Hand eczema is one of the most common dermatological disorders, caused by various exogenous and endogenous factors. Many hand eczema cases have multifactorial aetiology, including allergic contact dermatitis. Therefore, identification and avoidance of the allergen, if implicated, is important in the management and treatment of hand eczema. Hence patch test becomes an important tool in identification of allergens [1,2]. Patch testing is a tool to reproduce, in a clinical setting, a mini-model of allergic contact dermatitis using allergens suspended in a vehicle at non-irritant concentrations [3]. Patch test is the only scientific investigation to prove the diagnosis of allergic contact dermatitis.
There is substantial morbidity caused due to hand eczema with significant physical, social and financial implications. Therefore a study of patch testing in hand eczema patients is definitely indicated to determine the role of allergic contact dermatitis in causing hand eczema and the relative importance of different causative allergens in this particular geographical area. We aimed to find out the causes of allergic contact dermatitis in adult patients with hand eczema with the help of patch testing.
Materials and Methods
This was a cross-sectional study conducted between October 2013 and June 2015, at a tertiary care centre in Southern India. The study was done after obtaining approval from the institutional ethics committee which follows the Helsinki Declaration. Consecutive adult patients with hand eczema attending the Department of Dermatology, Venereology and Leprosy, who had given consent to participate in the study, were included in the study. Patients who had received oral steroids in the past 2 weeks and patients with significant eczema elsewhere, apart from feet, were excluded from the study. A potassium hydroxide preparation with skin scraping was done to rule out suspected tinea manuum.
Brief Procedure
After informed consent, detailed history including history of occupational/personal exposure to chemicals, history of atopy and detailed examination findings with area of involvement, morphology and final diagnosis were noted down in the proforma. Patch test was done on these patients with Indian standard series, approved by Contact and Occupational Dermatoses Forum of India (CODFI) and manufactured by CREDISOL® and marketed by Systopic® Laboratories Pvt. Ltd., New Delhi with 20 allergens. The patches were removed after 48 hours. The reading was taken one hour after removal of the patches, to allow the erythema to subside. Another reading was taken after 72 hours [4]. The readings were interpreted according to International Contact Dermatitis Research Group criteria and noted down [1].
Statistical Analysis
The data were analysed using descriptive statistics and inferential statistics. The data were summarized using mean and standard deviation for continuous variables and percentages for categorical and dichotomous variables. The test of association was done with Fisher’s-exact test.
Results
A total number of 59 patients with hand eczema, after applying the inclusion and exclusion criteria, gave the informed consent to participate in the study. However, only 54 of them attended both the 2nd and 3rd day follow-up and were included in the per protocol analysis. Among the 54 participants there was an equal gender distribution of 27 male and 27 female patients.
Out of the 54 participants, 14 of them were housewives (26%), followed by 9 agriculturists (17%), 6 students (11%), 5 masons and 2 housekeeping staff [Table/Fig-1]. Other less common occupations encountered among the hand eczema patients were managers of small firms, research analysts, security personnel, manual labourers, plumbers, workers in a shop, drivers, doll makers as well as retired and unemployed individuals. Nineteen patients (35.19%) gave personal or family history of atopy. A large number of patients (31 out of 54; 57.4%) gave history of regular exposure to detergents. A history of exposure to parthenium was present in 11 patients, to cement and artificial jewellery in 9 patients each and to hair dye in 3 patients. Hyperkeratotic palmar eczema was the most common morphology, observed in 16 patients (29%). This was closely followed by 15 patients with discoid eczema (28%), 9 patients with pompholyx, 6 patients with patchy vesiculosquamous eczema, 5 patients with wear and tear dermatitis, 2 patients with fingertip eczema and 1 patient with recurrent focal palmar peeling.
Occupation-wise distribution of hand eczema patients (n=54).
| Occupations | Number of patients (n=54) | Percentages (%) |
|---|
| Housewives | 14 | 26% |
| Agriculturists | 9 | 17% |
| Students | 6 | 11% |
| Masons | 5 | 9% |
| Housekeeping staff | 2 | 4% |
| Managers | 2 | 4% |
| Others | 16 | 29% |
Out of 19 atopic patients 7 (37%) had pompholyx whereas only 2 of the remaining 35 patients presented with pompholyx. Therefore, atopic patients have a significantly higher chance of developing pompholyx (p=0.006) [Table/Fig-2].
Morphological pattern of hand eczema in relation to atopy.
| History of atopy among hand eczema patients | Pompholyx (n=9) | Morphological patterns other than pompholyx (n=45) | Total |
|---|
| History of atopy-positive (n=19) | 7 | 12 | 19 |
| History of atopy-negative (n=35) | 2 | 33 | 35 |
| Total | 9 | 45 | 54 |
Fishers-exact test (p = 0.006). Significant at p <0.05
Out of the 54 participants who had hand eczema, 34 participants had a negative patch test. The remaining 20 (37%) participants showed patch test positivity to a total of 25 allergens. Nickel was the most common allergen identified in 6 (11.11%) patients, followed by paraphenylenediamine (PPD) in 4 (7.4%) patients [Table/Fig-3]. Cobalt, potassium dichromate and fragrance mix showed positive reaction in 3 patients (5.55%) each. Parthenium showed a positive response in 2 patients. Paraben mix and colophony were identified as the allergen in one patient each.
Positive patch test allergens among hand eczema patients.
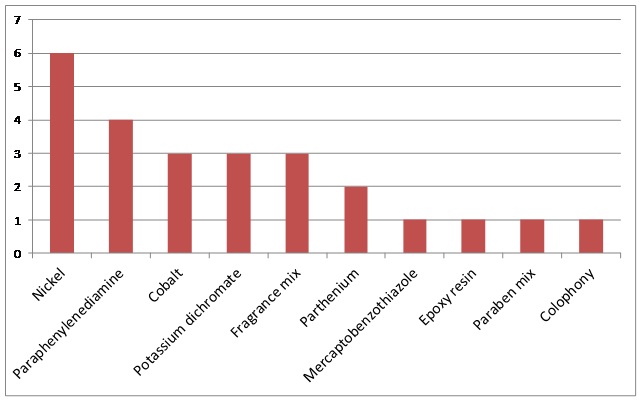
Taking into account the individual patch test readings, the most common allergen causing strongly positive result (+ + or more) was Fragrance mix in 3 patients followed by potassium dichromate and PPD in 2 patients each. One patient each showed strongly positive results to parthenium, nickel and colophony. On the other hand weakly positive results (+) were more with nickel (5 patients), cobalt (3 patients), PPD (2 patients) followed by potassium dichromate, parthenium, mercaptobenzothiazole, epoxy resin and paraben mix in one patient each. Among the 27 female participants, 11 showed a positive result for patch test. Nickel was the positive allergen in 6 female patients whereas 3 each were positive for cobalt and PPD respectively. Further, one female patient each showed positive result for mercaptobenzothiazole, epoxy resin and fragrance mix respectively.
Five patients showed more than one patch test positive reaction of which 3 showed positive reactions to nickel and cobalt. One patient tested positive for mercaptobenzothiazole and epoxy resin and the other patient to colophony with fragrance mix.
The allergens identified on patch testing showed a marked difference according to the gender. Eleven out of 27 female hand eczema patients showed a positive patch test result whereas 9 out of 27 male patients showed a positive patch test reaction. Nickel (6 patients) and cobalt (3 patients) were the common allergens among women, seen exclusively among them. Potassium dichromate (3 patients) and parthenium (2 patients) were the common allergens among men, again seen exclusively among them. Three male patients and 1 female patient tested positive for PPD whereas fragrance mix produced a positive patch test among 2 male patients and 1 female patient respectively.
Out of the 19 participants with history of atopy, only 2 participants showed positive patch test results, both of them for nickel and one of them for cobalt. Out of the 35 non-atopic patients only 4 patients showed a positive patch test result to nickel. There was no statistically significant difference in nickel sensitivity between atopics and non-atopics (p=1.0) by Fisher’s-exact test. Out of the 5 masons, 2 were positive for potassium dichromate, a statistically significant association (p=0.02). Among 9 farmers, only 1 showed a positive patch test result to parthenium. Out of 3 patients with history of using hair dye, 2 were patch test positive for PPD, a statistically significant association, by Fishers exact test (p=0.012). Out of 9 patients with history of using artificial jewellery, 2 were patch test positive for nickel.
Among 31 patients with history of exposure to detergents, patch testing was positive in 11 of them. Three of these 11 participants showed patch test positivity to only nickel, 3 participants to both nickel and cobalt and 3 participants to PPD. Among the other 2 patients, one showed positive reaction to parthenium and the other to mercaptobenzothiazole and epoxy resin.
Analysing for correlation between the morphological pattern and patch test positivity, among 16 hyperkeratotic palmar eczema patients, patch test results were positive in 4 patients with 2 patients showing positive results to fragrance mix, one of them along with colophony. The other 2 patients showed positive result to PPD and parthenium.
Among 15 hand eczema patients with discoid pattern, patch test was positive in 4 participants, potassium dichromate being the allergen in 3 of them. Discoid hand eczema patients showed significantly higher chance of patch test positive result to potassium dichromate by Fisher’s-exact test (p=0.02). Among 9 pompholyx patients, patch test was positive in 3 participants with 2 of them showing positive patch test result to both nickel and cobalt. However, patients with pompholyx did not have a significantly higher chance of a positive result to nickel (p=0.26). Apart from mild itching none of the patients showed any adverse reaction to patch testing.
Discussion
Housewives, agriculturists, students and masons formed the bulk of hand eczema patients in our study, similar to other Indian studies [5–8]. Housewives get exposed to a large number of chemicals and this along with the trauma of rubbing and scrubbing increases the chances of both allergic and irritant contact dermatitis. Studies done in Chandigarh, Delhi, Srinagar and even in Pondicherry showed a higher percentage of masons but lower number of agriculturists in their study compared to our study, possibly because our institution is located in a rural area and our patient population is predominantly rural [5,7–9]. The scenario was completely different in a study done in Denmark, where the common occupations among hand eczema patients were health care workers, bakers, hairdressers, kitchen workers [10].
Atopic diathesis is a very common cause of hand eczema. In our study the percentage of atopic patients was similar to studies by Handa et al., and Suman et al., and even an European study [5,9,11], but surprisingly much higher than the study by Majid [8] and the previous study done in Pondicherry where only a single patient out of 36 hand eczema patients had history of atopy [7].
The morphological pattern of hand eczema in our study was markedly different from the previous Indian studies [Table/Fig-4] [5,7,8].
Comparison of different morphological types of hand eczema in different studies [5,7,8].
| Studies | Hyperkeratotic hand eczema | Pompholyx | Wear and tear hand eczema | Fingertip eczema | Patchy vesiculos-quamous eczema |
|---|
| Handa et al., [5] Chandigarh (n=100) | 9% | 14% | 10% | 5% | Nil |
| Laxmisha et al., [7] Pondicherry (n=36) | 12% | 2.7% | 53% | Nil | 8.3% |
| Majid, [8] Srinagar (n=278) | 12.2% | 6.1% | Nil | 16.1% | 13.6% |
| Present study Pondicherry (n=54) | 29% | 17% | 9.3% | 3.7% | 11.1% |
This emphasizes the lack of uniformity and difficulty in classifying hand eczema. The difference in patient population with a more rural patient population could be responsible for a lower percentage of wear and tear hand eczema patients in our study compared to the previous study done in Pondicherry [7]. We found a significant association of pompholyx with history of atopy, a known association [12]. This probably explains the higher percentage of pompholyx patients in our study compared to the studies by Laxmisha et al., and Majid [7,8], shown in the above table, as our study had a larger number of patients with history of atopy.
As can be seen from the above [Table/Fig-5], the percentage of patch test positivity varied widely in different Indian studies [5–9,13]. The patch test positivity in our study was comparatively lower compared to most of the Indian studies. The probable reason could be a higher contribution of irritant contact dermatitis and endogenous eczema, most commonly atopic eczema for the causation of hand eczema. Potassium dichromate was the most common allergen in the studies done in Chandigarh, Mangalore and Pondicherry [5–7]. The lesser positivity for potassium dichromate in our study could be because of less number of masons among our hand eczema patients, as explained before. However, studies done in Srinagar, New Delhi and Jaipur found nickel positivity to be most common, similar to our study [8,9,13]. Even the study done in Mangalore by Kishore et al., found nickel to be the second most common allergen with a percentage similar to our study [6]. We found patch test positivity to nickel exclusively among women. In the study by Handa et al., 11 out of 14 positive patch test results to nickel occurred in females [5]. Similarly Majid found that 35 out of 45 positive patch test results to nickel occurred in females [8]. Sensitization during ear piercing, exposure to wet work, artificial jewellery and utensils could be the reason behind this finding. This is supported by the fact that, in our study out of 9 patients with history of using artificial jewellery, 2 were patch test positive for nickel. We found nickel to be the most common allergen among pompholyx patients, similar to the study by Handa et al., and another European study [5,14]. The absence of positive patch test results to nickel in the study by Laxmisha et al., can be explained by the less number of pompholyx patients in their series as mentioned earlier [7].
Comparison of patch test results in different studies (positive allergens expressed as % of total no. of patients) [5–9,13].
| Studies | Patch test positivity | Nickel | PPD | Cobalt | Potassium dichromate | Fragrance mix |
|---|
| Handa et al., [5] Chandigarh (n=100) | 65% | 14% | 13% | 1% | 25% | 16% |
| Kishore et al., [6] Mangalore, (n=50) | 82% | 18% | Not known | Not known | 26% | Not known |
| Laxmisha et al., [7] Pondicherry (n=36) | 52.78% | Nil | Nil | 2.77% | 27.77% | 2.77% |
| Majid, [8] Srinagar (n=278) | 48.5% | 16.1% | Nil | 2.9% | 9.7% | 6.1% |
| Suman et al., [9] New Delhi, (n=100) | 67% | 20% | Not known | Not known | 18% | Not known |
| Agarwal et al., [13] Jaipur, (n=21) | 30% | 14.28% | Nil | Nil | 9.52% | 4.76% |
| Present study, Pondicherry (n=54) | 37% | 11.1% | 7.4% | 5.55% | 5.55% | 5.55% |
The relation between pompholyx and nickel could be due to high nickel content of diet which is known to result in worsening of vesicular hand eczema in patients sensitized to nickel [15]. One of the studies found nickel sensitivity to be significantly more common in atopics, unlike our study [5].
Potassium dichromate allergy was significantly common among masons in our study, a finding shared by all the other studies. Lack of protective measures while handling cement and non-availability of hypoallergenic cement are the main reasons behind this significant occupational hazard. In most of the European countries hypoallergenic cement has been made legally mandatory but similar laws are yet to be enacted in India. The absence of social security system in India makes changing the profession difficult for the patient resulting in continuous exposure and further exacerbation. Significantly higher potassium dichromate allergy found among discoid hand eczema patients indicate that cement allergy can present with a morphological picture resembling discoid eczema.
Significant association of PPD allergy with the use of hair dye was found in another study in addition to ours [5]. The widespread use of hair dyes and lack of public awareness about PPD allergy is responsible for this problem. Allergy to fragrance mix in our study was less common than in Chandigarh but comparable to studies from Jaipur, Srinagar and the previous study in Pondicherry [5,7,8,13]. This could be due to difference in the pattern of use of cosmetics in different parts of India. In addition to cosmetics, detergents, soaps and other personal care items can also sensitize an individual to fragrance mix. Allergy to both PPD and fragrance mix seen in both male and female emphasizes widespread sensitization across both genders.
As mentioned before, detergents are an important source of sensitization, proven by positive patch test results to nickel, cobalt and PPD among patients with history of exposure to detergents.
The percentage of patch test positivity among hyperkeratotic hand eczema patients in our study was similar to that by Handa et al., [5]. Other studies have shown variable results to patch testing in hyperkeratotic hand eczema patients [16]. The frequent concurrence of positive patch test results to nickel and cobalt is due to cobalt being a common contaminant in nickel as described earlier. Parthenium sensitization although widely suspected, was not a common reason of hand eczema among farmers.
The few studies conducted abroad on patch testing in hand eczema patients cannot be compared to the Indian studies because of a completely different pattern of allergen exposure in the personal and occupational environment and different sets of allergens used in the standard series. Even then the patch test positivity rate, common morphological types and common allergens were similar. Hald et al., found patch test positive results in 45.6%, similar to some Indian studies [11]. Pompholyx and wear and tear hand eczema were the common clinical types [14]. Nickel, fragrance and cobalt allergy were common among women and fragrance, nickel and chromate allergy common among men [11].
Lack of any serious side effects in any of our patients demonstrated that patch test is a non-invasive and remarkably safe diagnostic procedure.
Limitation
Inclusion of larger number of patients would have definitely increased the validity of the conclusions. Further a 7th day follow-up would have detected delayed positive reactions.
Conclusion
We found that housewives, agriculturists, students and masons are predisposed to develop hand eczema and most cases of hand eczema are not due to allergic contact dermatitis. History of atopy was common among patients with pompholyx. Nickel was the most common allergen in our series. Therefore, patch testing remains an essential tool in the diagnostic work up of patients with hand eczema.
Fishers-exact test (p = 0.006). Significant at p <0.05