The term “autopsy” is derived from the Ancient Greek word autopsia, means “to see for oneself ”, autos (“oneself ”) and opsis (“eye”) [1,2]. A handful of histopathological findings unrelated to the cause of death are noticed in routine histopathological examination of medicolegal autopsies. These findings have proved to be of great academic value and serve as an eye opener to the infrequent lesions which go unnoticed when a person is alive. The medicolegal autopsy provides an opportunity for studying not only medically diagnosed and treated neoplasms, but also the natural evolution of untreated disease [3]. Autopsy also aids in the diagnosis of undiagnosed or misdiagnosed malignant tumours irrespective of underlying cause of death, which may or may not be related to malignancy [4]. But many incidental findings have been highlighted on histopathological examinations which have proven to be great learning tools for the pathologists as well as the forensic expert. Histopathological examination is also important for assessing statistics of mortality which are essential for public health and health service planning [5].
Materials and Methods
A retrospective descriptive study of medicolegal autopsies for five years from 2008-2013 was conducted in the Department of Pathology, a Medical College attached tertiary care center. A total number of 269 cases were sent for histopathological examination out of which 202 cases were included in our study, where the internal organs were sent and 67 cases (hanging, electrocution and burns) were excluded, in which skin was sent for histopathologic examination. The organs relevant to the case concerned were sent in 10% formalin. In most of the cases they comprised of heart, liver, spleen, kidneys, brain and lungs. Representative bits from the concerned organs were processed in a routine manner. All sections were stained with Haematoxylin and Eosin (H & E) stain and special stains were used, as and when required. Gross and histopathologic findings were noted and the salient features were studied.
Results
The present study consisted of a series of 269 autopsy cases from JSS Hospital, Mysuru, India conducted over a period of five years. The internal organs of total of 202 autopsies were sent for histopathological examination. [Table/Fig-1] displays the spectrum of lesions noted at autopsy. The remainder consisted of 60 cases of hanging, 5 cases of electrocution and 2 cases of burns.
Spectrum of lesions noted at autopsy.
| Sl. No. | Histopathological finding | No of cases |
|---|
| 1 | Atherosclerosis | 55 |
| 2 | Fatty liver | 40 |
| 3 | Pulmonary oedema | 25 |
| 4 | Acute Tubular Necrosis (ATN) | 22 |
| 5 | Pneumonia | 7 |
| 6 | Tuberculosis | 7 |
| 7 | Cirrhosis | 6 |
| 8 | Neoplastic lesions | 5 |
| 9 | Infarction intestine | 3 |
| 10 | Erosive gastritis | 3 |
| 11 | Pancreatitis | 2 |
| 12 | Meningitis | 2 |
| 13 | Uterus-leiomyoma | 2 |
| 14 | Chronic venous congestion spleen | 1 |
| 15 | Other incidental findings | 6 |
| 16 | Autolysed | 16 |
| Total | 202 |
Out of the total 202 cases, 121 (60.0%) were males and 81 (40.0%) were females. The majority (48.5%) of cases were between 21-40 years, constituting 98 of the total cases as stated in [Table/Fig-2]. The commonest cause of death was pulmonary oedema.
Age distribution of autopsy cases.
| Age group | No of cases |
|---|
| 0-20 | 5(2.5%) |
| 21-40 | 98(48.5%) |
| 41-60 | 80(39.6%) |
| 61-80 | 12(5.9%) |
| >80 | 7 (3.5%) |
| Total | 202 |
The most common incidental histopathologic finding noted was atherosclerosis of the aorta and coronary vessels in 55(27.2%) cases followed by fatty liver in 40 (19.8%) cases.
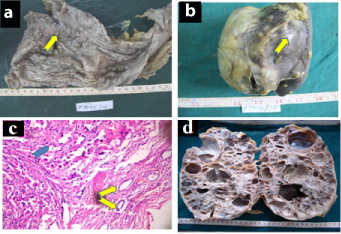
The incidental renal masses in the study comprised of oncocytoma, adult polycystic disease of kidney, multilocular cystic renal cell carcinoma and clear cell Renal Cell Carcinoma (RCC) with coexistent pulmonary tuberculosis and hepatic cirrhosis. The incidentally discovered oncocytoma was a rare case of tumour to tumour metastasis in a 68-year-old male, with history of snake bite. The patient had nodular lesions of adenocarcinoma in the stomach [Table/Fig-3a] metastasising into oncocytoma of kidney [Table/Fig-3b] confirmed by histopathology [Table/Fig-3c] and immunohistochemistry. A case of Autosomal Dominant Polycystic Kidney Disease (ADPKD) was identified in the post mortem examination of a 45-year-old male after death from road traffic accident who was asymptomatic during his life [Table/Fig-3d]. The case of Multilocular Cystic Renal Cell Carcinoma (MCRCC) was identified in a 38 year old male autopsied after alleged consumption of organophosphorus compound. The right kidney showed an expansile lesion comprising of multiple thick gelatinous fluid filled cysts and septa surrounded by fibrous pseudocapsule [Table/Fig-4a] and on microscopy, cysts of varying sizes were seen separated by intervening septae, lined by aggregates of epithelial cells with clear cytoplasm characteristic of MCRCC [Table/Fig-4b]. Clear cell RCC [Table/Fig-4c] was incidentally detected in a 40-year-old male after death from massive haemoptysis where the lungs showed cavitatory lesions with caseating granulomas and Langhans giant cells diagnostic of pulmonary tuberculosis and liver was nodular displaying cirrhotic parenchymal nodules with bridging septae.
a) Cut open stomach showing thickening of wall with grey white nodular lesions (arrow)-Adenocarcinoma of Stomach. b) Outer surface of right kidney showing a single nodule (arrow)-Oncocytoma. c) Oncocytoma (arrow head) of Kidney with metastatic deposits from adenocarcinoma of stomach (arrows). (H&E, x200). d) Cut surface of right kidney showing multiple cysts of varying sizes-Autosomal Dominant Polycystic Kidney Disease.
a) Cut surface of right kidney displaying expansile gelatinous fluid filled cystic lesion -Multilocular Cystic Renal Cell Carcinoma. b) Multilocular cystic Renal Cell Carcinoma (MCRCC) showing multiple cysts with septae lined by clear cells (arrow). (H&E, x200). c) Clear cell Renal Cell Carcinoma (RCC) displaying nests of tumor cells. (H&E, x200). d) Hepatocytes with cytoplasmic vacuolation and brown pigment-Dubin Johnson syndrome. (H&E, x100).
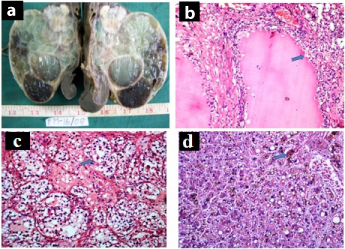
Liver being a predominant organ sent for histopathologic study, a total number of 52 liver lesions were discovered, 40 showed fatty change constituting 19.8% of cases, with 6 (3%) cases of cirrhosis and a spectrum of fortuitous findings comprising of Dubin Johnson syndrome, bile duct hamartoma Von Meyenburg Complex (VMC), large bile duct obstruction, carcinoid tumour of liver and amoebic liver abscess. Dubin Johnson Syndrome was diagnosed postmortem in a 25-year-old male after death from hanging. Pieces of liver with blackish discoloration displayed hepatocytes with abundant grey brown cytoplasmic pigment along with grade 1 micro and macrovesicular steatosis [Table/Fig-4d]. The pigment was not stained with Perl’s Prussian Blue while Masson Fontana stain confirmed the brown granular pigment in hepatocytes [Table/Fig-5a]. A case of subcapsular bile duct hamartomas (VMC) was found in a patient aged 40 years [Table/Fig-5b].
a) Hepatocytes with brown pigment. (Masson Fontana, x100). b) Expanded portal tract with proliferating bile ductule-von Meyenburg complex. (H&E, x100). c) Liver displaying perivenular bilirubinostasis with portal tract edema, inflammation and bile duct proliferation- Large bile duct obstruction (H&E, x100). d) Specimen of liver showing multiple grey white nodules-Metastatic Carcinoid.
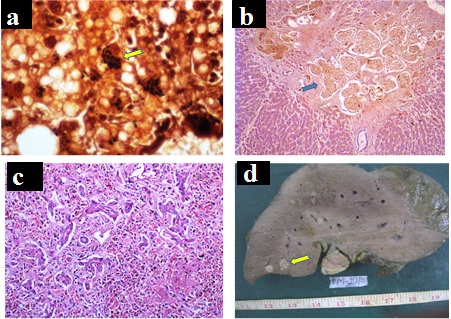
The changes in hepatic architecture secondary to large bile duct obstruction were noted in a 30-year-old male after suicidal death from poison consumption, who had a past clinical history of recurrent jaundice and microscopy revealed bile duct proliferation with perivenular bilirubinostasis accompanied by portal tract oedema and inflammation, suggestive of changes due to large bile duct obstruction [Table/Fig-5c]. Among the neoplastic lesions of liver, a case of carcinoid tumour was diagnosed in a specimen of liver displaying multiple grey white nodules, largest measuring 2x1.8cm, suggestive of metastatic deposits [Table/Fig-5d]. Microscopy of the same revealed carcinoid tumour [Table/Fig-6a]. Among the inflammatory conditions, an undiagnosed abscess showed multiple trophozoites of Entamoeba histolytica in a friable specimen of liver with dark coloured pus [Table/Fig-6b].
a) Hepatic carcinoid displaying nests and trabeculae of tumor cells. (H&E, x100). b) Trophozoites of Entamoeba histolytica having abundant cytoplasm, central round nuclei with karyosome. (H&E, x200). c) Liver displaying epithelioid granuloma with Langhan’s giant cell and fatty change.(H&E, x100). d) Hepatic sinusoids filled with sickled rbc’s. (H&E, x400).
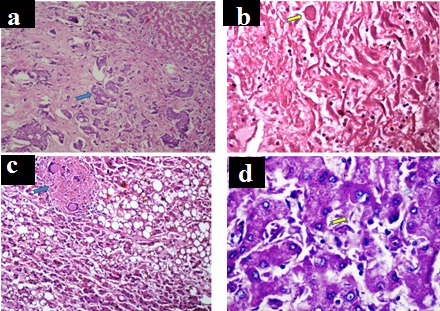
Three cases (1.48%) of tubercular lesions unrelated to the cause of death were discovered, although our study had a total of seven cases (3.46%) of pulmonary tuberculosis. Tubercular lesions in lungs were seen in two patients with one of them having extra-pulmonary involvement of liver with coexistent fatty change [Table/Fig-6c], whereas the third case was that of the triple lesion mentioned above comprising of pulmonary tuberculosis with micronodular cirrhosis and clear cell RCC.
A postmortem diagnosis of Sickle cell anaemia was made in a 23-year-old male who died in road traffic accident. The patient had intra-cerebral bleed, collapsed lungs and haemorrhagic contusion of liver, where the cause of death was attributed to cardio-respiratory arrest. On histopathology, multiple sections from lung showed macrophages and blood vessels filled with sickled erythrocytes with areas of consolidation, liver displayed congested sinusoids filled with sickled erythrocytes [Table/Fig-6d] and brain had large areas of oedema displaying congested cerebral blood vessels packed with sickled erythrocytes.
Among the incidental and interesting findings noted in our study, neoplastic lesions accounted for 5(2.47%) of cases, comprising of the above mentioned cases of RCC, tumour to tumour metastasis- adenocarcinoma of stomach with metastasis to oncocytoma of kidney, carcinoid of liver and a case of follicular adenoma of thyroid [Table/Fig-7].
Incidental findings in autopsy.
| Sl.No. | Age/Sex | History / indication of autopsy | Histopathological findings |
|---|
| 1 | 68/M | Snake bite | Tumour to tumour metastases –gastric adenocarcinoma metastasising into oncocytoma of kidney |
| 2 | 40/M | Massive haematemesis | Lungs-Tuberculosis, Kidney-Clear cell RCC, Liver-cirrhosis |
| 3 | 38/M | OP poisoning | Kidney-MCRCC |
| 4 | 45/M | RTA | ADPKD |
| 5 | 25/M | Hanging | Dubin-Johnson Syndrome |
| 6 | 40/M | RTA | Bile duct hamartoma |
| 7 | 30/M | Poisoning | Large bile duct obstruction |
| 8 | 35/M | RTA | Liver-carcinoid |
| 9 | 45/F | RTA | Amebic liver abscess |
| 10 | 52/M | Massive haemoptysis | Lungs-Tuberculosis |
| 11 | 39/M | RTA | Lungs-Tuberculosis Liver- Tuberculosis with fatty change |
| 12 | 23/M | RTA | Sickle cell anaemia with vaso-occlusive crisis |
| 13 | 38/F | Unidentified body | Thyroid-follicular adenoma |
Abbreviations used: RCC-renal cell carcinoma, MCRCC-multilocular cystic renal cell carcinoma, OP-organophosphate, RTA-road traffic accident, ADPKD-autosomal dominant polycystic kidney disease
Discussion
Our study revealed 4 incidental renal masses accounting for 1.98% of the histopathological findings. In a study of 650 cases of autopsy by Shah VB et al., 5 cases of renal masses were detected incidentally (less than 1%), which included MCRCC [6]. Incidence of MCRCC is rarely reported in literature. These cases were asymptomatic and had no symptoms related to the masses and the causes of death were unrelated to the renal masses [6]. In a study of incidental RCC, 110 tumours were diagnosed at autopsy with a rate of 7.1/1000 autopsies [7]. We encountered 2 cases of incidental renal cell carcinomas with a rate of 2/269 autopsies. ADPKD, the most common hereditary kidney disorder, affects approximately 1/1000 living people with an incidence of 1:500 in autopsy series [8]. whereas an incidence of 1:269 was seen in our series.
The case of adenocarcinoma of stomach metastatic to oncocytoma of kidney was a rare finding with less than 100 cases being reported in the English literature [9]. Metastasis of one neoplasm to another is known as metastasis of “cancer to cancer” or “tumour in tumour” and is quite rare, being first documented in 1902 [10,11]. The commonest donor sites being lung followed by breast, prostate, thyroid and gastrointestinal tract cancers [9]. The commonest recipient is RCC of kidney followed by sarcomas, meningiomas, thyroid and pituitary adenomas. Other tumours of kidney such as angiomyolipomas and renal oncocytomas have also been described as recipients as in our case [7]. A set of criteria were described by Campbell et al., for the diagnosis of tumour to tumour metastasis: a) more than one primary tumour must exist; b) the recipient tumour must be a true neoplasm (benign or malignant); c) the metastatic neoplasm must be a true metastasis with established growth in the host tumour and not a collision tumour (the result of contiguous growth); and d) neoplasms which have metastasized to the lymphatic system where lymhoreticular tumours already exist are excluded [9].
Quite rightly liver is called as custodian of milieu interior” and is vulnerable to a variety of metabolic, toxic, microbial and circulatory insults [12]. Hence, liver is sent in almost all cases of autopsies to ascertain the cause of death. Most of the chronic liver diseases even in advanced stages may cause no prominent clinical signs and symptoms and are diagnosed only during autopsy [12,13]. The spectrum of lesions that are reported in a series of autopsy findings of liver have reported fatty change, Chronic Venous Congestion (CVC), cirrhosis of liver, malignancy, hepatitis and chronic abscess, fatty change being the predominant finding [14].
Another, autopsy study of fifty cases of liver specimens reported fatty change, chronic venous congestion (CVC), cirrhosis of liver, neoplasm and hepatitis with CVC being the predominant finding [15]. The findings in our study are comparable to these studies with fatty liver being the commonest lesion in both studies. In most of the cases of Dubin Johnson syndrome, patients have asymptomatic hyperbilirubinemia with well preserved hepatic functions. Although patients were present with hyperbilirubinemia or cholelithiasis, our patient had an asymptomatic course which was undiagnosed before death [16]. Bile duct hamartomas of the liver are usually detected at laparotomy or autopsy as an incidental finding as in our study and are usually multiple [17,18]. Carcinoids being the most common gastrointestinal endocrine tumours, metastases frequently involve liver. Primary hepatic carcinoids are solitary in contrast to metastatic carcinoids [19]. Most hepatic carcinoids are metastatic rather than primary with multiple nodules in the liver similar to our case [19,20]. The importance of histopathology in autopsy studies cannot be under emphasised in understanding the disease processes involving liver.
Tuberculosis (TB) has been described as a ‘global emergency’ by WHO and is still considered as a major cause of morbidity and mortality worldwide [21]. Our study encountered 3.46% cases of tuberculosis with all the cases having pulmonary involvement and one having extrapulmonary involvement. The incidence of tuberculosis is much lower in our study as compared to a study by Garg M et al., where, active tuberculosis were found in 8.7%, of which 90% suffered from pulmonary tuberculosis, 10% had military tuberculosis and 30% manifested with extra-pulmonary tuberculosis. The most frequently affected organ was lung similar to our study [22]. The diagnosis of tuberculosis was incidental in three of our cases with postmortem diagnosis of tuberculosis. The probable explanation for this would be that latent infection is common in tuberculosis with 10% of it eventually progressing to active disease. Many cases of tuberculosis remain undiagnosed and are diagnosed only at autopsy [23]. In a study of 73 cases of sudden deaths, by Rastogi P, forty five cases (61.64%) were specifically assigned to tuberculosis [21]. Our study has revealed the importance of histopathology in autopsy towards the study of actual disease prevalence of tuberculosis.
The clinical profile of sickle cell patients is reported to be less severe in India compared to that of African countries and is characterized by delayed presentation, pauci symptomatic cases, less frequency of vaso occlusive crisis and low mortality. Therefore, most of the patients remain undiagnosed as in our case [24]. The strongest factor in SCT (sickle cell trait) patients implicating intravascular sickling with tissue injury and even death is hypoxia leading to intravascular sickling [24–27]. In our case, the road traffic accident with resultant bleeding leading to hypoxia probably triggered intra-vascular sickling and vaso-occlusive crisis contributing to the catastrophic events leading to death.
The overall incidence of unsuspected neoplasia in our study was 2% (4 per 202 autopsies) which is somewhat lower as compared to other studies by Burton EC with a detection rate of 9% (100 per 1105 autopsies) malignant neoplasms and Sens et al., with an incidence of 7% unexpected cancer in forensic autopsies [4,28]. The types of neoplasms in this study were similar to those seen in other postmortem studies but with a lower incidence [5]. Histopathologic study in autopsies is invaluable in the detection of these unsuspected neoplasms and evaluating the cause of death, also aiding to the true cancer incidence statistics.
Limitation
The present study has not stressed on the common lesions because the aim was to highlight interesting and incidental findings. It would have better if lesions involving individual system were studied separately.
Conclusion
From our study we conclude that atherosclerosis was the commonest histopathologic finding followed by fatty liver. Histopathology in autopsy plays a vital role in the study of some of the rare neoplastic lesions contributing to the knowledge of pathology. This study highlights the various incidental unexpected rare cases in medico-legal autopsies, which are imperative in academic and research purposes. Histopathology would not have been necessary for some of these conditions during a life time but an incidental finding in autopsy has unveiled the histo-pathological changes that help in the understanding of disease processes which are otherwise rare for a pathologist to encounter in the day to day specimens. Such retrospective and prospective studies also provide an insight into the true prevalence of diseases or lesions.
Abbreviations used: RCC-renal cell carcinoma, MCRCC-multilocular cystic renal cell carcinoma, OP-organophosphate, RTA-road traffic accident, ADPKD-autosomal dominant polycystic kidney disease