Primary Abdominal Pregnancy: A Case Report
Sunita Dubey1, Mohit Satodiya2, Priyanka Garg3, Mamta Rani4
1 Assistant Professor, Department of Obstetrics and Gynaecology, GMCH, Sector 32, Chandigarh, India.
2 Senior Resident, Department of Obstetrics and Gynaecology, GMCH, Sector 32, Chandigarh, India.
3 Senior Resident, Department of Obstetrics and Gynaecology, GMCH, Sector 32, Chandigarh, India.
4 Senior Resident, Department of Obstetrics and Gynaecology, GMCH, Sector 32, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunita Dubey, Assistant Professor, Department of Obstetrics and Gynaecology, GMCH, Sector 32, Chandigarh-160030, India.
E-mail: sunitas504@gmail.com
Abdominal pregnancy is a potentially life threatening form of ectopic gestation with an incidence of 1% of all the ectopic pregnancies. Rarely, it may reach at advanced gestation and a viable fetal outcome is indeed a rare event. Most of them are terminated earlier due to poor fetal prognosis and higher chances of maternal mortality secondary to haemorrhagic shock following spontanous placental separation. A high index of suspicion is important for making a diagnosis of abdominal pregnancy and its timely management after correct diagnosis.
We report a case of primary abdominal pregnancy in a 30-year-old gravida 3, para 2 at 7+2 weeks of gestation. She presented with haemorrhagic shock due to spontanous separation of gestational sac from the site of implantaion. She had persisitent nausea, vomiting, diarrhoea and always had an urge to defecate which never goes off even after she defecates. She underwent termination of pregnancy by dilatation and curattage without having any antenatal ultrasound. After 72 hours of the procedure, her symptoms were aggravated and she went into haemorrhagic shock. During laparotomy haemoperitoneum of 3litres, 1kg of clots were evident and size of the uterus was about 10-12 week, bilateral tubes and ovary were healthy. A ensac fetus of 10+2 weeks along with the separated placenta was lying in the abdominal cavity. Site of implantation was identified over sigmoid colon which was not bleeding. Patient was transfused with blood and blood products. She was discharged satisfactorily on 5th postoperative day.
Hence, an Ultrasound should be done to rule out abdominal pregnancy before medical termination of pregnancy, especially in those with persistent Gastrointestinal Tract (GIT) symptoms as clinically uterus may correspond to the period of gestation in abdominal pregnancy.
Abdominal pregnancy, Adnexal mass, Ectopic Pregnancy, Haemorrhagic shock
Case Report
A 30-year-old pregnant women gravida 3, para 2 at 7+2 weeks of gestation came in the emergency section of gynaecology department with complaints of severe pain in abdomen with syncopal attack few hours back. She had a five-year-old elder child and a six-month-old younger child. Both were delivered vaginally. She was not on any contraceptive. She did not have any history of pelvic inflammatory disease. She had conceived spontaneously in the present pregnancy. Since conception she had nausea, vomitting with pain abdomen and increased frequency of defecation. She always had an urge to defecate which was persistent even after she defecates. Without undergoing any ultrasound she underwent termination of pregnancy 3 days back by dilatation and curratage based on her symptoms like nausea, vomitting and enlarged uterus which are common in pregnancy.
After 72 hours of the procedure, she had an urge to defecate which was followed by severe pain in abdomen along with loss of consciousness. Immediately she presented to our emergency ward. On examination, patient was severly pale, Pulse rate was 120/min, feeble, blood pressure was 60/40 mm of Hg. Gaurding and tenderness was present all over the abdomen. Bimanual vaginal examination revealed a 12 weeks uterine size with tenderness in adnexa. She was given intravenous fluid and started on noradrenaline infusion. Trans abdominal ultrasound revealed an empty uterine cavity and a live fetus of 10+2 weeks within the amniotic sac which was lying in peritoneal cavity on right side of uterus. There was moderate amount of free fluid in pelvis, Morrison’s pouch and paracolic gutters. Investigations revealed haemoglobin of 5gm/dl, platelets were 1.6lac/microliter and Prothrombin Index was 54%.
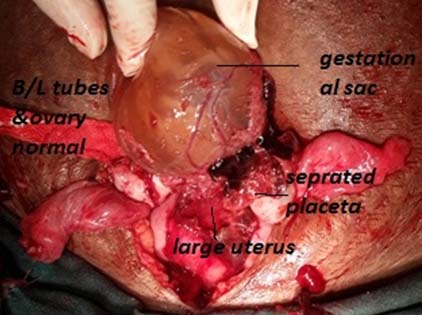
She underwent midline laparotomy under general anesthesia in view of separated abdominal pregnancy with shock. Haemoperitoneum of 3litres and 1kg of clots were evident. The fetus ensac along with separated placenta was lying freely in the peritoneal cavity and was removed [Table/Fig-1,2]. The site of placental implantaion was identified over the serosa of sigmoid colon; few tiny remnants of gestaional sac were left undisturbed. There was no bleeding from the implantation site. Uterus was 10 to 12 week size along with normal bilateral tubes and ovaries [Table/Fig-1]. There were no adhesion in the abdominal and pelvis cavity. She was transfused a total of 4units of whole blood volume and 8 units of Fresh frozen plasma along with 3liters of fluids. Noradrenaline infusion was stopped after 12 hours of surgery. Postoperative period was uneventful. She was discharged on day 5 of postoperative day.
Intraoperative fetus ensac with seprated placenta was seen in peritoneal cavity. Bilateral tubes & ovary appears normal. Uterus about 10 -12 weeks size.

Discussion
About 1- 2% of all pregnancies are ectopic pregnancies and more than 95% of them occur within the fallopian tubes [1,2]. Abdominal pregnancy is much more uncommon with an incidence of 1% of all ectopic pregnancies [3]. Abdominal pregnancy refers to a pregnancy that has implanted in the peritoneal cavity, external to the uterine cavity and fallopian tubes. The placenta can be implanted to any of the abdominal organs, pelvic vessels besides uterine wall and it can separate from the site of implantation at any time during pregnancy leading to haemorrhagic shock as in the present case.
A rare case of iatrogenic abdominal pregnancy after perforation of uterus by catheter while doing embryo tranfer has also been reported in a patient who had salpingectomy prior to In Vitro Fertilization (IVF) procedure [4]. There are reports of abdominal pregnancy occurring after hysterectomy [5]. Apart from multiparity, tubal damage secondary to pelvic inflammatory disease and endometriosis are the risk factors of abdominal pregnancy [6].
According to Studdiford’s criteria, the diagnosis of primary abdominal pregnancy is based on the following anatomic conditions: normal tubes and ovaries, absence of an uteroplacental fistula and attachment exclusively to a peritoneal surface early enough in gestation to eliminate the likelihood of secondary implantation from primary site [7]. In 1968 Friedrich EG and Rankin CA proposed that to be a true primary abdominal pregnancy the pregnancy should be less than 12 weeks of gestation and the trophoblastic attachments should be related solely to the peritoneal surface [8].
A high index of suspicion is important for making a diagnosis of abdominal pregnancy especially in those who have persistent abdominal pain, gastrointestinal disturbances, painful fetal movements, abnormal presentations, uneffaced cervix, vaginal bleeding, and syncope. Abdominal pregnancy is associated with a wide range of signs and symptoms due to variable location. As in this case symptoms were related to implantaion over gut. She did not gave history of irregular vaginal bleeding which is less frequently reported than in tubal ectopic pregnancies [9]. History of regular menstrual cycle and absence of delay in menses has been reported in a case of primary omental pregnancy who presented with severe pain in abdomen [10]. In present case ultrasound age of gestational sac was more than period of amenorrhoea.
As the diagnosis of abdominal pregnancy is often missed during routine ultrasonography. The classical ultrasound finding of abdominal pregnancy is absence of myometrial tissue between the maternal bladder and the pregnancy especially at advanced gestational age [11]. An empty uterus may be easily visualized. Other findings suggestive of the diagnosis include poor definition of the placenta, oligohydramnios and unusual fetal lie. It is difficult to differentiate it from tubal ectopic pregnancy in early gestaion when it implants in the vicinity of the adnexa. Non-contrast Magnetic Resonance Imaging (MRI) is a sensitive, specific and accurate method for evaluating ectopic pregnancy and may help in surgical planning [12]. Abnormal trends in serial Human Chorionic Gonadotropin (HCG) values seen in tubal ectopic pregnancy are usually not seen with abdominal pregnancy. Other differential diagnosis includes ectopic pregnancy in other locations, intrauterine pregnancy in a rudimentary uterine horn, abruptio placenta, and uterine rupture.
In contrast to the tubal ectopic pregnancies, primary methotrexate therapy of early gestations has high risk of failure due to the more advanced gestational age at which these pregnancies are discovered. Abdominal pregnancy at an early gestational age (first trimester), can be managed by operative laparoscopy as removal of the small and less vascular placental tissue is easier [13]. Expectant management to gain fetal maturity has been successful attempted in a few cases [14]. Very close maternal monitoring is essential in those who decide to wait for fetal maturity. In late pregnancy preoperative selective arterial embolization may be done to prevent haemorrhage during removal of large placenta [15]. Laparotomy is done as life-threatening maternal haemorrhage may occur during placental separation. Ligating the umbilical cord and leaving the placenta in situ is one option. The patient can then be followed without further intervention, or active intervention using arterial embolization or methotrexate can be instituted to hasten involution. Ultrasonographically guided feticide of a 14.5 week gestation to prevent further development and initiate the process of natural resorption has been reported [16].
The placental mass takes years to be absorbed when left at the implantation site but the levels of HCG takes few months to decline. In early postoperative period wound dehiscence may occur. Frequent follow up of patient is required for early diagnosis of inflammatory changes related to necrotic placenta including delayed haemorrhage, intestinal or ureteral obstruction, fistula involving abdominal organs, abscess formation and sepsis [17,18]. Other option which should only be done if there are no other reasonable options: to separate placenta after identification and ligation of each placental blood vessels. However, difficulty may arise when placenta implants on one or more vital organs or large blood vessels, and the normal mechanism to prevent blood loss from the placental bed (contraction of the uterus) is absent. So adequate blood, blood products should be kept ready and packing of pelvis should be done to apply pressure at the implantation site. Uncontrollable haemorrhage is the reason of maternal death, and has been reported in as many as 20 percent of cases [9]. Fetal deformations and perinatal death occur more often than maternal death [19]. Common malformations in fetus include facial and cranial asymmetry, joint abnormalities (e.g., talipes equinovarus), hypoplastic limbs and central nervous system malformations. Pregnancies with some vascular attachment to the uterus seem to be associated with a higher chance of fetal survival. Lithopedion ("stone child") may result from dead and calcified abdominal pregnancy when it goes undetected for long periods. It may causes intestinal obstruction due to adhesions, intra-abdominal abscess and fistula [20]. In most cases, the lithopedion can be identified on a plain film of the abdomen, often as an incidental finding.
Conclusion
Abdominal pregnancy should be suspected after failed induction of pregnancy in any trimester. From this case it can be inferred that symptoms like nausea, vomitting, diarrhoea along with intense persistent desire to defecate must be considered and investigated. Even when clinically size of uterus corresponds to gestational age of fetus, antenatal ultrasound should be done before medical termination of pregnancy to confirm the site of pregnancy especially when symtopms related to implantaion over bowel persist and increased over time.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
[1]. Jurkovic D, Diagnosis and management of ectopic pregnancyBritish Medical Journal 2011 342:3397 [Google Scholar]
[2]. Fylstra DL, Ectopic pregnancy not within the (distal) fallopian tube: Etiology, diagnosis, and treatmentAm J Obstet Gynecol 2012 206(4):289-99. [Google Scholar]
[3]. Nwobodo EI, Abdominal pregnancy. A case reportAnn Afr Med 2004 3(4):195-96. [Google Scholar]
[4]. Fisch B, Peled Y, Kaplan B, Zehavi S, Neri A, Abdominal pregnancy following in vitro fertilization in a patient with previous bilateral salpingectomyObstet Gynecol 1996 88:642 [Google Scholar]
[5]. Fader AN, Mansuria S, Guido RS, Wiesenfeld HC, A 14-week abdominal pregnancy after total abdominal hysterectomyObstet Gynecol 2007 109:519 [Google Scholar]
[6]. Maas DA, Slabber CF, Diagnosis and treatment of advanced extra-uterine pregnancyS Afr Med J 1975 49:2007-10. [Google Scholar]
[7]. Studdiford WE, Primary peritoneal pregnancyAm J Obstet Gynecol 1942 44:487-91. [Google Scholar]
[8]. Friedrich EG, Rankin CA, Primary pelvic peritoneal pregnancyObstet Gynecol 1968 31:649-53. [Google Scholar]
[9]. Rahman MS, Al-Suleiman SA, Rahman J, Al-Sibai MH, Advanced abdominal pregnancy—observations in 10 casesObstet Gynecol 1982 59:366 [Google Scholar]
[10]. Onan MA, Turp AB, Saltik A, Akyurek N, Taskiran C, Himmetoglu O, Primary omental pregnancy: Case report Human Reproduction 2005 20(3):807-09. [Google Scholar]
[11]. Varma R, Mascarenhas L, James D, Successful outcome of advanced abdominal pregnancy with exclusive omental insertionUltrasound Obstet Gynecol 2003 21:192 [Google Scholar]
[12]. Lockhat F, Corr P, Ramphal S, Moodley J, The value of magnetic resonance imaging in the diagnosis and management of extra-uterine abdominal pregnancyClin Radiol 2006 61:264 [Google Scholar]
[13]. Gerli S, Rossetti D, Baiocchi G, Clerici G, Unfer V, Di Renzo GC, Early ultrasonographic diagnosis and laparoscopic treatment of abdominal pregnancyEur J Obstet Gynecol Reprod Biol 2004 113(1):103-05. [Google Scholar]
[14]. Beddock R, Naepels P, Gondry C, Besserve P, Camier B, Boulanger JC, Diagnosis and current concepts of management of advanced abdominal pregnancyGynecol Obstet Fertil 2004 32:55-61. [Google Scholar]
[15]. Cardosi RJ, Nackley AC, Londono J, Hoffman MS, Embolization for advanced abdominal pregnancy with a retained placenta. A case reportJ Reprod Med 2002 47:861 [Google Scholar]
[16]. Mitra AG, LeQuire MH, Minimally invasive management of 14.5-week abdominal pregnancy without laparotomy: A novel approach using percutaneous sonographically guided feticide and systemic methotrexateJ Ultrasound Med 2003 22:709 [Google Scholar]
[17]. Nkusu Nunyalulendho D, Einterz EM, Advanced abdominal pregnancy: Case report and review of 163 cases reported since 1946Rural Remote Health 2008 8(4):1087 [Google Scholar]
[18]. Cetinkaya MB, Kokcu A, Alper T, Follow up of the regression of the placenta left in situ in an advanced abdominal pregnancy using the Cavalieri methodJ Obstet Gynaecol Res 2005 31:22 [Google Scholar]
[19]. Stevens CA, Malformations and deformations in abdominal pregnancyAm J Med Genet 1993 47:1189-95. [Google Scholar]
[20]. Odom SR, Gemer M, Muyco AP, Lithopedion presenting as intra-abdominal abscess and fecal fistula: Report of a case and review of the literatureAm Surg 2006 72:77-8. [Google Scholar]