Pleural Mesothelioma with No Asbestos Exposure: A Case Report
Salma Ait Batahar1, Othmane Ouradi2, Safae Elidrissi3, Lamyae Amro4
1 Medicine Doctor, Department of Pulmology, Mohamed VI University Hospital, Morocco.
2 Medicine Doctor, Department of Pulmology, Mohamed VI University Hospital, Morocco.
3 Medicine Doctor, Department of Pulmology, Mohamed VI University Hospital, Morocco.
4 Medicine Doctor, Department of Pulmology, Mohamed VI University Hospital, Morocco.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Salma Ait Batahar, 848, LOE Almassar, Route de Safi, Marrakech-40000, Morocco.
E-mail: aitbatahar@yahoo.fr
Malignant Pleural Mesothelioma (MPM) is the primary malignant tumour of the pleura. It is highly aggressive and linked to the exposure to asbestos fibers. The prognosis of this cancer is bad with a median of survival around 12 months. The diagnosis of pleural mesothelioma is often done at an advanced stage of the disease because of the lack of specific clinical and radiological signs differentiating it from any malignant pleural effusion. The absence of an explicit asbestos exposure is another diagnosis problem. We report the case of a 60-year-old patient without any prior exposure to asbestos who presented for pleural effusion and a nodular thickening of the pleura on the CT scan. The diagnosis of MPM was confirmed after pathology study of the biopsies obtained by video assisted thoracoscopy.
Diagnosis, Malignancy, Pleural effusion
Case Report
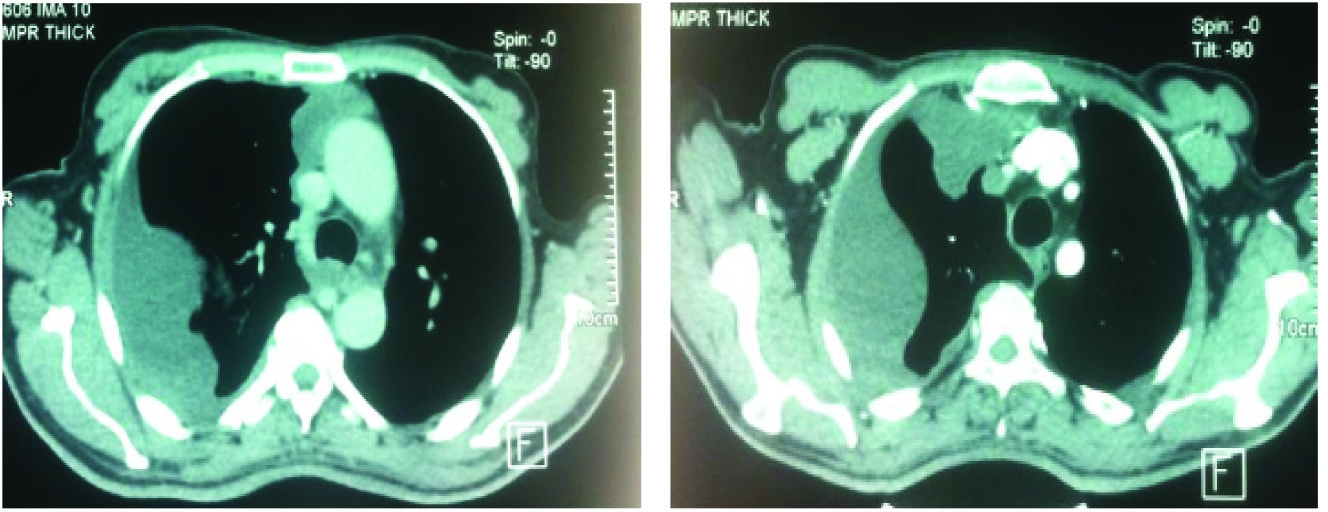
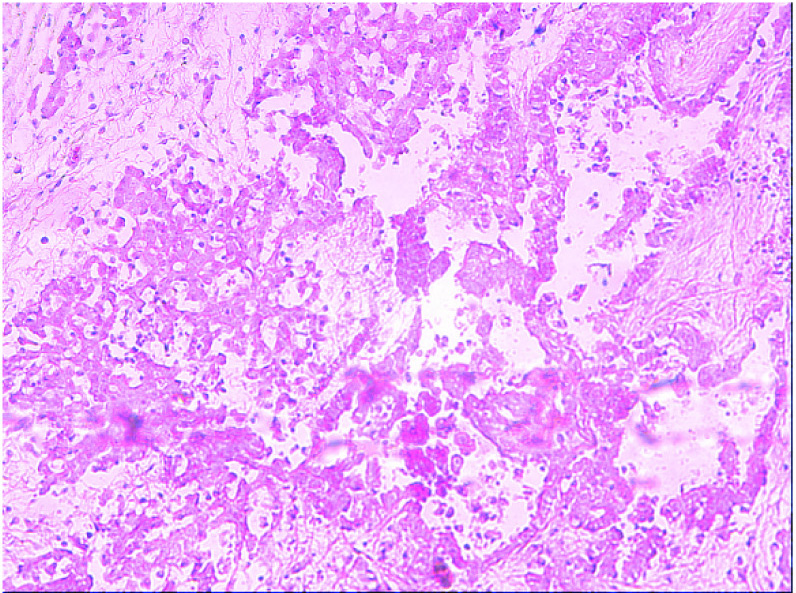
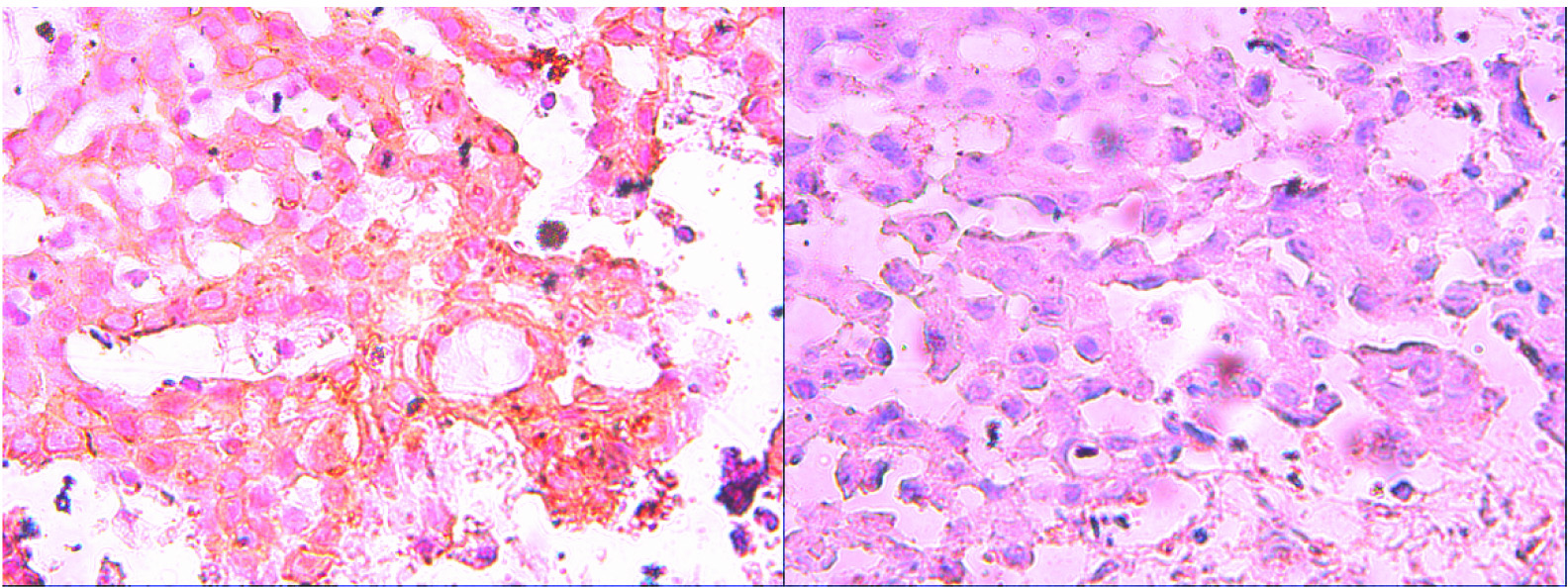
A 60-year-old male, presented to the department of pulmonology of our hospital with the chief complaint of lower right chest pain, dry cough and dyspnoea since one month. The patient had a negative history of smoking and had no asbestos exposure in the past. The pulmonary examination and chest radiography suggested a right pleural effusion [Table/Fig-1]. The thoracentesis found a viscous pleural fluid [Table/Fig-2]. The cytology and chemical study of the pleural fluid revealed a lymphocytic exudative fluid but the hyaluronan analysis was impossible to complete due to the thickness of the fluid. The chest CT scan showed a right pleural effusion with a nodular thickening of the pleura [Table/Fig-3]. The abdominal and pelvic CT scan showed sclerotic lesions of D1 and the right iliac bone. The diagnosis of a prostate or a digestive cancer with pleural and bone metastasis was suspected but the abdominal computed tomography did not show any abnormality. The video assisted thoracoscopy revealed multiple pleural nodules. The histopathology study of the pleural biopsy showed: round cell malignant tumour infiltration with a myxoid stroma reaction [Table/Fig-4]. The immunohistochemistry was positive for CK7 and anti-ACE while it was negative for anti-CK20 and anti-CK5/6 [Table/Fig-5]. Thus, the diagnosis of epitheliod pleural mesothelioma was confirmed. Our patient had a stage IV mesothelioma and was transferred to the Oncology Department where chemotherapy treatments made of cisplatin and pemetrexed was started. The patient died while he was on his treatment.
Chest X ray showing an opacity suggesting a right pleural effusion.


Chest CT scan showed a right pleural effusion with a nodular thickening of the pleura.
Malignant round cell infiltration with myxoid stroma raction: x100 magnification.
(a) Immunohistochemistry study showing positive CK7 on the left and (b) anti-ACE on the right
Discussion
Pleural mesothelioma is a neoplasm derived from the mesothelial cells of the pleural serous. It is very aggressive and the prognosis is generally bad with a median survival time of about one year [1]. Malignant Pleural Mesothelioma (MPM) affects men in 80% of cases and it is most frequent around the age of 60 years [1]. The main aetiological factor is a previous exposure to asbestos with typically long latency duration between exposure and the onset of MPM, around 20 to 40 years [2]. In this case, the patient was 60-year-old but he had not been exposed to asbestos.
The development of MPM is usually insidious, thus, clinical signs often appear at an advanced stage of the disease. In over 60% of cases, patients complain of progressive dyspnoea, cough, and chest pain [3]. General symptoms such as weight loss and fatigue are rare at the beginning of the disease; they appear in the advanced stages of the disease and are associated to poor outcomes [3]. Our patient presented with dyspnoea as the main symptom. The most typical clinical presentation is an unilateral pleural effusion, which is recurrent, and sometimes exudative and haemorrhagic.
The chest radiography and chest CT-scan help to make the diagnosis. The Positron Emission Tomography (PET) also helps in the diagnosis of malignant mesothelioma. Although, it has 91% sensitivity and 100% specificity, it is not systematically recommended for the diagnosis of MPM [4]. The analysis of the pleural fluid, which is typically exudative, is not contributive to the diagnosis of MPM. The cytology of the pleural fluid is useful for the diagnosis of cancer [4]. The diagnosis of MPM is confirmed by cytology in only 20-30% of cases and by percutaneous pleural biopsy in 20-23% of cases. The later method, often, does not produce enough material to confirm this diagnosis. The combination of both has a diagnosis yield of 35 to 40% [4]. Laparoscopy or medical thoracoscopy is a simple examination which is feasible for the majority of patients. It has a sensitivity of 95% for the diagnosis of MPM [4]. In our case thoracoscopy revealed multiple tumour nodules. The pathology examination of pleural biopsy can be difficult. It relies on the morphological examination completed with immunohistochemical analysis. In our case the pathology study showed an epitheliod myxoid stromal tumour.
Mesothelioma is strongly related to asbestos exposure. This exposure is not found in 20% of cases and few cases of pleural mesothelioma without asbestos exposure were reported [5,6]. Other exposures were reported to be linked to malignant pleural mesothelioma such as: some dust or chemicals (leather factories, agriculture, and stone breaking) [7]. Smoking can possibly be a risk factor for pleural mesothelioma but our patient did not smoke. Other exposures raise concern about the possible risk of mesothelioma such as; Erionite, Carbon nanotubes and the monkey polyoma virus [7]. In this case, the patient is a traditional farmer who has never used any chemical substances. He had never worked in any factory and had never dug any wells.
According to the American Cancer society guidelines [4], Cisplatin, Gemsitabin and Pemetrexed are the most commonly used chemotherapy for mesothelioma. According to the patient’s general condition, the tumour’s extent on thoracoabdominal CT scan and the histological type, different treatments were proposed: chemotherapy, surgery (extrapleural pneumonectomy with extended pleurectomy decortication), and radiation therapy. The therapeutic decision should be made after a multi-disciplinary meeting. In our case, the therapeutic decision was chemotherapy.
There are many cases of mesothelioma without any asbestos exposure reported in the literature. Lacle and Van Oosterhout reported a lung mesothelioma localization in a patient who never had any exposure to asbestos dust but had a history of smoking [8]. Iftikhar et al., published a case about a peritoneal mesothelioma in a woman who did not have any dust asbestos exposure [9]. In both cases the diagnosis was difficult to make because of the unusual presentation as well as the absence of asbestos exposure. In our case, the viscous pleural effusion was not unusual for mesothelioma but the absence of asbestos dust exposure or any other exposure linked to mesothelioma made the diagnosis of mesothelioma less probable than the diagnosis of metastatic pleural effusion.
Conclusion
MPM is a cancer with a very poor prognosis, despite the progress made in chemotherapy and surgery. This cancer is linked to asbestos exposure, but in 20% of cases this exposure fails to be found. A significant increase in survival among MPM patients can be reached through earlier diagnosis of the disease. Thus, in case of pleural effusion with pleural nodular thickening, the diagnosis of MPM should be suspected and a thoracoscopy needs to be performed, even if the asbestos exposure is not reported.
[1]. Robinson BW, Musk AW, Lake RA, Malignant mesotheliomaLancet 2005 366:397-408. [Google Scholar]
[2]. Pairon JC, Andujar P, Matrat M, Ameille J, Occupational respiratory cancersRev Mal Respir 2008 25:193-207. [Google Scholar]
[3]. Lee YC, Light RW, Musk AW, Management of malignant pleural mesothelioma: a critical reviewCurr Opin Pulm Med 2000 6(4):267-74. [Google Scholar]
[4]. Conference expert of the Society of French Language Pneumology (SPLF)Recommendations of the pneumology society of French language on pleural mesothelioma (short text)Rev Mal Respir 2006 23:6578-92. [Google Scholar]
[5]. Prasad R, Kant S, Mehrotra P, Suresh Babu K, Agarwal PK, Mesothelioma a report on 3 casesInd J Tub 1998 45:29-30. [Google Scholar]
[6]. Gaur SN, Kumar R, Malignant pleural mesothelioma without asbestos exposureIndian J Chest Dis Allied Sci 1999 41:61-64. [Google Scholar]
[7]. Jasani B, Gibbs A, Mesothelioma not associated with asbestos exposureArch Pathol Lab Med 2012 136:262-67.doi: 10.5858/ arpa.2011-0039-RA) [Google Scholar]
[8]. Lacle M, Van Oosterhout M, An unusual presentation of malignant pleural mesotheliomaJournal of thoracic oncology 2013 8:63-64. [Google Scholar]
[9]. Iftikhar A, Anastasios K, Javaid I, Wong T, Malignant peritoneal mesothelioma as a rare cause of ascites: a case reportJournal of Medical Case Reports 2008 2:121 [Google Scholar]