Lower limb chronic venous insufficiency affects more than one third of general population in their lifetime [1–4]. Superficial venous insufficiency develops due to venous valvular dysfunction resulting in venous hypertension, gradual dilatation and tortuosity of the involved veins and its small subdermal tributaries [3]. Minimally invasive treatment using endovenous laser ablation and/or foam sclerotherapy have replaced open surgery all over the world, because of increased safety, efficacy, faster recovery and better cosmetic results [1,3,5–12].
Laser ablation is mostly performed after perivenous Tumescent Injection (TI) which anaesthetises the vein while thermo-ablated with laser and protects adjacent tissues from heat, especially skin from burns in case of very superficial veins [3,5,6,13]. Multiple punctures, especially in the inner aspect of thigh and injection of tumescent solution in perivenous space causes significant pain [5,6]. Additionally, foam sclerotherapy performed most of the time concomitantly with laser ablation or sometimes as sole treatment causes considerable burning sensation.
Different methods are currently employed for pain control during these procedures. Spinal or even general anaesthesia is used by some physicians, especially surgeons [14]. Although these confer total analgesia, ideally they shouldn’t be advocated because of multiple reasons, the foremost of which is increased risk of deep venous thrombosis due to post procedure immobilisation [3,5,6,15–17]. Other pitfalls are potential complications of the anaesthesia itself ranging from headache, nausea and lingering backache (in spinal anaesthesia) to cardiac arrest and shock; additional cost and personnel requirement for anaesthesia and hospital stay prolongation [5,6]. Most other physicians use intravenous sedation with narcotics, which carry the risk of hypotension, respiratory depression and sedation which again, would interfere with post- procedure mobility [6].
An alternative form of analgesia in these situations is Ultrasound (US) guided nerve block because femoral, saphenous and sciatic nerves, which can be anaesthetised in isolation, have cutaneous innervation along the great and short saphenous territories and immediate post-op mobilization and early discharge from the hospital is possible with these techniques [2,5,6,16,18]. The purpose of this prospective study was to apply these techniques and describe their pain control efficiency and safety.
Materials and Methods
In this multicentre prospective observational study approved by Institutional Review Boards, all patients referred to the interventional radiology clinics with symptomatic varicose veins secondary to junctional (saphenofemoral or saphenopopliteal) and/or perforator incompetence, who agreed to treatment by laser and/or sclerotherapy were included. Extremely anxious patients who requested sedation were excluded from the study. The minimum number of procedures required to be studied considering a confidence interval of 95%, and a margin of Error (E) of 0.05 was calculated to be 383 using the formula-
where Zα was taken as 1.96 corresponding to 95% confidence, and P was taken as 0.47 from a similar previous study by Yilmaz S et al., where 47% of patients had no pain (visual analogue pain score 0 or 1) during endovenous laser ablation after femoral and sciatic nerve blocks [6]. Over the time period of 33 months from August 2013 to April 2016, 856 legs of 681 patients with symptomatic superficial venous insufficiency were treated with laser ablation and/or sclerotherapy using different nerve blocks for intra-procedural pain control. The type of nerve block required was determined by the location of varices. Combined femoral and saphenous block was used for anteromedial thigh and leg varices secondary to Saphenofemoral Junction (SFJ) and anteromedial perforator incompetence; sciatic nerve was blocked for posterior and posterolateral leg varices secondary to Saphenopopliteal Junction (SPJ) and posterior perforator incompetence; and saphenous block in isolation was performed for anteromedial leg varices with competent SFJ secondary to anteromedial leg perforator incompetence. All three nerves were blocked for patients with varices from combined SFJ, SPJ and perforator incompetence.
Informed and written consent was taken from all patients for nerve block, laser ablation and sclerotherapy after the details and possible complications of the procedure were expounded. 2% chlorhexidine in ethanol was used for disinfection in all patients. 2% Lignocaine hydrochloride (Lox 2%, Neon Laboratories Limited, Mumbai) was used for nerve block and TI in all patients but one, who had history of allergy to local anaesthesia – 2% Cardiac lignocaine (Loxicard, Neon Laboratories Limited, Mumbai) was used in this patient uneventfully. The whole limb from groin to ankle was disinfected before the procedure and a sterile towel was used to cover the foot. Linear transducer of a portable ultrasound machine (either L12-3 Linear Array, CX50 Compact Xtreme Ultrasound System, Philips Healthcare; or a 12L-RS Linear Probe, GE Vivid E Portable Ultrasound System, GE Healthcare) was disinfected with the same solution and was ensheathed in a sterile endoscopy camera cover. A pre-procedural thorough ultrasound mapping of incompetent vessels was performed and size of Great Saphenous Vein (GSV) of Short Saphenous Vein (SSV) to be ablated was measured at selected sites.
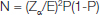
Femoral nerve block: With patient in supine position, the linear US transducer was used to insonate the common femoral vessels transversely at the groin with the transducer placed over the inguinal creases. Immediately lateral to the common femoral artery and deep to the fascia iliaca, femoral nerve could be readily identified [Table/Fig-1a]. In case of difficulty, the probe was tilted cranially or caudally which brightened the nerve making it conspicuous. Using in-plane technique, a single skin puncture was made with a 22 G 1.5 inch long needle to inject 10ml of local anaesthetic solution all around the nerve, without puncturing the nerve [Table/Fig-1b].
US-guided Femoral nerve block. (a) US anatomy at the groin showing the femoral nerve as a hyperechoic triangle (asterisk), lateral to the common femoral artery (Ar) and vein (V). (b) US image after anaesthetic infiltration showing the injectate (arrows) surrounding the femoral nerve (asterisk).
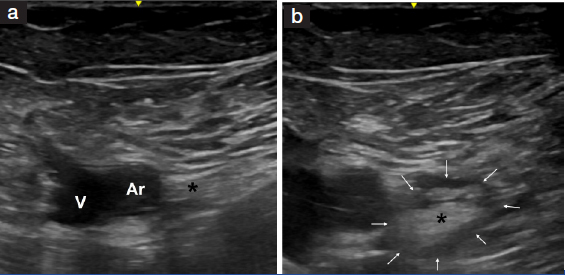
Saphenous nerve block: Saphenous nerve was targeted at the junction of mid and lower thigh in all cases and when combined with femoral block, was always performed 2 minutes after femoral block (femoral block would numb the skin puncture required for this block). US visualization of saphenous nerve [Table/Fig-2a] was overall poor and could be seen only in approximately 35% of the patients (most of whom were lean). With patient in supine position and limb externally rotated, the femoral vessels in the subsartorial canal were located transversely using the linear US transducer. The intermuscular plane between the sartorius and vastus medialis muscles medial to the vessels was then identified [Table/Fig-2a]. Skin was punctured with a 22G needle at the medial end of the transducer and using in-plane technique, needle tip was positioned in the intermuscular plane medial to the femoral vessels and 10ml of local anaesthetic solution was infiltrated. In patients where the nerve could be visualized, the nerve was selectively targeted within the intermuscular plane and the anaesthetic solution was infiltrated around it [Table/Fig-2b].
US-guided Saphenous nerve block. (a) US anatomy at the medial part of the lower thigh showing the saphenous nerve (asterisk) as a echogenic structure anteromedial to the superficial femoral artery (Ar) and vein (V) in the inter-muscular plane between the Sartorius (SM) and the vastusmedialis (VM) muscles. (b) US image after anaesthetic infiltration showing the injectate (arrows) surrounding the saphenous nerve (asterisk).
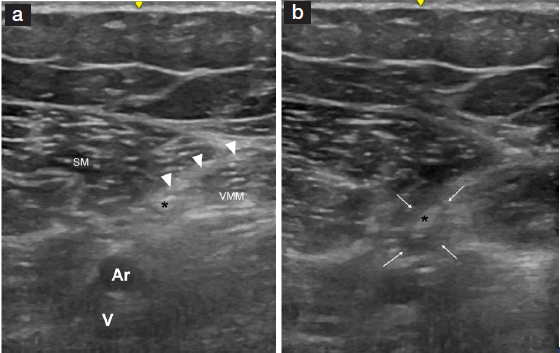
Sciatic nerve block: Patient was positioned in prone or lateral decubitus position. The popliteal vessels were identified in the popliteal fossa. The anterior tibial and common peroneal nerves could be seen superficial and lateral to the popliteal artery which were traced superiorly into the lower thigh till their division from a single sciatic nerve could be seen [Table/Fig-3a]. A 10ml of local anaesthetic solution was injected around the sciatic nerve using in-plane technique taking care not to poke the nerve [Table/Fig-3b].
US-guided Sciatic nerve block. (a) US anatomy at the dorsal aspect of lower thigh showing the sciatic nerve (asterisk) as a bright oval echogenic structure superficial to the popliteal vein (V) and artery (Ar). (b) US image after anaesthetic infiltration showing the injectate (arrows) surrounding the sciatic nerve (asterisk).
Laser ablation and/or sclerotherapy procedures were started approximately five minutes after the nerve blocks. For laser ablation, GSV was punctured (without additional anaesthetic infiltration) either just below the knee or above the ankle (depending on the extent of dilated GSV) and GSV from 1.5 to 2 cm below the SFJ to the puncture site was ablated with energies ranging between 24 to 40J/cm using standard technique after perivenous tumescent injection throughout the length of the vein using a solution made by adding 30ml of 2% lignocaine in 500ml Ringer lactate. Similar technique was used to ablate straight segments of SSV punctured usually in lower leg. Incompetent perforators were assessed for straight segment in their course, which if present were ablated by introducing laser fibre into the perforator under ultrasound guidance through an 18 G puncture needle, after tumescent injection around the perforator.
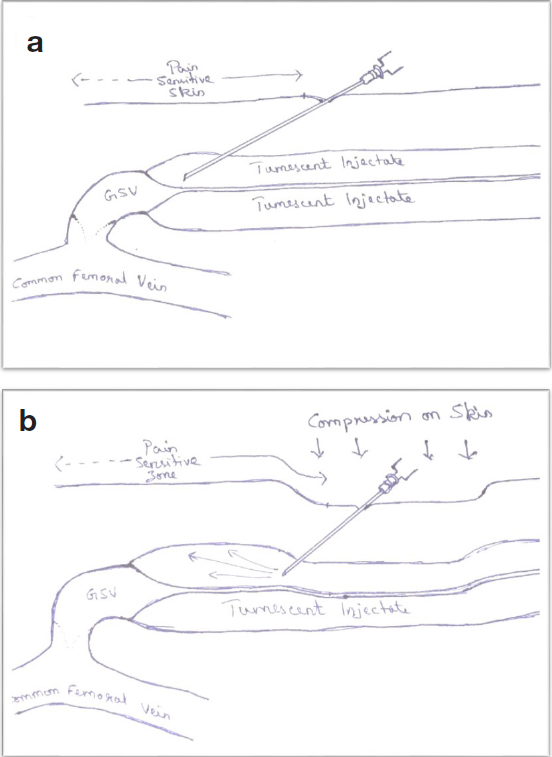
During TI for GSV ablation, certain patients had preserved sensations in the upper-most part of the thigh (sensation was checked in upper thigh in all patients before puncturing for TI and the extent of un-anaesthetised skin from the SFJ was measured). In those cases, TI of the cranial-most segment of the GSV was performed by either using a 22G lumbar puncture needle through a low puncture of anaesthetised skin [Table/Fig-4a], or by securing a needle in perivenous space lower down and applying manual compression at the site of injection to drive the further injected tumescent cranially without actually having to puncture the un-anaesthetised skin higher up [Table/Fig-4b].
Schematic pictures depicting methods of circumventing the issue of preserved cutaneous sensation in the upper thigh below the SFJ by either injecting tumescent solution in the cranial most segment of GSV through a low puncture using a long lumbar puncture needle (a) or applying manual compression at a lower site of injection to force the tumescent solution cranially (b).
Foam sclerotherapy was performed for residual non-saphenous collaterals after laser ablation. Isolated foam sclerotherapy was performed in patients having anteromedial leg varices secondary to isolated perforator incompetence; in patients with isolated SPJ incompetence with mildly dilated or tortuous SSV; and in patients with residual/ recurrent varices. For foam sclerotherapy, the abnormal superficial veins were cannulated using 22G scalp vein sets, position confirmed by blood aspiration and contrast injection under fluoroscopy, perforators mapped by venography and foam made by agitating sodium tetradecyl sulphate and air in 1:3 proportion across a partially open three way stop cock was injected into the vein taking precautions to prevent deep vein extension of sclerosant by either stopping injection when sclerosant reaches the perforator or by occluding the perforator by compression during injection. Additional measures like alternate dorsi and plantar flexion of the ankle or maintaining saline flow in posterior tibial vein through an intravenous cannula inserted by US guidance was used in certain cases to immediately wash out any sclerosant entering the deep veins.
After these procedures, compression stockings were applied on the intervened leg till the upper thigh. Motor block was assessed by evaluating muscle weakness. For femoral block, in supine position, the patient was asked to flex the hip and with the hip flexed, extend the knee. Motor block was graded severe if the patient was unable to extend the knee, moderate if unable to sustain extension against gravity and mild if unable to sustain extension against an applied resistance. Saphenous nerve, being totally cutaneous was not assessed for. For sciatic nerve block, the patient was asked to dorsi and plantar flex the foot, and motor block was graded severe if the patient was unable to move the foot, moderate if able to move toes but not the foot at the ankle, mild if able to perform restricted dorsi and plantar flexion.
Patients were encouraged to walk if there was no significant motor block. In case of motor block, patients were asked to actively dorsi and plantar flex the foot (after femoral block) or flex-extend the knee (after sciatic block) and flex the hip in frequent cycles till they could walk. A visual analogue pain scale was employed for assessment of procedural pain in all cases. Fire stats version 1.6 was used for statistical analysis. Wilcoxon-Mann-Whitney U test was used for comparison of pain score distribution between different groups; particularly to determine the effectiveness of the two above described techniques to circumvent the problem of un-anaesthetized skin of the upper thigh after femoral block.
Results
Demographic and clinical details of the patients in the present study are provided in [Table/Fig-5]. Nerve blocks (femoral, saphenous and sciatic in 769, 808 and 52 limbs) could be successfully performed in all patients. Site of incompetence, type of nerve block employed, and procedure performed in the study population is provided in [Table/Fig-6]. Visual Analogue Pain Scores (VAS) were found to be 0 or 1 in 591 (69%), 2 or 3 in 214 (25%) and 4 in 51 (6%) legs with no score above 4 [Table/Fig-7,8] in any of the patients. Considering absence of pain in 69% patients (VAS of 0 or 1) and comparing with that of 47% in a previously described study by Yilmaz S et al., post-hoc power of this study was found to be 100% [6].
Patients’ demographic and clinical details.
| Number of patients | 681 patients, 856 limbs (bilateral in 175) |
|---|
| Age | 22 to 93 years |
| Sex | 366 males and 315 females |
| Recurrent varices after previous sclerotherapy or surgery | 52 limbs |
| Clinical classification(CEAP) | C1 (n = 52)C2 (n = 92)C3 (n = 138)C4a (n = 109)C4b (n = 136)C5 (n = 53)C6 (n = 276) |
Incompetent veins and nerve blocks employed in the study population.
| Number of patients | Incompetent veins | Procedure performed | Nerve block employed |
|---|
| 762 | GSV +/- anteromedial leg PV | Laser ablation of GSV in all cases and concurrent sclerotherapy in 641 | Combined femoral + saphenous |
| 39 | Isolated anteromedial leg PV | Laser ablation of PV / collateral veins in 18 and sclerotherapy in 21 limbs. | Saphenous |
| 48 | SSV +/- posterolateral leg PV | Laser ablation of SSV in 36 and sclerotherapy in 23 limbs (11 limbs had both) | Sciatic |
| 7 | GSV + SSV +/- leg PV | Laser ablation of GSV in all, laser ablation of SSV in 4, sclerotherapy in 6 | Combined femoral + saphenous + sciatic |
GSV – great saphenous vein
SSV – short saphenous vein
PV – perforator veins
Visual pain scoring in separate nerve blocks.
| Visual analogue pain score | 0 | 1 | 2 | 3 | 4 |
|---|
| Femoral + saphenous (762) | Before* (347) | 155 | 61 | 50 | 45 | 36 |
| After* (415) | 207 | 105 | 69 | 22 | 12 |
| Saphenous (39) | 14 | 10 | 10 | 5 | 0 |
| Sciatic (48) | 23 | 11 | 7 | 4 | 3 |
| Femoral + saphenous + sciatic (7) | 3 | 2 | 1 | 1 | 0 |
* Before and after application of techniques to circumvent the problem of un-anaesthetized upper-most anterior femoral skin.
Distribution of patients as per their procedural visual analogue pain score.
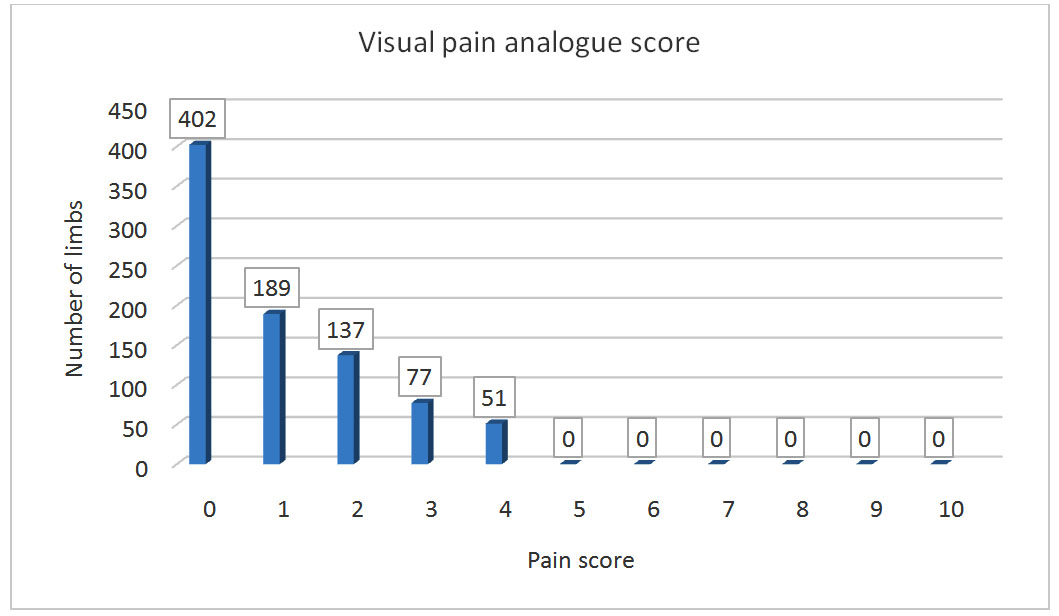
A total of 169 patients (22%) had a strip of un-anaesthetised skin in the upper most part of anterior thigh, extending approximately 5 to 12 cm below the SFJ. They contributed to most of the patients with higher VAS in our initial experience due to pricking the skin and tumescent injection in the upper-most thigh not numbed by femoral block. A few of such patients also complained of mild pain in the groin and upper thigh region lasting for as long as three weeks. Pain scores showed a significantly better distribution after introducing the two above described techniques to circumvent this problem (p = 0.008). Pain score comparison showed no statistically significant difference between patient groups who had femoral and isolated sciatic nerve blocks (p=0.288) or between patient groups who had sciatic and isolated saphenous nerve block (p=0.2).
Technically problematic venous spasm, which we used to encounter occasionally before we used nerve blocks, was not experienced in any of the patients in this study. Visually appreciable increase in diameter of great saphenous vein after femoral block was found initially in our study but it was quantitated (percentage increase in the average of two orthogonal diameters at a specific location) only in 106 patients, and it ranged from 12.5% to 38% with a mean of 22%.
Motor weakness after femoral block was seen in 163 limbs (21%), which was mild in 122 limbs and moderate in 41. Seven (13%) patients had mild (n=5) or moderate (n=2) motor weakness after sciatic nerve block. No case of severe motor block was observed. In patients with motor block, weakness was observed for an average period of two and a half hours, and lasted a maximum of four and a half hours after nerve block.
None of the patients in our study group were complicated by lignocaine toxicity or deep venous thrombosis. Follow-up examination and US was performed one week and one month after the procedure.
Discussion
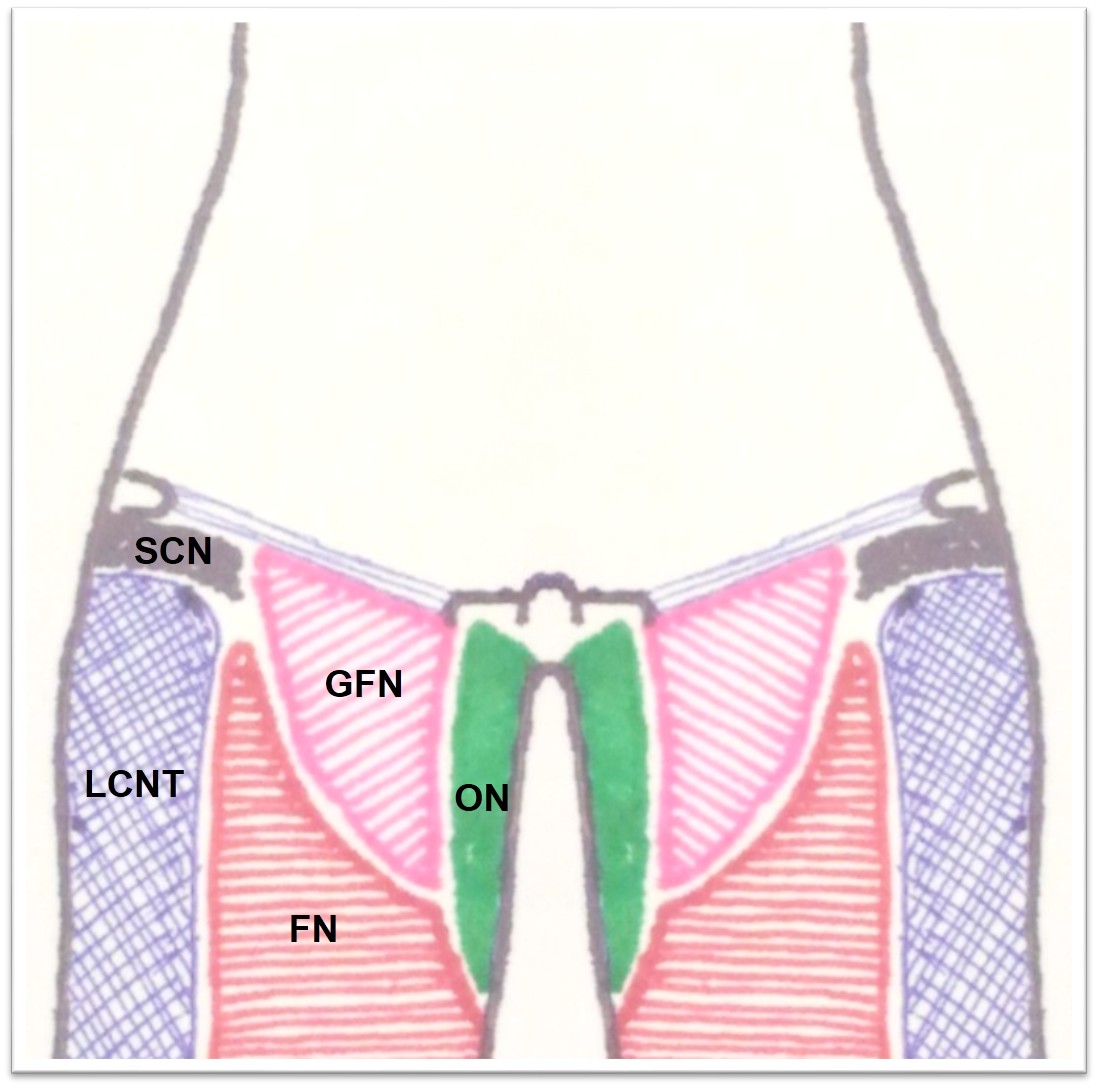
Most of the cutaneous sensation of the lower limb is carried by the femoral and sciatic nerves. Femoral nerve is a large nerve of L2 to L4 lumbar plexus derivation blocking which results in anaesthesia of the anterior and medial thigh till the knee and a variable cutaneous strip on the medial leg [6,19–21]. Saphenous nerve is a cutaneous nerve from the posterior division of the femoral nerve, and carries sensation from the medial aspect of the leg down to the ankle and foot [20,21]. Sciatic nerve is the largest human nerve of L4 to S3 lumbosacral plexus derivation [6,21]. The tibial and common peroneal components divide at the lower thigh and carry cutaneous sensation from the posterior thigh and posterior and lateral aspects of the leg and foot [6,21]. Blocking this nerve hence provides adequate anaesthesia for ablation of typical varicose veins due to SPJ and posterolateral leg Perforator Vein (PV) incompetence.
Because we found limbs with inadequate anaesthesia in the leg after femoral block (in spite of injecting along the posterior border of the femoral nerve echogenic triangle), we started performing saphenous block along with femoral block for ablating varices from SFJ and anteromedial leg PV incompetence. We never had problems of inadequate numbing of the medial leg thereafter. Performing saphenous block after femoral block caused no added pain since, the skin prick to perform saphenous block was numbed by the femoral block.
Another issue we had in 22% patients undergoing GSV ablation after femoral block was persistence of cutaneous sensation in a variable strip of skin in the upper-most part of thigh below the SFJ, due to innervation by the femoroinguinal branch of the genitofemoral nerve [Table/Fig-9]. This strip of skin varied between 5 and 12 cm below the SFJ. TI of the underlying segment of GSV was performed by accessing this site through a lower puncture with long lumbar puncture needle or by forcing the tumescent solution cranially through a lower puncture by application of pressure at the site of injection [Table/Fig-4].
Schema of cutaneous innervation of anterior aspect of the upper thigh showing a strip of skin supplied by the femoral branch of the Genitofemoral Nerve (GFN) cranial to the skin innervated by the Femoral Nerve (FN), explaining the cause of persistent pain sensation in the upper thigh after femoral nerve block. Also, shown are innervation territories of Obturator Nerve (ON), Lateral Cutaneous Nerve of Thigh (LCNT) and the Subcostal Nerve (SCN).
Saphenous nerve block in isolation was used satisfactorily for laser ablation or sclerotherapy of patients with leg varices due to anteromedial leg PV incompetence in whom SFJ was competent and GSV in thigh was not dilated.
Literature search revealed four studies performed previously that reported, the use of nerve blocks for laser ablation. One of them by Osturk T et al., compared femoral block with unilateral spinal anaesthesia and reported analgesia to be similar after both procedures [16]. Two studies were prospective randomised control studies by Karim Youssef et al., (involving femoral and obturator nerve blocks) and Dzieciuchowicz et al., (involving femoral nerve block), wherein they divided their study population into two groups with one group subjected to nerve block. Both the studies found significantly lower pain scores with nerve block [5,14]. A study by Salim Yilmaz et al., involved the use of femoral and sciatic nerve blocks for laser ablation with either ambulatory phlebectomy or foam sclerotherapy and reported considerable reduction in procedural pain with preserved motor functions enabling earlier mobilization [6]. To the best of our knowledge, our study is the first to report the successful use of saphenous block for laser ablation/sclerotherapy of isolated leg varices; report, quantitate and circumvent the issue of genitofemoral cutaneous innervation to the upper thigh and to quantitate the effect of femoral nerve block on GSV diameter.
In our experience, US guided nerve blocks provided major comforts and advantages during laser ablation and foam sclerotherapy for varicose veins. They abolished or significantly attenuated procedural pain, especially the pain of tumescent injection and foam sclerotherapy. They increased the saphenous vein diameter, facilitating easy puncture and catheter navigation and eliminated chances of spasm, which the superficial veins are notorious for, thereby, decreasing procedure time. They required no additional equipment or personnel, and could be performed by the operating interventional radiologist very effectively, underpinned by their prowess at US guided interventions.
Limitation
There are a few limitations in this study which include – absence of comparison with patients treated without nerve blocks and absence of availability of data on incidence of venous spasms in patients treated without nerve blocks.
Conclusion
US guided nerve blocks for anaesthesia during minimally invasive procedures on varicose veins provide excellent procedural pain relief, enable post-procedural active mobilization, confer no additional complications, thereby, augmenting patient and operator comfort at no additional cost or equipment requirement.
GSV – great saphenous vein
SSV – short saphenous vein
PV – perforator veins
* Before and after application of techniques to circumvent the problem of un-anaesthetized upper-most anterior femoral skin.