Symptomatic Granuloma Secondary to Embolic Agent: A Case Report
Prashant Gunawat1, Salman Tehran Shaikh2, Vikram Karmarkar3, Chandrashekhar Deopujari4
1 Consultant Neurosurgeon, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
2 Senior Resident, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
3 Consultant Neurosurgeon, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
4 Professor and Head of Department, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Salman Tehran Shaikh, V-1, Row House II, Sector 6, Vashi, Navi Mumbai-400703, Maharashtra, India.
E-mail: shaikhsalman25@gmail.com
Onyx is a liquid embolic agent presently gaining wide acceptance for embolisation of multiple vascular cranial pathologies like Arteriovenous Malformation (AVM) and Arteriovenous Fistula (AVF). Onyx stays in the nidus of vascular pathology and initiates inflammatory response leading to thrombosis and subsequently resulting in occlusion of vascular nidus. However, if onyx spills into the surrounding brain tissue, reaction occurs in the form of foreign body inflammatory reaction.
This is one of the very few cases in literature whereby embolisation of AVM with onyx lead to granuloma formation which needed surgical excision. It presented with limb weakness and seizure episodes.
Arteriovenous malformation, Onyx, Seizure
Case Report
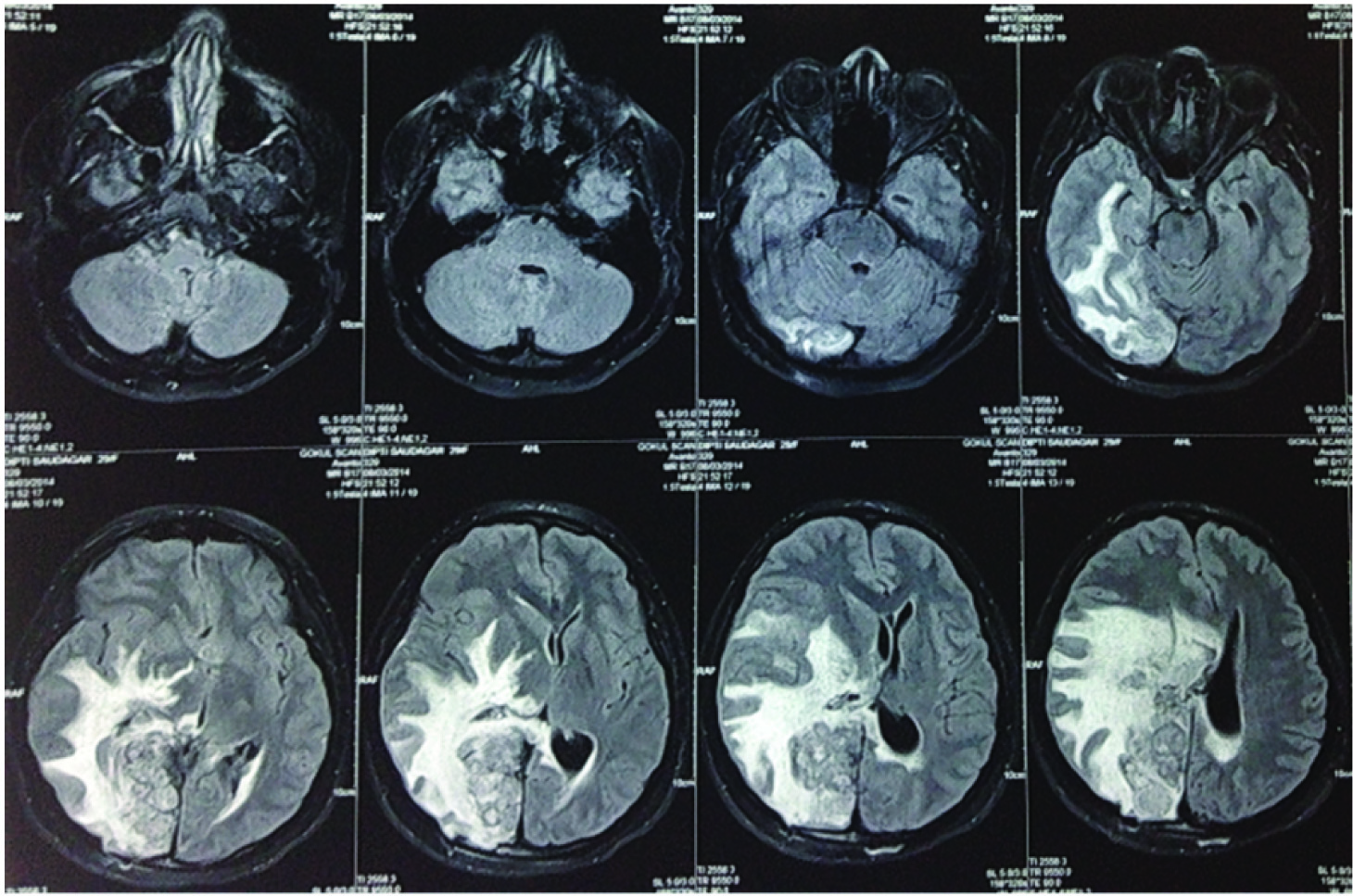
A 24-year-old female presented with weakness of left upper limb and an episode of generalised seizure. She had a history of right parieto-occipital Arteriovenous Malformation (AVM) which was embolised in four settings with different embolic agents (glue, polyvinyl alcohol). She had received Gamma Knife Surgery (GKS) for residual AVM. Post radiosurgical procedure, there was complete obliteration of AVM which was confirmed on angiography. However, she had developed an intracranial Space Occupying Lesion (SOL) at the site of AVM with atypical imaging features [Table/Fig-1]. Surgical excision of this lesion was carried out and histological examination of the specimen showed a foreign body reaction.
MRI image showing intracranial SOL at the site of AVM with atypical features.
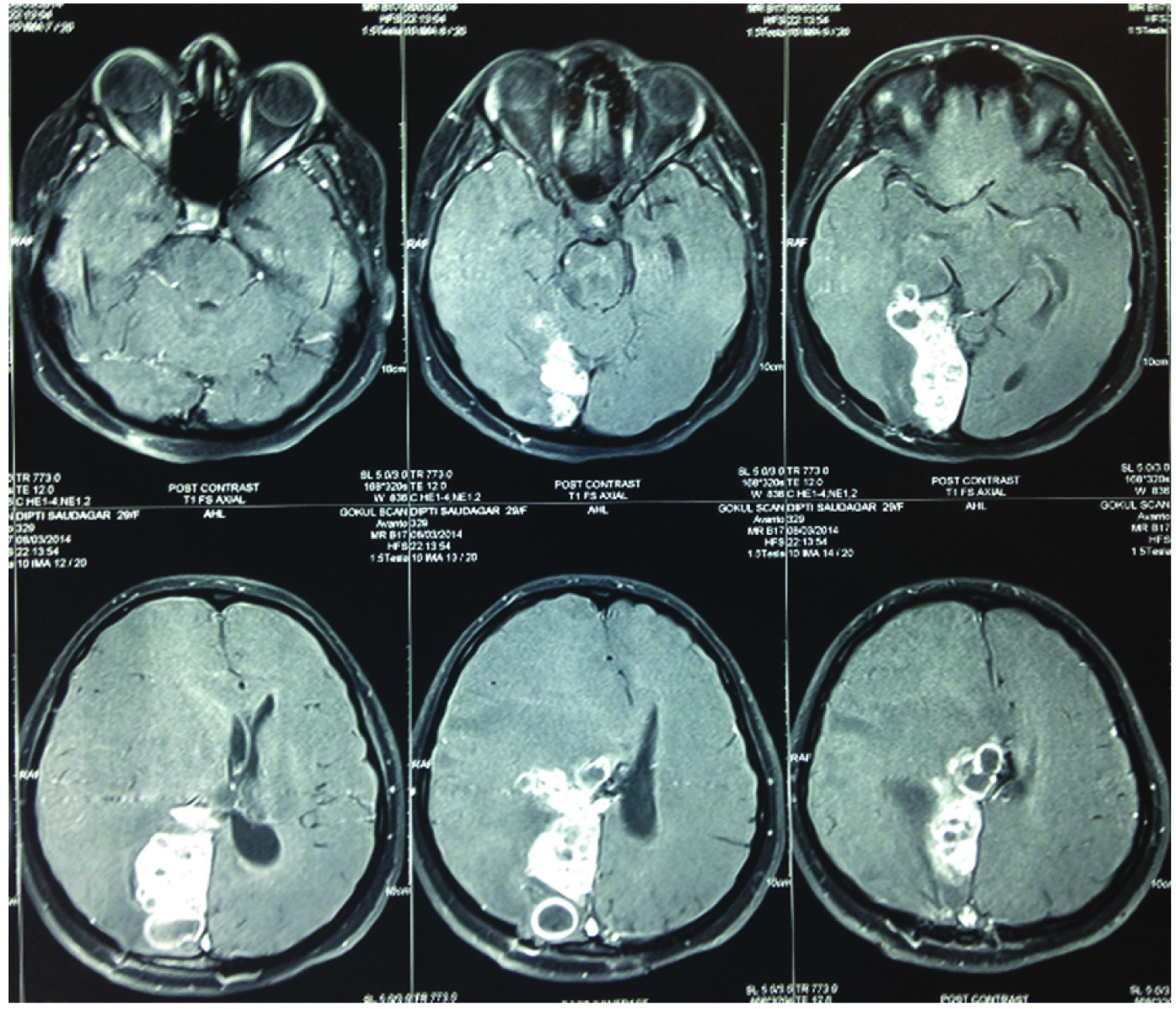
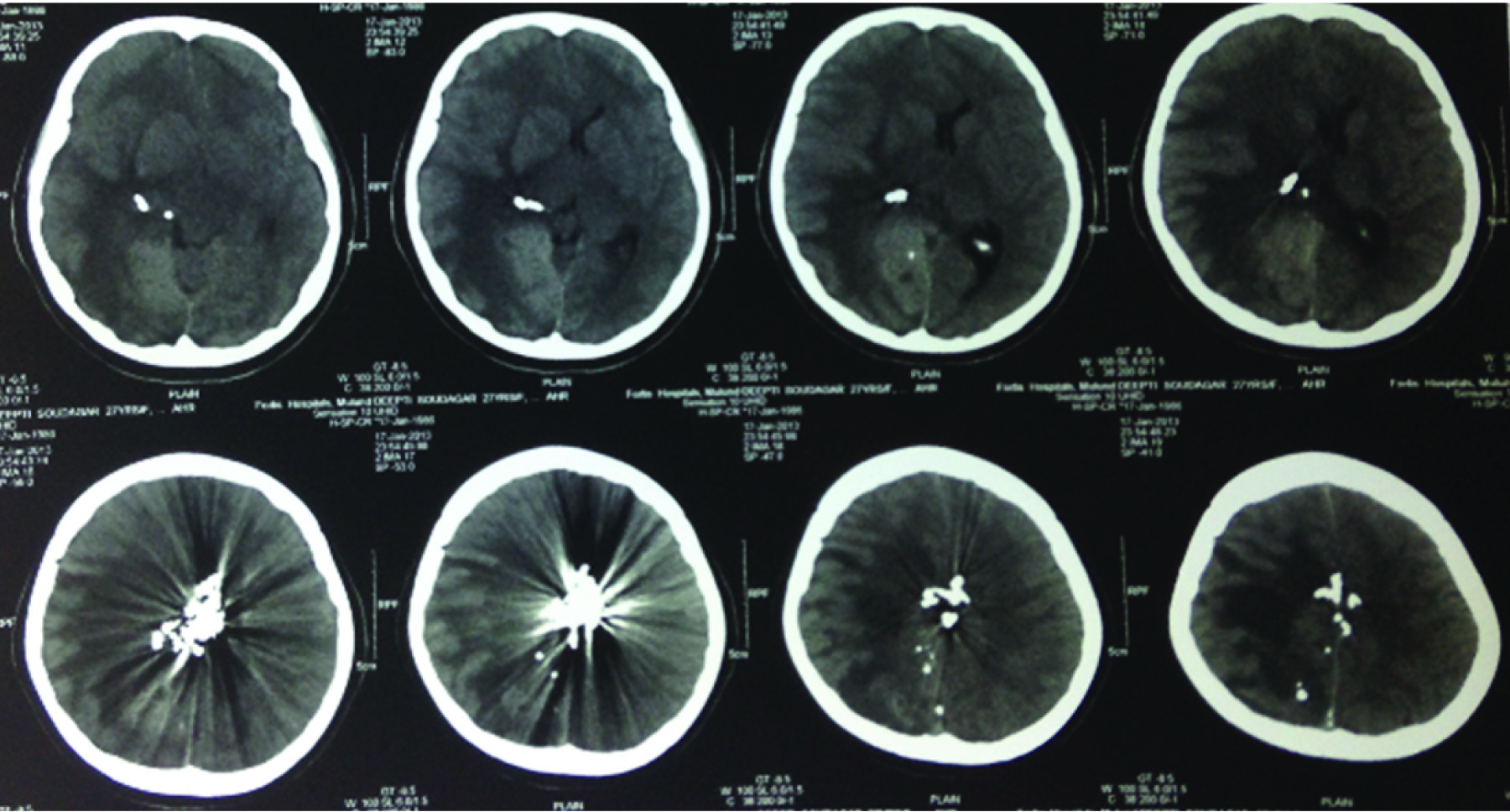
She then came to our institute with weakness of left upper limb and an episode of generalised seizure. Gadolinium contrast MRI showed multiple conglomerate ring enhancing lesion at right parieto-occipital region with mass effect [Table/Fig-2]. Computed Tomography (CT) scan showed artefacts due to the presence of onyx [Table/Fig-3]. We proceeded to do a re-exploration of the previous craniotomy and microsurgical excision of the contrast enhancing lesion. It was a firm mass which was excised completely in piecemeal fashion. Histopathological examination showed an AVM nidus with necrotising granulomatous inflammation with predominant foreign body giant cell reaction. The patient made a good postoperative recovery and has had an uneventful follow-up for the last one year.
Post Contrast image showing multiple conglomerate ring enhancing lesion at right parieto-occipital region with mass effect.
CT scan showing artefact due to onyx.
Discussion
Onyx was approved by US FDA as a liquid embolic agent for brain AVM in July 2005. Onyx initiates an angio-necrotic inflammatory response after coming in contact with vessel intima which progresses from acute to chronic inflammation [1] Clinico-pathological studies performed on resected AVM nidus after embolisation showed different stages of inflammatory response depending upon timing of embolisation and surgical resection [1]. Onyx is rapidly gaining acceptance for embolisation of brain AVM due to its physical properties like low adhesiveness to catheter which allows longer injection time and deeper penetration into nidus [2,3]. Post embolisation resection of AVM is indicated for residual AVM. In our case AVM was completely obliterated and excision of the symptomatic onyx granuloma (embolised AVM nidus) was carried out. Inflammatory process secondary to embolic agent are usually self-limiting and generally do not extend beyond vessel and adjacent brain. Progression of such a granuloma is a very unlikely event, which in our patient may be attributed to Mycobacterium tuberculosis infection. Histopathological examination of resected nidus or onyx granuloma showed evidence of Langerhans giant cells typical of mycobacterium infection and also foreign body giant cells typical of foreign body reaction.
Inflammation outside the nidus into surrounding brain tissue may result due to extravasation secondary to rupture of AVM during embolisation [4]. However, such an event did not occur in this case.
Embolisation of AVM in our patient was done by different agents like glue, polyvinyal alcohol and onyx. Though onyx alone may not be responsible for granuloma formation, we cannot determine the exact agent responsible for granuloma formation.
Conclusion
To summarise, onyx granuloma is a standard foreign body inflammatory response of brain to any embolic agent. The term onyx granuloma therefore may not be considered exclusive only to onyx. They are usually self-limiting but may become progressive and symptomatic in which case treatment is indicated.
[1]. Jahan R, Murayama Y, Gobin YP, Duckwiler GR, Vinters HV, Viñuela F, Embolization of arteriovenous malformations with Onyx: clinicopathological experience in 23 patientsNeurosurgery 2001 48(5):984-95.discussion 995-97 [Google Scholar]
[2]. Ayad M, Eskioglu E, Mericle RA, Onyx: a unique neuroembolic agentExpert Rev Med Devices 2006 3(6):705-15. [Google Scholar]
[3]. Weber W, Kis B, Siekmann R, Jans P, Laumer R, Kühne D, Preoperative embolization of intracranial arteriovenous malformations with OnyxNeurosurgery 2007 61(2):244-52.:252-54. [Google Scholar]
[4]. Lv X, Wu Z, Jiang C, Li Y, Yang X, Zhang Y, Complication risk of endovascular embolization for cerebral arteriovenous malformationEur J Radiol 2011 80(3):776-79. [Google Scholar]