De Garengeot’s Hernia – A Diagnostic and Therapeutic Challenge
Arun Prasath Sinraj1, Nagaraja Anekal2, Surag Kajoor Rathnakar3
1 Post Graduate, Department of General Surgery, ESIC MC and PGIMSR, Bengaluru, Karnataka, India.
2 Associate Professor, Department of General Surgery, ESIC MC and PGIMSR, Bengaluru, Karnataka, India.
3 Post Graduate, Department of General Surgery, ESIC MC and PGIMSR, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arun Prasath Sinraj, 167, Manoranjitham Street, PTR Nagar, Gandhi Nagar Post, Neyveli, Cuddalore- 607308, Tamil Nadu, India.
E-mail: drapms89@gmail.com
De Garengeot’s hernia is an eponym for femoral hernia containing vermiform appendix as its content and is named after Rene-Jacques croissant De Garengeot after he first described the condition in 1731. We present a case of a 38-year-old woman who presented with right inguinal swelling for 15 years associated with pain and vomiting for 2 days. Clinical examination revealed an irreducible femoral hernia. Emergency surgery was done and inflamed appendix was found as content of the sac. Appendectomy followed by mesh repair was done. Standard treatment protocol does not exist owing to its rarity and the outcome depends on the time of diagnosis and treatment given. A low inguinal approach is reasonable and use of polypropylene mesh warrants further study. This article is being presented because of its rarity and intends to briefly discuss the surgical pitfalls and considerations through an up-to-date literature review.
Femoral hernia, Mesh repair, Strangulation
Case Report
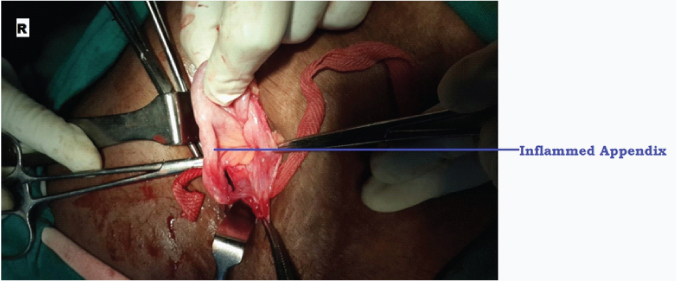
A 38-year-old woman presented with a 15 years history of swelling in right groin associated with pain and vomiting of about 5 episodes/day for past 2 days. On examination, she was afebrile, vitals were BP – 126/84 mmHg, PR–92/min, RR–16/min, SpO2- 95% in room air and found to have a tender erythematous irreducible femoral hernia. Laboratory findings including complete haemogram, Renal Function Test, Serum electrolytes, Coagulation profile, Chest radiograph were within normal limits except for leukocytosis (18000/cubicmm) with neutrophilic predominance 85%. Strangulated femoral hernia was suspected and the patient was posted for emergency surgery, hence, USG/CT abdomen was not done. On exploration via low inguinal approach, inflamed appendix was found to be the content [Table/Fig-1]. Appendicectomy was done and the femoral ring was closed by fixing polypropylene mesh to inguinal ligament anteriorly and pectineus fascia posteriorly.
Intra-operative image showing Inflamed appendix as the content of hernia.
Post-operatively, patient developed superficial surgical site infection, which was treated with appropriate intravenous antibiotics, and the patient was discharged after 10 days. Histopathological examination of appendectomy specimen was suggestive of acutely inflamed appendix with neutrophilic infiltration of muscularis propria.
Discussion
Femoral hernias account for 4% of all groin hernias with 0.5%-5% of all femoral hernias containing appendix as its content [1] and inflammed appendix within femoral hernia is even rarer, with an incidence of 0.08%-0.13% [2]. So far, fewer than 100 cases have been reported worldwide [1]. There is a strong female preponderance – female: male ratio being 13:1 reflecting the higher incidence of femoral hernia in post-menopausal women [2]. It is more common on right side. The hernia sac can contain any of the intra-abdominal contents like pre-peritoneal fat, omentum, colon, small bowel or rarely even vermiform appendix [3]. A caecal appendix secondary to intestinal malrotation or a large caecum extending into the pelvis may pre-dispose to this clinical picture; a pelvic appendix bears the highest risk of entering a femoral hernial sac [4]. Acute appendicitis in femoral hernia may be a consequence of incarceration and strangulation of the appendix by the rigid femoral neck [4].
The most common manifestation is that of a strangulated femoral hernia. Sometimes, it can present with features of small bowel obstruction or rarely even as necrotizing fasciitis. The tight neck of femoral hernia and pelvic rigidity prevents the spread of inflammation to the peritoneal cavity and hence, cardinal features of appendicitis are usually absent [5].
Differential Diagnoses include inguinal hernia, lymphoma, adnexitis, varix node, lipoma and other groin swelling. Usually, the diagnosis is made intra-operatively. Computed Tomography (CT) has low sensitivity in diagnosing appendicitis within femoral hernia with only 44% of cases that underwent pre-operative CT being diagnosed; classical findings being intramural air density in an incarcerated hernia indicating intestinal involvement [6]. Ultrasonography is not of much diagnostic use with only one case being diagnosed using USG. Our patient was not subjected to USG/CT of abdomen and pelvis to avoid any undue delay in intervention and was posted for emergency surgery.
Due to paucity of cases no standard treatment exists. Various surgical options include initial drainage followed by interval appendectomy and hernia repair in cases with advanced suppuration, appendectomy followed by interval hernia repair, appendectomy via hernia sac with femoral hernia repair at the same time. Most cases are treated with emergency appendectomy and hernia repair. Laparoscopic repair is controversial; studies have shown the use of laparoscopy and trans-abdominal pre-peritoneal repair [7,8]. There is no clear consensus on the use of mesh. If there is no evidence of infection a mesh repair may be done. Controversy exists regarding the use of prosthetic material in a contaminated field due to the risk of infection, but a few reports have mentioned mesh repair even in the presence of an inflamed appendix with no evidence of postoperative infection. The most common complication reported following De Garengeot hernia repair is wound infection, occurring in upto 29% of patients [9].
Conclusion
Despite its rarity, the surgeon should be aware of this condition and include it in the differential diagnosis of right lower quadrant pain. Imaging studies such as CT may aid the final diagnosis. Appropriate management consists of emergency appendicectomy and herniorraphy/plasty. Significantly higher rates of wound infection were noted in post-operative period and must be looked into. The role of laparoscopy is debatable and requires further study.
[1]. Talini C, Oliveira LO, Araujo ACF, Netto FACS, Westphalen AP, De Garengeot hernia: Case report and reviewInternational Journal of Surgery Case Reports 2015 8:35-37. [Google Scholar]
[2]. Piperos T, Kalles V, Al Ahwal Y, Konstantinou E, Skarpas G, Sapsakos TM, Clinical significance of de Garengeot’s hernia: A case of acute appendicitis and review of the literatureInternational Journal of Surgery Case Reports 2012 3:116-17. [Google Scholar]
[3]. Doddi S, Sagar V, Singhal T, Balakrishnan S, Smedley F, Sinha P, Femoral hernia with a twistCase Reports in Medicine 2010 2010:650829 [Google Scholar]
[4]. Hussain A, Slesser AAP, Monib S, Maalo J, Soskin M, Arbuckle J, A De Garengeot Hernia masquerading as a strangulated femoral herniaInternational Journal of Surgery Case Reports 2014 5(10):656-58. [Google Scholar]
[5]. Konofaos P, Spartalis E, Smirnis A, Kontzoglou K, Kouraklis G, De Garengeot’ s hernia in a 60-year-old woman: a case reportJournal of Medical Case Reports 2011 5:258 [Google Scholar]
[6]. Ahmed K, Bashar K, McHugh TJ, McHugh SM, Kavanagh E, Appendicitis in De Garengeot’s Hernia presenting as a nontender inguinal mass: Case report and review of the literatureCase Reports in Surgery 2014 2014:932638 [Google Scholar]
[7]. Al-Subaie S, Mustafa H, Al-Sharqawi N, Al-Haddad M, Othman F, A case of De Garengeot hernia: the feasibility of laparoscopic transabdominal preperitoneal hernia repairInternational Journal of Surgery Case Reports 2015 16:73-76. [Google Scholar]
[8]. Comman A, Gaetzschmann P, Hanner T, Behrend M, De Garengeot Hernia: transabdominal preperitoneal hernia repair and appendectomyJSLS 2007 11:496-501. [Google Scholar]
[9]. Le HD, Odom SR, Hsu A, Gupta A, Hauser CJ, A combined Richter’s and de Garengeot’s herniaInt J Surg Case Rep 2014 5(10):662-64. [Google Scholar]
[10]. D’Ambrosio N, Katz D, Hines J, Perforated appendixwithin a femoral herniaAmerican Journal of Roentgenology 2006 186(3):906-07. [Google Scholar]
[11]. Nguyen ET, Komenaka IK, Strangulated femoral hernia containing a perforated appendixCan J Surg 2004 47:68-69. [Google Scholar]
[12]. Rajan SS, Girn HR, Ainslie WG, Inflamed appendix in a femoral hernial sac: De Garengeot’s herniaHernia 2009 13(5):551-53. [Google Scholar]
[13]. Fukukura Y, Chang SD, Acute appendicitis within a femoral hernia: Multidetector CT findingsAbdom Imaging 2005 30:620-22. [Google Scholar]