Inflammatory Myofibroblastic Tumor of the Kidney: A Rare Renal Tumor
Alvin Jose Pothadiyil1, Suresh Bhat2, Fredrick Paul3, Jithesh Mampatta4, Mahesh Srinivas5
1 Senior Resident, Department of Urology, Goverment Medical College, Kottayam, Kerala, India.
2 Professor, Department of Urology, Goverment Medical College, Kottayam, Kerala, India.
3 Associate Professor, Department of Urology, Goverment Medical College, Kottayam, Kerala, India.
4 Senior Resident, Department of Urology, Goverment Medical College, Kottayam, Kerala, India.
5 Senior Resident, Department of Urology, Goverment Medical College, Kottayam, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suresh Bhat, Professor, Department of Urology, Goverment Medical College, Kottayam-686008, Kerala, India.
E-mail: drsureshbhat@yahoo.com
Inflammatory Myofibroblastic Tumour (IMT) or ‘pseudotumour’ of the kidney is a rare benign tumour of unknown aetiology affecting mostly young adults. A subset of IMT is neoplastic and harbours translocations of activin receptor-like kinase-1 (ALK-1) gene and can recur or rarely metastasize. Presentation varies from an incidentaloma to gross haematuria. Clinical examination and radiological investigations are usually inconclusive. Often, biopsy is inconclusive necessitating a management similar to that of Renal Cell Cancer (RCC). Diagnosis is based on immunohistochemistry. We are reporting a case of IMT in a 50-year-old male patient who presented with left flank mass which on evaluation was suggestive of left renal cell carcinoma. Excision of the tumour, histopathological examination and Immunohistochemistry proved the tumour to be IMT.
Inflammation, Neoplasm, Nephrectomy, Pseudotumour
Case Report
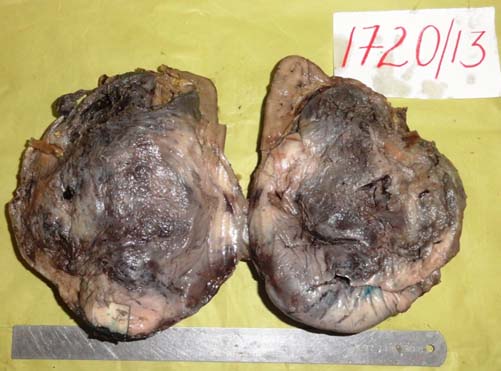
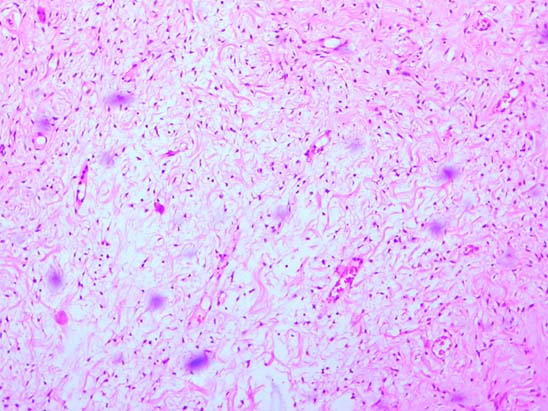
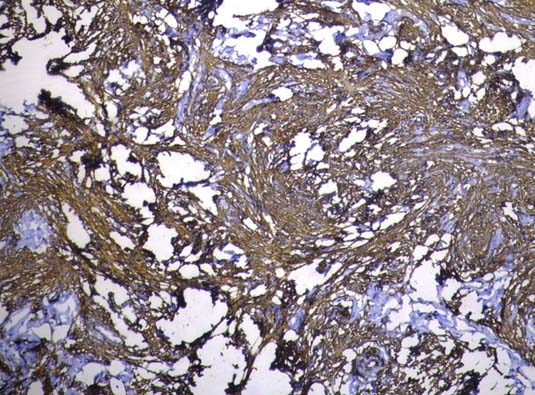
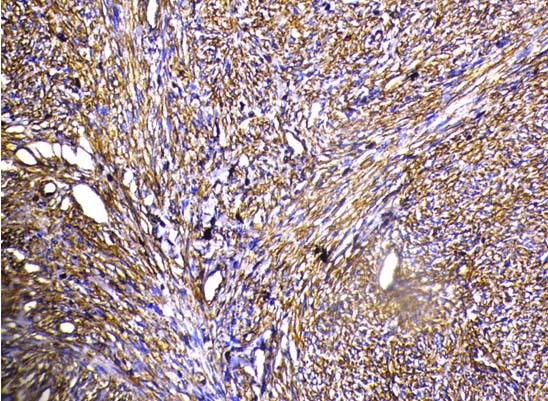
A 50-year-old male reported with left flank pain of two months duration. Physical examination revealed a large mass in the left loin. Routine investigations were normal. Ultrasonography and computerized tomographic imaging showed a large mass arising from the left kidney. Clinically, the stage was T3N0M0. Radical nephrectomy was done considering a diagnosis of Renal Cell Carcinoma (RCC). On cut section, the tumour was circumscribed, and unencapsulated with a tan, fleshy, myxoid surface [Table/Fig-1]. Histologically, the tumour consisted of proliferating spindle cells in an oedematous myxoid background with abundant blood vessels mixed with various amounts of lymphocytes and plasma cells [Table/Fig-2]. On immunohistochemistry (IHC) the tumour was positive for vimentin and SMA [Table/Fig-3,4] and negative for cytokeratin, HMB45, S-100, C-kit, CD31, CD34 and desmin. Thus, the diagnosis of IMT was confirmed. At 2 years follow-up, the patient remained recurrence free.
Cut section showing circumscribed, unencapsulated tumour with a tan and myxoid appearance.
H&E stain showing spindle cells admixed with lympho plasmacytic infiltration in a loose fibro myxoid background. (10 X).
Immuno histochemical staining showing strong SMA positivity. (10X).
Immuno histochemical staining showing strong vimentin positivity. (10X).
Discussion
Inflammatory Myofibroblastic Tumour (IMT) is a very rare tumour affecting young people, males (58%) more than females. The age at presentation varies from 3 to 89 years. Inflammatory pseudotumours are common in lungs and orbit. In the urinary tract, IMT is common in the bladder. In the kidney, so far 39 cases have been reported. The first IMT of the kidney was reported in 1972 by Davides et al., as plasma cell granuloma [1].
IMT has various synonyms like inflammatory pseudotumour, plasma cell granuloma, inflammatory myofibrohistiocytic proliferation, pseudosarcomatous myofibroblastic proliferation and xanthomatous pseudotumour. This confusion in nomenclature is due to confusion regarding its origin that whether it is a reactive process or a true neoplasm. Inflammatory reactions to surgery, trauma, irritation and infection are some of the etiological factors. Infections due to Epstein-Barr virus and herpes virus are also considered as causative factors. Translocation of chromosome band 2p23 involving ALK receptor tyrosine kinase gene suggest a neoplastic origin [2,3].
Patients usually present with abdominal pain (38%), haematuria (28%), constitutional symptoms (23%) and occasionally a mass. In 36%, these tumours are detected incidentally. A clinical or radiological diagnosis as well as pre-operative exclusion of malignancy is difficult. The radiological features of IMT are variable and non-specific possibly because of the amount of fibrosis and cellular infiltrate. Diagnosis is usually made at surgical intervention. On occasions (15%), sufficient material on trucut biopsy proved the diagnosis and these patients responded to corticosteroids [4]. Majority (33/39 patients) underwent partial or radical nephrectomy. One case of spontaneous regression on follow-up has been reported implicating inflammatory aetiology [5]. A case of IMT enclosing renal cell cancer has also been reported warranting a cautious approach to this entity [6].
Histologically, the tumour consists of proliferating spindle cells in an oedematous myxoid background with abundant blood vessels mixed with various amounts of lymphocytes, plasma cells. The spindle cells express vimentin and smooth muscle actin. They are strongly positive for CD34. ALK is positive in 50% cases. In our case also the tumour was strongly positive for vimentin and smooth muscle actin and was negative for desmin and cytokeratin. Pseudotumours generally lack severe cytological atypia and have less mitosis than sarcomas and also tend to be negative for p53 which is positive in sarcoma. The architecture of these tumours has been described as ‘pattern less pattern’. Histologically, three patterns have been described including a myxoid vascular pattern, a compact spindle cell pattern, and a hypo cellular fibrous pattern (nodular fasciitis like, fibrous histiocytoma like and a desmoid or scar tissue). Dystrophic calcification and osseous metaplasia are occasionally seen. Necrosis is uncommon. The differential diagnosis includes renal cell carcinoma, sarcomatoid RCC, leiomyosarcoma, rhabdomyosarcoma, neurogenic tumours, angiomyolipoma, and xanthogranulomatous pyelonephritis [7]. The immunohistochemistry helps to distinguish these in some of the cases. S-100 will be positive in neurogenic tumours; myogenin and Myo D1 in rhabdomyosarcoma and Pan cytokeratin in renal cell carcinoma. The diagnosis of inflammatory myofibroblastic tumour requires a correlation of both morphological and Immuno-histochemical features. Angiomyolipoma of the kidney is diagnosed by fat containing (-15 to -85 HU) mass on CT scan. Xantho granulomatous pyelonephritis on CT scan classically shows “bear paw sign”. The CT scan usually shows a calculus in the renal pelvis surrounded by dilated calyces. The kidney is usually poorly functioning.
Inflammatory myofibroblastic tumours are considered to be of low malignant potential and low incidence of local recurrence. Recurrence has been reported when the tumour is of large size, abdominopelvic location, and occurring in elderly. Metastasis was reported in younger patients, large size tumours and abdominopelvic location [8]. No recurrence has been reported in IMT of the kidney. our case is this elderly patient presented without classical symptoms of hematuria and abdominal pain which is uncommon.
Conclusion
In conclusion, patients presenting with renal mass, haematuria and loin pain need detailed evaluation with various imaging modalities like Ultrasonography, CT scan and MRI. Rare tumours like IMT do not have any specific imaging features indicative of a definite diagnosis. In these patients, a pre-operative biopsy of the tumour has a role. This will help in pre-operative planning of the surgical modality to be chosen like radical nephrectomy or partial nephrectomy. Benign tumours like IMT if are diagnosed pre-operatively can be managed by conservatively. This will help in preventing long term morbidities associated with radical ablative surgery.
[1]. Davides KC, Johnson SH, Marshall M, Price SE, Stavrides A, Plasma cell granuloma of the renal pelvisJ Urol 1972 107(6):938-39. [Google Scholar]
[2]. Gleason BC, Hornick JL, Inflammatory myofibroblastic tumours: Where are we now?J Clin Pathol 2008 61:428-37. [Google Scholar]
[3]. Lawrence B, Perez-Atayde A, Hibbard MK, Rubin BP, Dal Cin P, Pinkus JL, TPM3-ALK and TPM4-ALK oncogenes in inflammatory myofibroblastic tumoursAm J Pathol 2000 157:377-84. [Google Scholar]
[4]. Ma Y, Zieske AW, Fenves AZ, Bilateral infiltrating renal inflammatory pseudotumour responsive to corticosteroid therapyAm J Kidney Dis 2008 51:116-20. [Google Scholar]
[5]. Marshall J, Lin EP, Bhatt S, Dogra VS, Inflammatory Pseudotumour of the KidneyJ Ultrasound Med 2008 27:803-07. [Google Scholar]
[6]. Gwynn ES, Clark PE, Inflammatory myofibroblastic tumour associated with renal cell carcinomaUrology 2005 66:880-81. [Google Scholar]
[7]. Selvan DR, Philip J, Manikandan R, Helliwell TR, Lamb GH, Desmond AD, Inflammatory pseudotumour of the KidneyWorld J Surg Oncol 2007 5:106 [Google Scholar]
[8]. Lee NG, Alexander MP, Huihong Xu, Wang DS, Renal Inflammatory Myofibroblastic Tumour: A Case Report and Comprehensive Review of LiteratureWorld journal of oncology 2011 2:85-88. [Google Scholar]