Isolated arterial dissection without aortic pathology has been rarely reported in mesenteric vessels. The natural history and appropriate treatment for this disease is uncertain because of the scarcity of literature which limits the data available to the clinician, resulting in management challenges. Herein, we report a rare case of a 42-year-old Tunisian man with spontaneous dissection and aneurysmal dilatation of the Celiac Artery (CA) and the Superior Mesenteric Artery (SMA) with partial thrombosis. This case was successfully managed conservatively with heparin infusion and blood pressure control and the patient remained symptom free at 15 months follow up. This case demonstrates that conservative management may be warranted in non-complicated isolated visceral arterial dissection.
Non-operative, Spontaneous dissection, Visceral arterial dissection
Case Report
A 42-year-old Tunisian man was presented to the emergency department with acute epigastric pain, nausea and vomiting. He was a smoker and had a past medical history of hypertension. On physical examination, there was no evidence of peritonitis and vital signs were normal.
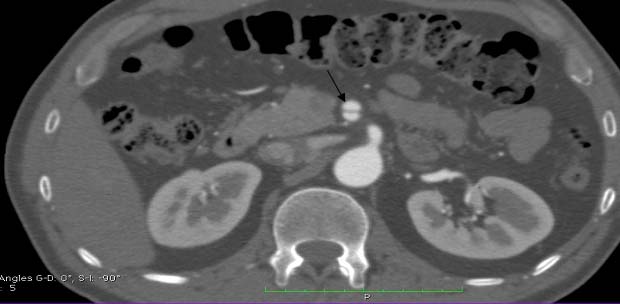
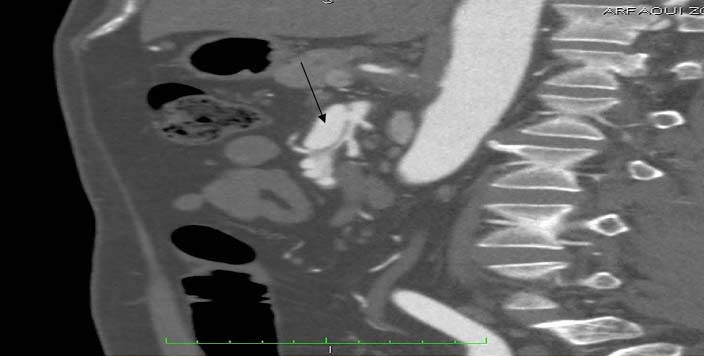
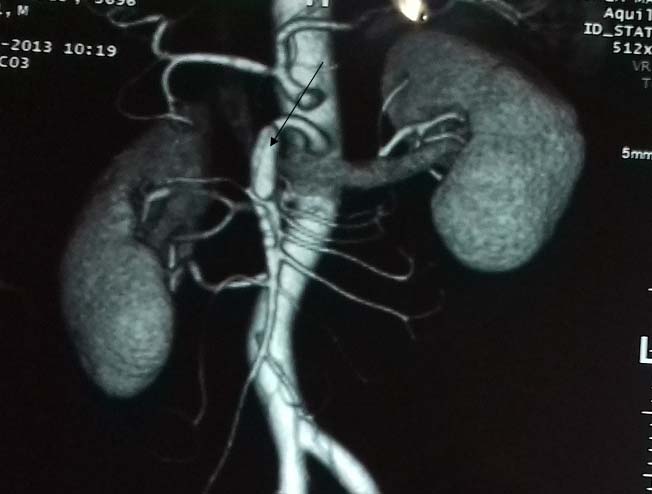
Laboratory data revealed leukocytosis with a white blood cell count of 11,000/ml. There was no evident pathology in the abdominal sonographic examination. An abdominal computed tomography scan with intravenous contrast showed a normal thoraco-abdominal aorta. However, dissection of both the celiac trunk and SMA was determined. SMA dissection was classified as Sakamoto type II b. There was no bowel oedema or free fluid. The dissection of the celiac artery was approximately 22mm long with aneurysmal dilatation [Table/Fig-1,2 and 3] with partial thrombosis causing moderate narrowing.
The characteristics of the patient.
| Age/Gender | 42yr/male |
| Risk factor | Hypertension, smoking |
| Symptoms | Abdominal pain, nausea, vomiting |
| Location & length of dissection | CA:22mm+aneurysmal dilatationSMA:18mm |
| Sakamoto classification | II b |
| Treatment | Heparin & aspirin |
Abdominal CT scan with intravenous contrast (longitudinal view) reveals an isolated celiac artery dissection (arrow) measuring 22mm in length with aneurysmal dilatation.

Abdominal CT scan with IV contrast (Longitudinal view): demonstrates Celiac artery dissection.

Dissection of SMA was extending for approximately 1.8cm, accompanied by contrast accumulation in the wall due to ulceration in the proximal part of the artery. SMA was visualized as 60% narrowed because of the dissection [Table/Fig-4,5 and 6]. Inferior Mesenteric Artery (IMA) and renal arteries were normal. Conservative treatment was the method of choice. It was based on anticoagulation, pain and hypertension control. His abdominal pain resolved in 2 days. The patient was discharged home with warfarin and aspirin. Follow-up CT scan at 3 and 6 months demonstrated that the dissections and aneurysmal dilatation were both stable. The patient was continuing to do well on his 15 month clinical follow-up. Further follow-up CT examinations were planned.
Axial contrast enhanced computed tomographic scan through the upper abdomen shows an intimal flap (arrow) in the SMA This finding is consistent with SMA dissection.
Abdominal 4 CT scan with IV contrast (Longitudinal view) demonstrates a dissection of SMA with Partial thrombosis causing 60% stenosis.
CT scan tridimensional view aneurysmal dilatation of the SMA.
Discussion
Spontaneous Visceral Artery Dissection (VAD) is defined as a dissection of the SMA, CA, IMA or renal artery, in the absence of aortic dissection. It is a rare occurrence and till date, about 110 cases have been reported [1,2]. The disease is increasingly recognized due to the widespread use of advanced abdominal imaging technology [3]. Demographic data shows that the majority of cases have been reported from Japan followed by the United States and then Europe, South America, and Asia [4]. To our knowledge, this case is the first one reported in Tunisia.
The majority of cases occur in men between the ages of 41 and 67 years [5]. VAD most frequently involves the SMA and less frequently the celiac trunk. Spontaneous visceral artery dissection is an exceptionally rare event that occurs in both celiac and superior mesenteric arteries. Because of its rarity, the aetiopathogenetic factors remain unclear and no definite cause is usually found. Postulated pathogenesis include fibro muscular dysplasia, atherosclerosis, hypertension, abdominal trauma, connective tissue disorder [6].
Often, as in our case, no aetiology other than hypertension could be found. Diagnosis of spontaneous VAD can be challenging. Initial clinical presentation is variable and is always nonspecific. The presentation can include abdominal pain, vomiting, nausea, bloating or weight loss [7]. Some patients may be asymptomatic and others may present with severe complications (bowel ischemia and arterial rupture). Patients with CA lesions are often less symptomatic than those with SMA lesions [8]. There are no specific laboratory markers. Abdominal ultrasound is the first choice of investigation for many patients with abdominal pain and can be helpful if aneurysmal dilatation or the intimal flap is observed. However, it is an insensitive tool [9]. Angio-CT scan is the best diagnostic tool: it allows visualization of false and true lumen and possible signs of ischemic bowel or parenchymal infarction [10].
Sakamoto classified SMA dissection into 4 types [Table/Fig-7]:
Sakamoto’s classification of spontaneous isolated dissection of superior mesenteric artery.
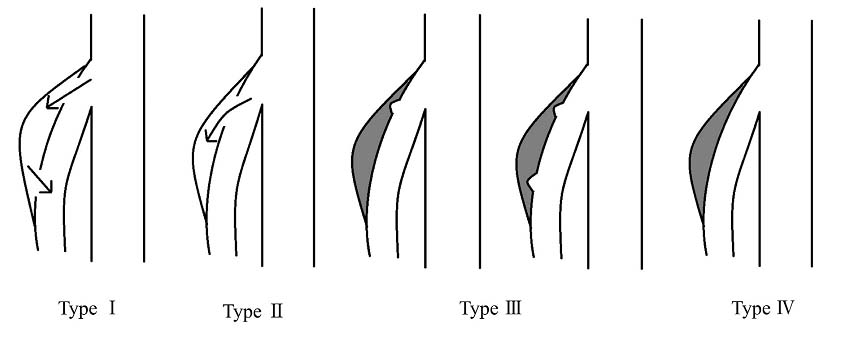
Type I: false lumens with both entry and re-entry;
Type II: represented “cul-de-sac” shaped false lumens without re-entry;
Type III: represented thrombosed false lumens with ulcer-like projections defined as localized blood filled pouches protruding from the true lumens into the thrombosed false lumens;
Type IV represented completely thrombosed false lumens without ulcer-like projections [11].
Mesenteric Angiography (MA) is a valid diagnostic tool. Unfortunately, it is invasive; it may cause embolization or dissection. Thus, it should be done in patients with worsening of symptoms and in those who necessitate surgical or endovascular treatment. Management of this condition is also challenging. There is no well-established approach. A variety of treatment options have been described including conservative management (medical), endovascular treatment and open surgery.
Conservative treatments include anti-platelet, anticoagulants and antihypertensive therapy. Anti-coagulation is considered valid for this pathology because of the risk of thrombosis in these visceral arteries because of the small caliber and relatively slower blood flow as compared to the aorta [12]. Anticoagulation has been successful in patients with 90% stenosis of the main trunk of the SMA. Most patients which can be initially managed conservatively if there are no clinical and imaging signs indicating rupture of the artery branches or bowel ischemia [13]. Nevertheless, a conservative approach, does not prevent disease progression, one-third of such patients may need surgery or stenting [14,15].
The absolute indication for invasive treatment (emergency surgical intervention) is bowel infarction and arterial rupture [16]. The other indications for surgical intervention in SMA dissection are: increased size of the aneurysm, intra-luminal thrombosis, abnormal blood flow through the vessel and persistent symptoms despite anticoagulation. In celiac artery dissection surgical repair is recommended in the presence of occlusive lesions, arterial rupture, aneurysm formation or extension of the dissection into the hepatic arteries [17]. Surgical treatment consists of aortomesenteric bypass or mesenteric artery re-implantation.
An advance in endovascular surgery has been useful in managing patients who need revascularization. In cases with short segment dissection without bowel ischemia or with signs of peritonitis and in patients who are not improving on conservative therapy and who have an increased risk of perioperative complications, stent placement is indicated. This helps to seal the entry point of the dissection and often self-expandable stents are used, because they are soft and elastic [18].
Based on the above CT scan classification, type I may be managed conservatively; type II has an increased chance of bowel ischemia;Type III can expand and form an aneurysm and type IV resolves and does not need long-term followup. Cho and Carter have suggested algorithms for the management of VAD dissection based on patient presentation and clinical course [19]; acute abdomen is managed surgically.
Asymptomatic patients are managed expectantly with follow-up imaging. Patients who fail conservative therapy or those who develop or worsen symptoms undergo endovascular stenting or surgery. There are no current recommendations for the interval between imaging studies for initial management and follow-up. Sakamoto et al., in their study including 12 patients, recommended a follow-up CT scan at 1 week, 2 weeks, 1 month, 3 months, 6 months and at 6-month intervals thereafter [11]. Follow up should be continued until there is complete resolution of dissection in patients treated conservatively. No data with regard to duration of follow-up in patients undergoing revascularization procedures is currently available. Thus, long-term follow-up studies are needed to clarify follow-up schedule.
Retrospectively, our patient improved with medical management but stenting can be an option in the initial presentation. His clinical improvement on full anticoagulation highlights the applicability of medical management.
Conclusion
This case report documents a very rare presentation of simultaneous isolated dissection of CA and SMA. It is a situation that should be kept in mind in the differential diagnosis of abdominal pain and conservative management may be warranted in non-complicated cases.
[1]. Ko SH, Hye R, Frankel DA, Management of spontaneous isolated visceral artery dissectionAnn Vasc Surg 2015 29(3):470-74. [Google Scholar]
[2]. Seidita A, Barbiera F, Murmura E, Accardi M, D’Alcamo A, Randazzo G, Isolated dissection of the superior mesenteric artery: a case report and literature reviewItal J Med 2013 8(1):56 [Google Scholar]
[3]. D’Ambrosio N, Friedman B, Siegel D, Katz D, Newatia A, Hines J, Spontaneous isolated dissection of the celiac artery: CT findings in adultsAJR Am J Roentgenol 2007 188(6):W506-11. [Google Scholar]
[4]. Kim YW, Current Understandings of Spontaneous Isolated Superior Mesenteric Artery DissectionVasc Spec Int 2016 32(2):37-43. [Google Scholar]
[5]. Bauersfeld SR, Dissecting aneurysm of the aorta; a presentation of 15 cases and a review of the recent literatureAnn Intern Med 1947 26(6):873-89. [Google Scholar]
[6]. Nonami S, Nakanishi T, Tanizaki S, Matsumoto T, Sera M, Maeda S, Characteristics and diagnostic pitfalls of spontaneous visceral artery dissection in the emergency departmentAm J Emerg Med 2016 34(6):1092-96. [Google Scholar]
[7]. Mousa AY, Coyle BW, Affuso J, Haser PB, Vogel TR, Graham AM, Nonoperative management of isolated celiac and superior mesenteric artery dissection: case report and review of the literatureVascular 2009 17(6):359-64. [Google Scholar]
[8]. Fenoglio L, Allione A, Scalabrino E, Alberto G, Benedetti V, Pomero F, Spontaneous dissection of the celiac artery: a pitfall in the diagnosis of acute abdominal pain. Presentation of two casesDig Dis Sci 2004 49(7-8):1223-27. [Google Scholar]
[9]. Lynch TG, Hobson RW, Kerr JC, Brousseau DA, Silverman DG, Reilly CA, Doppler ultrasound, laser Doppler, and perfusion fluorometry in bowel ischemiaArch Surg Chic Ill 1960 1988 123(4):483-86. [Google Scholar]
[10]. Rha SE, Ha HK, Lee SH, Kim JH, Kim JK, Kim JH, CT and MR imaging findings of bowel ischemia from various primary causesRadiogr Rev Publ Radiol Soc N Am Inc 2000 20(1):29-42. [Google Scholar]
[11]. Sakamoto I, Ogawa Y, Sueyoshi E, Fukui K, Murakami T, Uetani M, Imaging appearances and management of isolated spontaneous dissection of the superior mesenteric arteryEur J Radiol 2007 64(1):103-10. [Google Scholar]
[12]. Aydin S, Ergun E, Fatihoglu E, Durhan G, Kosar PN, Spontaneous Isolated Celiac Artery and Superior Mesenteric Artery Dissections: A Rare CasePol J Radiol Pol Med Soc Radiol 2015 80:470-72. [Google Scholar]
[13]. Subhas G, Gupta A, Nawalany M, Oppat WF, Spontaneous isolated superior mesenteric artery dissection: a case report and literature review with management algorithmAnn Vasc Surg 2009 23(6):788-98. [Google Scholar]
[14]. Gobble RM, Brill ER, Rockman CB, Hecht EM, Lamparello PJ, Jacobowitz GR, Endovascular treatment of spontaneous dissections of the superior mesenteric arteryJ Vasc Surg 2009 50(6):1326-32. [Google Scholar]
[15]. Park YJ, Park KB, Kim D-I, Do YS, Kim DK, Kim Y-W, Natural history of spontaneous isolated superior mesenteric artery dissection derived from follow-up after conservative treatmentJ VascSurg 2011 54(6):1727-33. [Google Scholar]
[16]. Morris JT, Guerriero J, Sage JG, Mansour MA, Three isolated superior mesenteric artery dissections: update of previous case reports, diagnostics, and treatment optionsJ Vasc Surg 2008 47(3):649-53. [Google Scholar]
[17]. Hashidomi H, Saito S, Spontaneous isolated superior mesenteric artery dissection treated under intravascular ultrasound guidanceCardiovascInterv Ther 2011 26(3):269-73. [Google Scholar]
[18]. Satokawa H, Takase S, Seto Y, Yokoyama H, Gotoh M, Kogure M, Management strategy of isolated spontaneous dissection of the superior mesenteric arteryAnn Vasc Dis 2014 7(3):232-38. [Google Scholar]
[19]. Yun WS, Kim YW, Park KB, Cho SK, Do YS, Lee KB, Clinical and angiographic follow-up of spontaneous isolated superior mesenteric artery dissectionEur J VascEndovasc Surg Off J Eur Soc Vasc Surg 2009 37(5):572-77. [Google Scholar]