second malignancies, chronic GvHD and abnormalities with psycho-social adjustment. These late effects can deteriorate performance for the day to day activities, sense of personal well-being, and inter-personal and family relationships. As compared with above study, our study found that the mortality was only 5 among total 52 patients taken in the study. This is about 9.6% in the studied sample with survival of 91.4% of the patients still kept good health after HSCT. Similarly as the death of one patient was noticed after 3 years, it shows that, the risk of delayed mortality is even higher in the recipients.
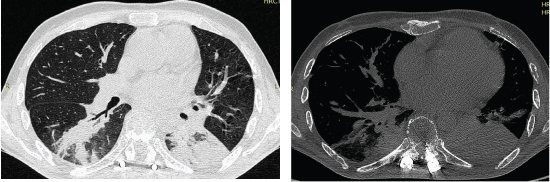
Another study of Coelho LOM et al., described that, there were about 60% patients who had consolidation, 50% centri-lobular nodules, 40% ground glass opacities [Table/Fig-12a-c], 20% large nodules, 10% pleural opacities and 10% had the tree in bud opacities [21]. As per their study the presence of large nodules and visualization of the halo sign was most suggestive of fungal infection. Other high-resolution CT patterns were not helpful in distinguishing among the various types of infection seen in bone marrow transplant recipients. Similar results have been published in few more studies [22–25]. As compared, our study states that, the positive findings were about 23% consolidation, 17% ground glass opacities, 11% fibrotic changes, 10% cavities and 8% had bronchiectatic changes. Over 1/3rd of the cases had normal HRCT chest. This study is stronger as we correlated the pathologies with the HRCT findings by pathological fluid analysis.
A 25-year-old male known case of Aplastic anaemia with chief complaints of fever and cough following 3 years of transplant. Patient was found positive for CMV infection in bronchial aspirate. (a) Radiograph chest appearing normal. (b) Axial section of the lung showing extensive ground glass opacities in bilateral lungs and few areas of patchy consolidation in right middle lobe, right lower lobe and left upper lobe. (c) Axial section of lungs with bilateral ground glass opacities and patchy consolidation in right lower lobe.

However, the differences among the studies with the present one could be explained on the basis of difference in the number of total patients, geographical population, environmental factors, socioeconomic status, statistical study group, objectives and manufacturer of CT.
Limitation
Few patients were excluded from the study due to non-engraftment but we had a significant scope for studying such patients for preventing future mortality of post-HSCT procedure. The patients selected were not uniformly divided based on the age groups, gender and diseases. Different geographical origin of the patients, inability in positioning the patients in pronation for HRCT was few of the other limitation. The radiation hazards associated could not be avoided.
Conclusion
The patients with HSCT always have a risk for various pulmonary complications; however the early use of HRCT chest helps in early diagnosis and treatment. The HRCT chest has been found normal on several occasions with positive history of pulmonary symptoms and in such cases the bronchial fluid analysis was complimentary for the management. Similarly, on various immunogenic conditions as GvHD and VOD the pathological fluid analysis was found normal with positive HRCT chest study, hence, the use of both the modalities was the most favourable approach in such cases. Similarly mortality was higher in patients with deranged counts or abnormal organ function tests, hence these should be considered in the management and follow-up of such cases.
* kV-kilovolts, † mAs/Slice- milli amperes seconds, §FOV-Field Of View
PT 1- stands for fibrotic changes
PT 2- stands for consolidation.
PT 3- stands for cavities
PT 4- stands for bronchiectatic changes and tree in bud appearence
PT 5- stands for normal.
PT 6- stands for ground glass opacities and ill defined opacities.
GR1-Group 1 for sterile and non specific.
GR2-Group 2 for tuberculosis.
GR3-Group 3 for bacterial origin.
GR4-Group 4 for viral markers positive.
GR5-Group 5 for fungal origin.
t-test