High Flow AV Malformation (A-V Shunt) of Mandible: A Rare Life Threatening Entity
Sanat Kumar Bhuyan1, Krishna Gopal Birmiwal2, Indu Bhusan Kar3, Ruchi Bhuyan4, Priyanka Debta5
1 Professor and Head, Department of Oral Medicine and Radiology, Institute of Dental Sciences, SOA University, Bhubaneswar, Odisha, India.
2 Senior Resident, Department of Oral Surgery, SCB Dental College, Cuttack, Odisha, India.
3 Professor and Head, Department of Oral Surgery, SCB Dental College, Cuttack, Odisha, India.
4 Professor, Department of Oral Pathology and Microbiology, Institute of Dental Sciences, SOA University, Bhubaneswar, Odisha, India.
5 Reader, Department of Oral Pathology and Microbiology, Institute of Dental Sciences, SOA University, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sanat Kumar Bhuyan, N5/15 IRC Village, Nayapalli, Bhubaneswar-15, Odisha, India.
E-mail: drsanatkumar68@gmail.com
Intraosseous Arteriovenous Malformations (AVMs) in the head and neck region are very rare and potentially life threatening entities due to massive hemorrhage. These are the results of an embryonic abnormality of the vascular system. Depending on the blood flow and clinical presentations they are of different types like slow flow and high flow AVM. Here we present a case of high flow AVM involving mandible with a chief complain of gingival bleeding in a four year old girl child.
Girl child, Intraosseous lesion, Jaw bones, Vascular malformations
Case Report
A 4-years-old female patient reported to the Department of Oral Surgery with a complaint of swelling of lower jaw bone since three years and intermittent episodes of blood discharge from the mouth since three years.
Patient was apparently normal three years back. Her parents noticed a small swelling on the left side of the chin which gradually increased to the present size. No associated symptoms like pain, tenderness or discomfort while chewing were present. Four months back her parents consulted a private dental college where she was planned for incisional biopsy under general anaesthesia. But the biopsy could not be performed due to profuse bleeding during the procedure. Patient developed episodes of blood discharge from the mouth intermittently for which she was admitted to a private hospital several times, for the management of bleeding. In due course of time, the swelling did not subside, then after 2 years she consulted the Department of Oral and Maxillofacial Surgery and was transfused with 9 units of blood. Past medical, surgical and family history was non-significant.
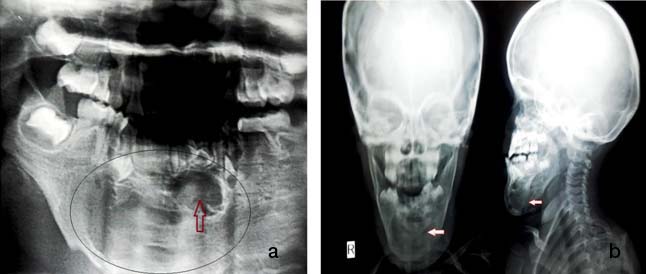
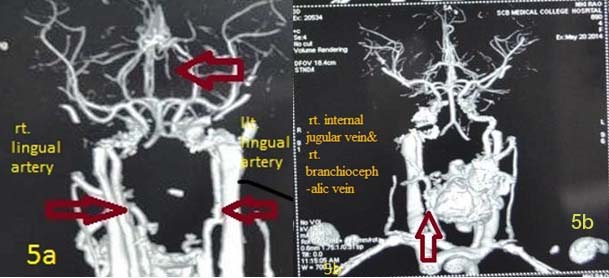
On extra-oral examination, marked facial asymmetry with swelling, around 5×4cm in dimension on anterior lower third of face extending from right parasymphysis to left parasymphysis region was seen [Table/Fig-1]. On intra-oral examination, a swelling around 5×4cm in dimension extending from tooth #73 to 84 region and extending up to the mucogingival junction and obliterating the buccal vestibule was seen. The swelling was firm and non-tender on palpation [Table/Fig-2]. Blood was examined for routine investigation and all the findings were found to be under normal limits. Orthopantomogram (OPG) and Antero-posterior (AP) view of skull suggested a radiopaque osteolytic lesion with ill defined margins on left side of mandible [Table/Fig-3]. Computed Tomography (CT) scan report suggested an expansible osteolytic lesion involving the mandible with associated soft tissue component extending to submandibular space. A provisional diagnosis of A-V malformation involving mandible was made [Table/Fig-4], CT angiogram showed intraosseous components in the mandible around mid-line and left half of mandible involving the floor of mouth. Arterial feeders were bilateral lingual artery [Table/Fig-5]. Draining veins were right internal jugular vein and right branchiocephalic vein. Thus, the final diagnosis of A-V malformation involving mandible was made.
Extra-orally marked facial asymmetry with swelling 5x4cm in size (front and lateral view).

Intra-oral swelling extending from tooth# 73 to 84.

(a) OPG; (b) Anteroposterior and lateral view (skull) revealed a radiopaque lesion with ill defined margins in the mandible.
CT scan showed expansible osteolytic lesion involving mandible with associated soft tissue component extending to submandibular area (red arrows).

CT angiogram showed intraosseous components in the mandible around midline and left half of mandible involving the floor of mouth. Arterial feeders, i.e., B/L lingual artery are shown by red arrows.
She was planned for embolization of the A-V malformation under general anaesthesia after ruling out all other causes of bleeding including bone marrow cytology. Femoral artery was identified from the groin region. A catheter was passed through the artery and dye was injected. The catheter was gently moved through the blood vessel up to the lingual artery. The branches supplying the lesion arising from lingual artery were embolized while those branches which supply tongue were secure to maintain the vascularity of tongue. The material used for embolisation was Poly Vinyl Alcohol (PVA) particles for permanent occlusion of blood vessels. Post-operatively she developed fever with multiple ecchymotic patches both extra and intra-orally. She was discharged, with stable health status, with no complaint of bleeding from oral cavity and was followed up for a year with no complaints.
Discussion
Vascular anomalies are congenital lesions of abnormal vascular development. The updated International Society for the Study of Vascular Anomalies/Biologic Classification divides vascular birthmarks into vascular tumors and vascular malformations. Vascular malformations occur in approximately 1% of births [1]. Most of congenital malformations are often misdiagnosed and left untreated [2]. The synonyms which have been used for this entity are mainly hemangioma, angioma, arterio-venous shunt, arterio-venous fistula, arterio-venous aneurysm, vascular malformation and arterio-venous malformation [3,4]. On the basis of rate of blood flow they have been divided into “slow flow” (capillary, venous, lymphatic or mixed) and “high flow” (arterial, arterio-venous fistulae or shunt) subtypes [Table/Fig-6,7] [5]. A high-flow AVM involving the mandible and surrounding soft tissue is extremely rare [6,7].
Current classification of hemangioma and vascular malformations [8,10].
| Vascular Lesions | Classification |
|---|
| Hemangioma | Superficial (capillary hemangioma)Deep (cavernous hemangioma)Compound (capillary cavernous hemangioma) |
| Vascular malformation | Simple lesionsLow-flow lesionsCapillary malformation (capillary hemangioma, port-wine stain)Venous malformation (cavernous hemangioma)Lymphatic malformation (lymphangioma, cystic hygroma)High-flow lesionsArterial malformationCombined lesionsArteriovenous malformationsLymphovenous malformationsOther combinations |
Simplified diagnostic approach for congenital vascular lesions [2,9,10].
| Hemangioma | Vascular malformations |
|---|
| Caused by failure of differentiation at early age of embryogenesis. | Caused by disturbance in late stage of angiogenesis (turnal stage). |
| Results in an embryologic abnormality of vascular system leading to proliferation of blood vessels. | Result in the persistence of AV anastomosis present during embryonic life. |
| Always congenital. | Congenital or acquired. |
| Usually extra osseous. | Usually intraosseous. |
| Usually present in childhood. | Usually present at birth although not evident clinically they may appear at different stage of life. |
| Regress or disappear in adolescence. | Do not regress. |
| Rarely associated with fatal hemorrhage. | Often cause massive or fatal hemorrhage. |
AVMs present with varied clinical presentation of age, sex and site. In the present case persistent pain and increase in size of mandibular swelling from the past three years were main complaints. Although, the lesion may be present at birth or most of the time may manifest in childhood or adolescence with peak incidence in the second decade [6]. Vascular lesions of the jaws have predilection for females with a ratio of 2:1. They are mostly seen in the skin, but may affect the visceral organs or bones; although most of the vascular lesions occur in the head and neck region but, rarely involve jaw bones. Clinically, AVM may present with minor gingival bleeding, swelling, dental loosening, paresthesia, facial deformity, malocclusion, bone resorption and sometimes hemorrhagic shock following extraction of teeth. Sometimes cases with no clinical symptoms also go undiagnosed for a long period. In the present case patient reported at very early age due to bleeding from gingiva. Systemic findings like blurred vision, epistaxsis, paresthesia and cardiac abnormalities (murmur, hypertrophy and failure) have been reported in some cases but in our case no systemic abnormality were observed [7–9].
Vascular tumors grow by cellular hyperplasia whereas; vascular malformation represents a localized defect in vascular morphogenesis. Several theories have been recommended for the pathogenesis of AVM; first is vascular stabilization (when lesion is present at birth), but in adults trauma is considered as the main cause. Defects in TGF-beta signaling, genetic two-hit hypothesis and progesterone receptors in puberty also can play a vital role in pathogenesis of AVM [10]. The hemodynamics plays an essential role in increase in size of these VMs. Areas of low vascular resistance lead to a shunting of blood with decreased perfusion of the peripheral tissue in favour of collateral flow. This causes gradual dilatation of the nutrient arteries and in turn leads to weakening of their musculo-elastic wall and diminishes the resistance. This will lead to dilatation and arterializations of the draining veins, owing to the increase in intra-luminal stress. This becomes an uninterrupted cycle and will lead to spreading out of lesion [7].
Plain radiography and CT scans have a limited role as diagnostic tools in high-flow vascular malformations. Magnetic Resonance Imaging (MRI) has become the investigation of choice because it shows the expansion of these lesions. Angiography is also most useful in poorly defined cases and mainly for embolization before surgery. It demonstrates the type of blood flow, feeder artery, and probable anastomoses. Radiographic appearance mainly include an osteolytic lesion with sunray emergence, multilocular areas with typical punched out areas, radiolucency with ill defined borders, expansion along with unilocular or multilocular cystic areas and phleboliths, root resorption and lack of lamina dura [11,12].
The radiographic differential diagnosis of AVM lesions includes ameloblastoma, ameloblastic fibroma, odontogenic myxoma, central giant cell granuloma and metastatic malignant tumours. Advanced radiological investigations are always suitable in case of similar findings like that of ameloblastoma or aneurysmal bone cyst, especially in children, before performing a biopsy or surgery, to avoid sudden bleeding, usually CT, MRI are preferred for such lesions but more recently angiography is considered as a gold standard for AVM as it can determine and locate the feeder artery and extension of lesion more precisely [11,12]. In the present case bone marrow cytology was used to rule out all other systemic causes of bleeding and CT angiogram was used to confirm the diagnosis and arterial feeders were identified as bilateral lingual artery. Draining veins were right internal jugular vein and right branchio-cephalic vein. More recently super-selective arteriography remains an essential tool in the identification of the VM and contributory vessels. This technique consists of injecting a radiopaque substance into the vascular system through a catheter near the region. The image is processed by computer, and the bone densities are subtracted for a clearer illustration of the vascular system [13].
Management of high-flow lesions depends on the depth of the vascular malformation, its anatomical site and involvement of surrounding vital areas. It is mostly managed by laser treatment and/ or embolization which provides good results. The standard treatment for AVM has been endovascular embolization with subsequent surgical removal of the lesion, but nowadays several additional treatments have been described [14]. However, other treatment modalities include Super-selective Intra-Arterial Embolization (SIAE), sclerotherapy, radiotherapy, bone wax packing of bone cavities and curettage, surgical resection, or combinations of these therapies. Various sclerosing agents like sodium morrhuate, boiling water, nitrogen mustard etc., have been used to treat high-flow lesions, but have proven to be ineffective because they were displaced from their site of action by the speed of the blood flow [15–17]. In the present case, considering the age of the patient, she was managed only by embolization of the feeder artery using PVA particles for permanent occlusion of blood vessels and was followed up for a year with no complaints. Embolization, combined with surgical treatment, is still the most conventional modern approach [18,19].
Conclusion
AVM is a rare life threatening disease. It is necessary for professionals to be aware of this type of rare lesion that can have critical complications. It is also very important to differentiate it from similar vascular lesions and diagnose it with recent advanced radiological techniques for anatomical location of the lesion and the feeder vessels of the entity in detail pre-operatively to prevent fatal consequences.
[1]. Martins F, Immordino V, Arterio-venous malformation of the base of tongue in pregnancy: Case reportActa Otorhinolaryngologica Italica 2009 29(5):274-78. [Google Scholar]
[2]. Muqtadir F, Hiremath S, Agarwal S, Gufran K, Vascular malformation of cheek: A case reportJournal of Evolution of Medical and Dental Science 2015 4(15):2617-20. [Google Scholar]
[3]. Duncan I C, Fourie PA, Vascular malformations. Part 2. Current classification of vascular-malformationsSouth African Journal of Radiology 2004 :23-30. [Google Scholar]
[4]. Kula K, Blakey G, Wright JT, Terry BC, High-flow vascular malformations: Literature re-view and case reportPediatr Dent 1996 18(4):322-27. [Google Scholar]
[5]. Spreafico R, Sordo L, Bellotto R, Schipano M, Rescaldani A, Parmigiani F Arteriovenous malformation of the mandible. Case report and review of literatureACTA Otorhino-Laryngol Ital 2016 36:333-36. [Google Scholar]
[6]. Dwivedi AND, Pandey A, Kumar I, Agarwal A, Mandibular arteriovenous malforma-tion: A rare life- threatening condition depicted on multidetector CT angiographyJOMFP 2014 (18):111-13. [Google Scholar]
[7]. Richter GT, Friedman A B, Hemangiomas and vascular malformations: Current theory and managementIntl J Pediatr 2012 2012 Article ID 645678, 10 pages [Google Scholar]
[8]. Manjunath SM, Shetty S, Moon NJ, Sharma B, Metta KK, Arteriovenous malformation of the oral cavityCase Reports in Dentistry 2014 2014 Article ID 353580, 5 pages [Google Scholar]
[9]. Singh V, Bhardwaj PK, Arteriovenous malformation of mandible: Extracorporeal curettage with immediate replantation techniqueNatl J Maxillofac Surg 2010 1(1):45-49. [Google Scholar]
[10]. Ethunandan M, Mellor T K, Haemangiomas and vascular malformations of the maxil-lofacial region-A reviewBritish Journal of Oral and Maxillofacial Surgery 2006 44:263-72. [Google Scholar]
[11]. Stafne EC, Oral Roentgenographic diagnosis 1969 3rd editionPhiladepliaW.B Saunders Company:198 [Google Scholar]
[12]. White SC, Pharoah M J, Oral Radiology Principal & Interpretations 2004 5th editionMosby Inc:449-452. [Google Scholar]
[13]. Noreau G, Landry P E, Morais D, Arteriovenous malformation of the mandible: Review of literature and case historyJ Can Dent Assoc 2001 67(11):646-51. [Google Scholar]
[14]. Amat EF, Armengol JP, Isabe Solivellas IM, Bueno JM, Padro EF, Gingival bleeding of a high-flow mandibular arterio-venous malformation in a child with 8-year follow-upCase Reports in Pediatrics 2015 2015Article ID 745718, 5 pages [Google Scholar]
[15]. Kar IB, Mishra N, Sethi AK, Mahavoi BR, Unusual case of postextraction bleedingNatl J Maxillofac Surg 2011 2(2):204-06. [Google Scholar]
[16]. Churojana A, Khumtong R, Songsaeng D, Chongkolwatana C, Suthipongchai S, Life-threatening arterio-venous malformation of the maxilla-mandibular region and treatment outcomesInterventional Neuroradiology 2012 18:49-59. [Google Scholar]
[17]. Seehra J, Horner K, Coulthard P, Arterio-venous malformation of the mandible-A case reportBritish Dental Journal 2006 201(1):25-27. [Google Scholar]
[18]. Kumaravelu C, Vasudevan R, Uma Maheswari G, Suresh Kumar P, Balaji J, Pasupathy High-flow vascular malformation of the mandibleIndian J Dent Research 2007 18(2):90 [Google Scholar]
[19]. LemoundJ J, Brachvogel P, Götz F, Rücker M, Gellrich NC, Eckardt A, Treatment of mandibular high-flow vascular malformations: Report of 2 casesJ Oral Maxillofac Surg 2011 69:1956-66. [Google Scholar]