Coincidental Finding of Beta Thalassaemia Minor in a Patient of Lacquer Thinner Poisoning Presenting as Methaemoglobinemia
Charu Agarwal1, Anisha Mohanpuria2, Gurdeep Buxi3, Vijay Kumar4
1 Presently-Assistant Professor, Department of Pathology, ESIC Medical College and Hospital, Faridabad, Haryana; Formerly-Senior Resident, Department of Pathology, PGIMER Dr RML Hospital, New Delhi, India.
2 Senior Resident, Department of Pathology, PGIMER Dr RML Hospital, New Delhi, India.
3 Professor, Department of Pathology, PGIMER Dr RML Hospital, New Delhi, India.
4 Associate Professor, Department of Pathology, PGIMER Dr RML Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Charu Agarwal, Opd 3rd Floor, PGIMER Dr RML Hospital, New Delhi-110001, India.
E-mail: dr.charu.ag@gmail.com
Lacquer thinner, commonly used for removing household paints, is known to contain various aromatic hydrocarbons and naphtha; if ingested, may cause methaemoglobinemia. We report a case of 13-year-old girl who presented with episodes of vomiting, abdominal pain and numbness of limbs. Peripheral blood smear showed few fragmented erythrocytes and 10-12 nucleated red blood cells /100 white blood cells. Reticulocyte count was 15% with presence of Heinz bodies. There was a history of accidental ingestion of lacquer paint thinner. Levels of methaemoglobin were very high along with raised HbA2 levels. An impression of haemolytic anaemia, due to lacquer thinner paint poisoning, with methaemoglobinemia was given. Incidentally High Performance Liquid Chromatography (HPLC) revealed increased HbA2 levels i.e., heterozygous inheritance of beta thalassaemia minor. Patient responded well to methylene blue. Blood transfusion was performed and symptomatic treatment was given.
Haemolytic Anaemia, Heinz bodies, Heterozygous inheritance
Case Report
A 13-year-old girl presented in emergency with episodes of vomiting, pain abdomen and numbness of limbs. A history of accidental ingestion of lacquer paint thinner was revealed.
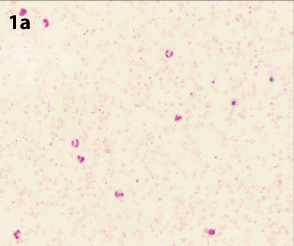
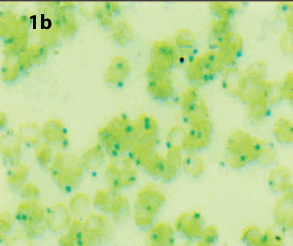
On examination, patient was sick and lethargic. Pallor and cyanosis was present. There was no organomegaly. On Central Nervous System (CNS) examination, patient was conscious but there was decreased tone in all the limbs. The rest of the systemic examination was within normal limits. Haemogram showed Haemoglobin (Hb) 9.9gm/dl, White Blood Cell (WBC) count 40,000/cumm (81% neutrophils, 11% lymphocytes, 6% eosinophils, 2% monocytes) and platelet count 3.3 lac/μl. On peripheral smear, Red Blood Cells (RBCs) showed moderate anisopoikliocytosis with dimorphic picture, normocytic normochromic to microcytic hypochromic cells. Few fragmented RBCs and 10-12 nucleated RBCs/100 WBCs were seen. WBCs showed neutrophilic leukocytosis. Platelets were adequate [Table/Fig-1a]. Reticulocyte count was 15% with presence of Heinz bodies [Table/Fig-1b]. In biochemical investigations, liver function tests: raised total bilirubin (1.8mg/dl) and direct bilirubin (1mg/dl), indirect bilirubin (0.8mg/dl); kidney function tests - was within normal limits.
Peripheral smear (Leishman stain;10x).
Heinz bodies (New Methylene Blue stain;100x).
Further investigations were performed; her coagulation profile was within normal limits and chest X-ray showed no abnormality. Urine analysis showed albumin 2+ with presence of few pus cells and 2-4 RBCs/High Power Field (HPF). Her SpO2 was low (78%) and PaO2 was normal (145mmHg). Patient was further evaluated and various investigations were done including methaemoglobin levels and High Performance Liquid Chromatography (HPLC). Her methaemoglobin levels were found to be raised: 55.8% and HPLC revealed increased HbA2 levels [Table/Fig-2].
High Performance Liquid Chromatography (HPLC).
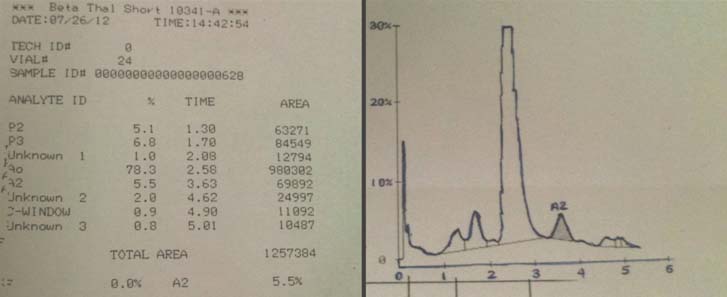
So based on the clinical history, haemogram, peripheral smear and HPLC findings along with an increased methaemoglobin levels, an impression of haemolytic anaemia, due to lacquer thinner paint poisoning, with methaemoglobinemia and co-existence of heterozygous inheritance of beta thalassaemia minor was given.
Patient was given oxygen by mask but she did not respond. Then she was given injection of methylene blue 2ml 1% solution (20mg) intravenous slowly for 5 minutes in seven doses. Her methaemoglobin levels were reduced to 30.2% and subsequently were within normal limits. SpO2 was raised to 90%. Subsequently the patient was given blood transfusion and supportive therapy was continued. She responded well and was discharged on day three.
Discussion
Lacquer thinner is commonly used for paint thinning It is very complex in nature and most versatile among all thinners. It contains various hydrocarbons (benzene, toluene and xylene) or halogenated hydrocarbons (carbon tetrachloride, methane and trichloroethylene) along with P naptha. It is known to cause methaemoglobinemia [1,2].
Methaemoglobin is formed by the oxidation of haemoglobin heme (Fe+2 to Fe+3) and has decreased ability to bind oxygen. Oxygen dissociation curve is left shifted and oxygen delivery to tissues is impaired. Methaemoglobinemia occurs when more than 1% of total haemoglobin occurs in the oxidized form. It occurs when there is an imbalance, either more methaemoglobin production or decreased methaemoglobin reduction. Exposure to toxic substances or absence of reduction pathways lead to increased methaemoglobin levels in blood. Toxic methaemoglobinemia is more common than hereditary type [2].
Arterial blood with elevated methaemoglobin levels has a characteristic dark red, chocolate or brownish to blue colour as compared to normal bright red oxygen- containing arterial blood [2]. Patient with methaemoglobinemia presents with cyanosis, headache, lethargy, fatigue or dyspnea. When methaemoglobin levels are greater than 15%, cyanosis is visible. In many cases, patient is asymptomatic other than cyanosis, but when the concentration of methaemoglobin reaches 30-45%, anoxic symptoms commonly develop. These include headache, dizziness, tachycardia, dyspneaon exertion, muscle cramps and weakness. In cases of acute thinner poisoning, methaemoglobin concentration may exceed 60-70% and may lead to vomiting, lethargy, loss of consciousness, circulatory failure and even death [2]. However, the onset of symptoms does not always correlate with particular methaemoglobin concentration [3]. Other effects include hepatosplenomegaly, altered liver functions and Heinz body haemolytic anaemia [4].
Methaemoglobin should be suspected in patients with cyanosis and presence of symptoms of hypoxia, though PaO2 can still be sufficiently high in such patients. Appropriate history is beneficial to reach the diagnosis. In case of suspicion of methaemoglobinemia, blood test is a key to confirm the presence and level of methaemoglobin [1].
In the present case, patient presented with episodes of vomiting, pain abdomen and numbness of limbs. Patient was sick and lethargic and there was pallor and cyanosis. Although there was no organomegaly but altered liver function tests were present. Peripheral smear showed Heinz bodies. Her PaO2 was in normal range although SpO2 was low. Levels of methaemoglobin were very high i.e., 55.8%. So it was a case of acute poisoning.
On reviewing of literature, very few cases of lacquer thinner poisoning have been reported [1,2,4]. The present case is one of the very few cases of methaemoglobinemia due to lacquer thinner paint poisoning in a 13-year-old female child.
Intravenous injection of 1mg/kg of methylene blue is an effective emergency therapy [5]. In the present case patient also responded well to injection methylene blue. Saxena et al., reported acute poisoning of nitrobenzene in a 16-year-old female where repeated infusions of methylene blue was given to treat the patient successfully [4]. However, our patient had a co-existence of thalassaemia minor. She was given blood transfusion along with symptomatic treatment.
Conclusion
Acute methaemoglobinemia constitutes a medical emergency and may result in significant mortality if not treated. In cases of suspected toxin induced methaemoglobinemia, appropriate doses of methylene blue are advised. Although diagnosis is clinical but in our case, presence of Heinz bodies with haemolytic anaemia corroborated the clinical diagnosis of methaemoglobinemia due to lacquer thinner paint poisoning.
Till now, very few cases have been reported in the literature. To the best of our knowledge, this is the first case in the literature in which patient has methaemoglobinemia (due to lacquer thinner poisoning) associated with a coincidental finding of heterozygous inheritance of beta thalassaemia minor.
[1]. Singh R, Vinayagam S, Vajifdar H, Methaemoglobinemia as a result of accidental lacquer thinner poisoningIndian J Crit Care Med 2012 16:44-47. [Google Scholar]
[2]. Verma S, Gomber S, Thinner intoxication manifesting as methaemoglobinemiaIndian J Pediatr 2009 76(3):315-16. [Google Scholar]
[3]. Wright RO, Lewander WJ, Woolf AD, Methaemoglobinemia: etiology, pharmacology, and clinical managementAnn Emerg Med 1999 34(5):646-56. [Google Scholar]
[4]. Saxena H, Saxena AP, Acute methaemoglobinemia due to ingestion of nitrobenzene (paint solvent)Indian J Anaesth 2010 54(2):160-62. [Google Scholar]
[5]. Fauci AS, Kasper DL, Longo DL, Jameson JL, Braunwald E, Hauser SL, Harrison’s Principles of Internal Medicine(17th edition). Disorders of haemoglobin 2012 The McGraw-Hill Companies United States of America:635-43. [Google Scholar]