Mucinous Cystadenocarcinoma in a Horse Shoe Kidney Masquerading as Giant Hydronephrosis – A Case Report: Diagnostic Challenges, Lessons Learnt and Review of Literature
Leena Dennis Joseph1, Sriram Krishnamoorthy2, Rajendiran Swaminathan3, Gokul Kripesh4, Hariharasudhan Sekar5
1 Professor, Department of Pathology, Sri Ramachandra Medical College, Porur, Chennai, India.
2 Professor, Department of Urology, Sri Ramachandra Medical College, Porur, Chennai, India.
3 Professor, Department of Pathology, Sri Ramachandra Medical College, Porur, Chennai, India.
4 Postgraduate Student, Department of Pathology, Sri Ramachandra Medical College, Porur, Chennai, India.
5 Assistant Professor, Department of Urology, Sri Ramachandra Medical College, Porur, Chennai, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sriram Krishnamoorthy, Professor, Department of Urology, Sri Ramachandra Medical College & Research Institute, Porur– 600125, Chennai, India.
E-mail: sriramuro@gmail.com
Primary epithelial tumour of the renal pelvis is a rare entity. So far, very few cases are reported in literature. Of these, mucin secreting adenocarcinomas are distinctly rare. However, mucinous cystadenocarcinoma, that too arising in a horse shoe kidney is extremely rare to be reported. Mucinous cystadenomas and carcinomas arising from the renal pelvis are regarded to be secondary to a metaplastic change in the urothelium. Here, we present a case of a 51-year-old male, who complained of abdominal pain, palpable abdominal mass, haematuria along with passage of mucoid material in the urine, with a very poorly functioning kidney. A pre-operative diagnosis of horse shoe kidney with pelvi ureteric junction obstruction and a poorly functioning kidney was made. Intraoperative findings and frozen section biopsy were suggestive of mucin secreting cystic mass and a right heminephrectomy was done. The final histopathology was suggestive of mucinous cystadenocarcinoma of the renal pelvis of the right moiety. This case is presented for its rarity, diagnostic challenges faced and the lessons learnt, stressing on the need for having a high index of clinical suspicion in making such diagnosis.
Haematuria, Heminephrectomy, Primary epithelial tumour
Case Report
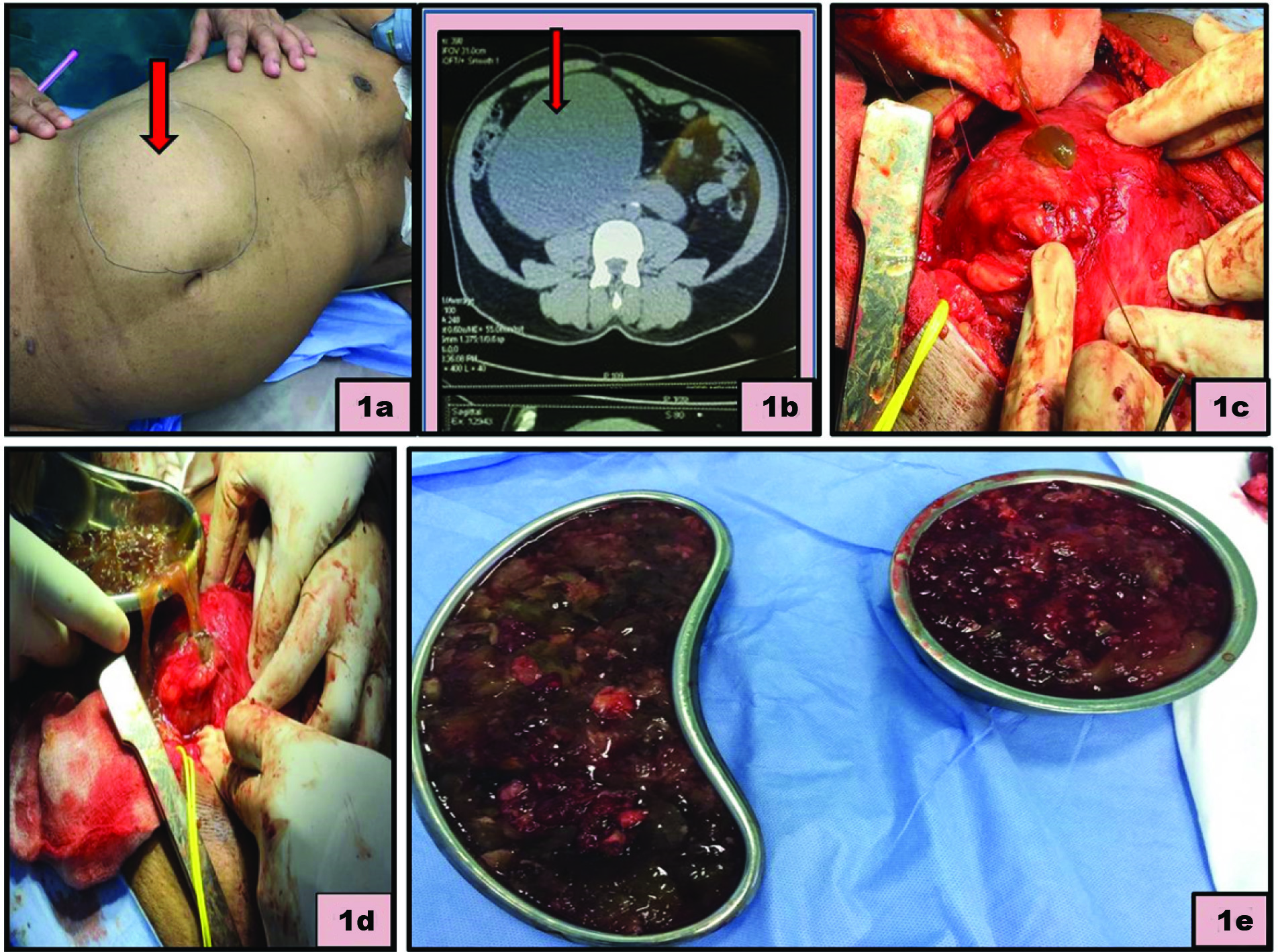
A 51-year-old male, presented with persistent right loin discomfort and a palpable right flank mass of one year duration [Table/Fig-1a]. He also had painless total haematuria and also complained of occasional passage of mucoid material along with urine. Computed Tomography (CT) abdomen showed a hugely hydronephrotic right moiety, with grossly thinned out renal parenchyma and fusion of both lower poles, suggestive of a horse shoe kidney with a poorly functioning hydronephrotic right moiety. The right kidney measured approximately 15cm in its greatest dimension, with density ranging from +10 to +20 Houndsfield Units (HU), consistent with the findings of Pelvi Ureteric Junction Obstruction (PUJO) with giant hydronephrosis and thinned out parenchyma with a poorly functioning right moiety [Table/Fig-1b]. With a diagnosis of a hydronephrotic right kidney, with negligible parenchymal function being met, right heminephrectomy was planned. Intraoperatively, the right moiety was found to be densely adherent to the duodenum and the peritoneum [Table/Fig-1c]. On decompression of the right moiety, about 1.5 litres of mucinous or gelatinous material was aspirated [Table/Fig-1d&e]. The renal parenchyma showed irregular areas of thickening.
(a) Palpable right loin mass, felt as fullness of abdomen; (b) CT film showing huge hydronephrosis; (c-e) Nephrectomy in progress.
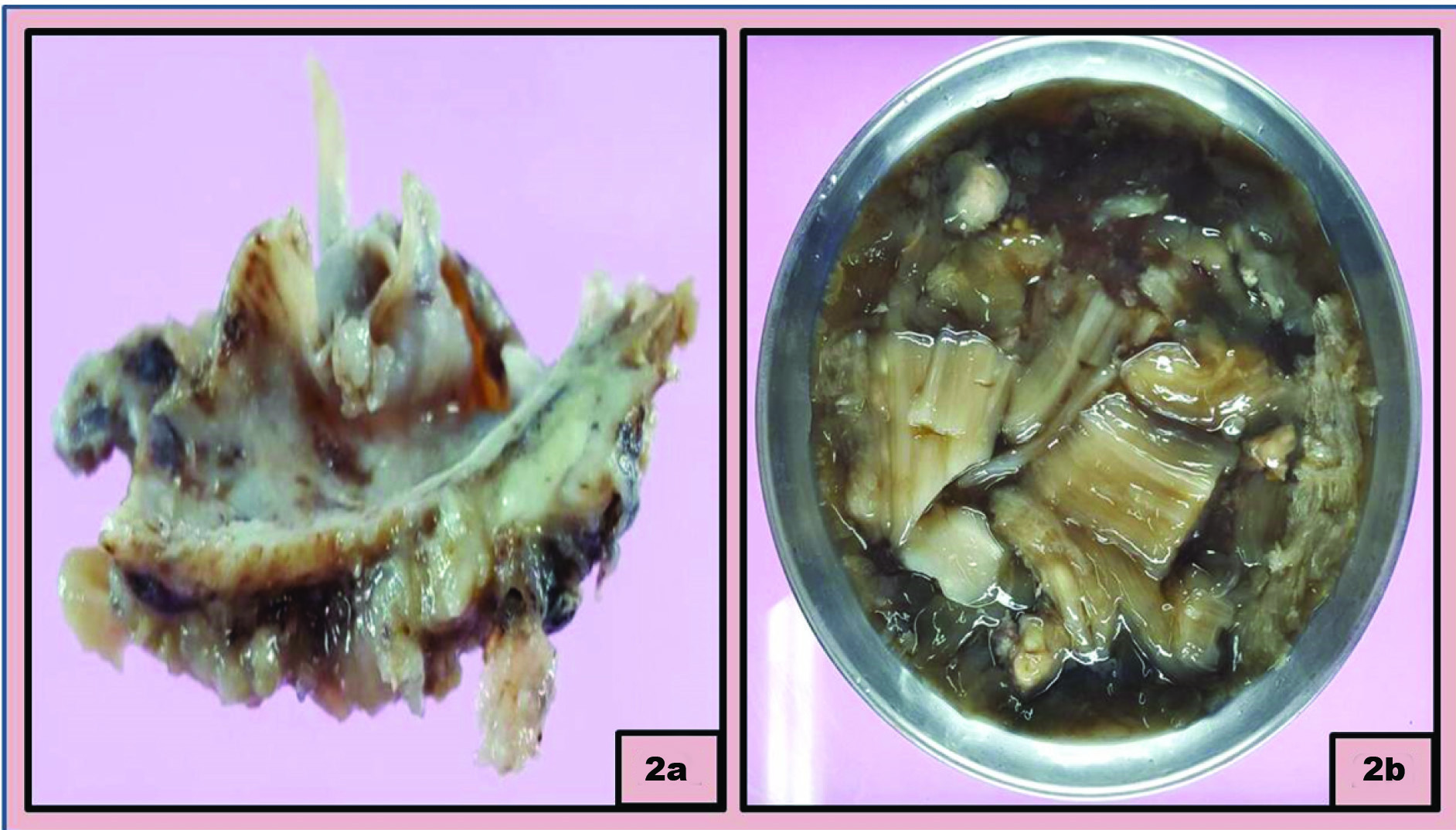
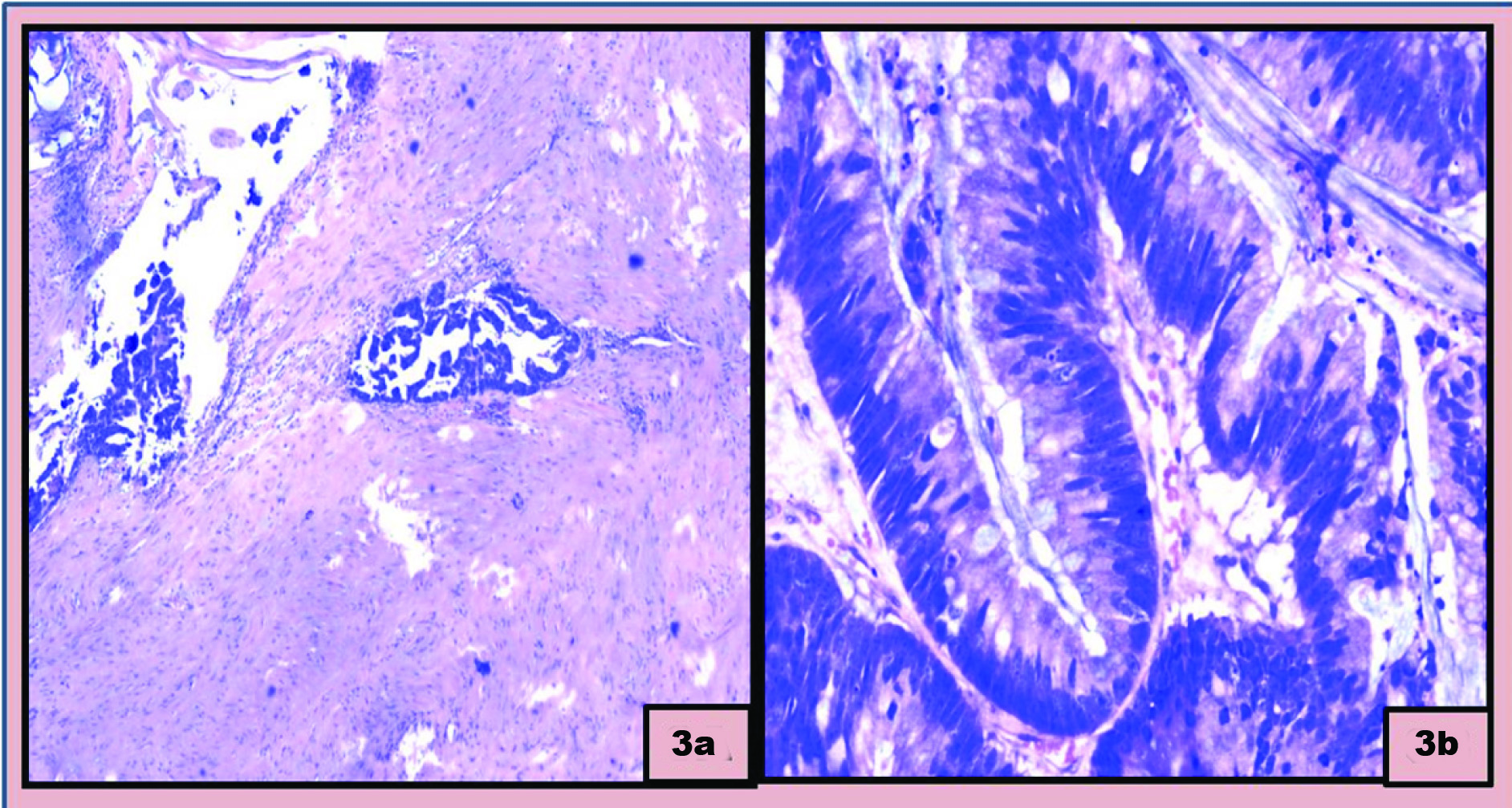
The removed right kidney specimen measured 10 cm in its largest dimension. Multiple fragments of the gelatinous material were found adherent to the inner wall of the renal parenchyma. Kidney was contracted, greyish brown, with focal grey black areas. On opening the kidney, the cortex was found to be grossly thinned out. The pelvicalyceal system was dilated and filled with gelatinous material. There were also thin flaps of tissue at the hilum with focus of gelatinous material [Table/Fig-2a&b]. Microscopic examination revealed focal areas of a papillary cystadenocarcinoma arising from a cyst with extensive areas of mucinous material [Table/Fig-3a&b]. The lining epithelium of the cyst was mucin secreting columnar epithelium.
(a) Fragmented tumour in mucinous material; (b) Gross specimen showing focal solid papillary areas in the cyst wall.
(a) Photomicrograph showing the papillary tumour showing stromal Invasion (H&E x40); (b) Photomicrograph showing the tumour in a background of mucin (H&E x400)
Patient had an uneventful post-operative period. He was advised to undergo adjuvant chemotherapy using cisplatin based drugs as there was an unintentional spillage of mucin material during surgery.
Discussion
Primary epithelial tumour of the renal pelvis is a rare condition. So far, approximately only about 100 such cases are reported in literature [1]. Transitional cell carcinomas constitute a vast majority of the malignant tumours of the renal pelvis (up to 85 to 90%). Squamous cell carcinomas constitute the rest (10 to 15%), with adenocarcinomas accounting for less than 1% of all such malignancies [2].
Renal pelvic tumours are predominantly urothelial in origin, but at times squamous and glandular lesions may arise, secondary to a metaplastic change. With this change, the lesion may turn into a mucinous cystadenoma, tubulovillous adenoma or cystadenocarcinoma [3]. Horse shoe kidney is one of the rare developmental anomalies. It constitutes the most common renal fusion anomaly, seen in 1 in 400 people, with a male - female ratio of 2:1 [4]. The abnormal course of the ureters might predispose to stasis of urine in the renal pelvis, infection and subsequent stone formation, but malignant transformation is relatively a rare occurrence in such patients [5]. The occurrence of such tumours in a horse shoe kidney is very rare. The first case of adenocarcinoma in the renal pelvis of a horse shoe kidney was reported by Albert et al., [6]. In this report, we discuss a rare case of malignant cystadenocarcinoma of the renal pelvis, camouflaged as a giant hydronephrosis.
Renal cell carcinoma is the most common tumour reported to develop in a horse shoe kidney. Association of adenocarcinoma of the renal pelvis in a patient with horse shoe kidney is extremely rare. These tumours arise in a background of intestinal metaplasia of the transitional epithelium in the pelvis [7]. Glandular metaplasia is also thought to be associated with urolithiasis and pyelonephritis [8]. Accumulation of the mucin within the collecting system may result in gross hydronephrosis. Such a condition is called as Muconephrosis [9].
A higher incidence of prevalence of adenocarcinomas of renal pelvis has been reported from India. Terris et al., proposed various reasons including dietary or environmental factors as probable reasons for such a high prevalence. However the exact reason for the same is unclear [10].
Mucinous adenocarcinoma of the renal pelvis has a propensity to spread over broad areas of renal pelvis and calyceal surfaces. This would resemble a flat physical structure, many a time, with no evidence of any form of proliferative growth, which might cause difficulty in diagnosing the condition pre-operatively by CT scan. Intraoperatively, the surgeon may not find any obvious mass and the pathologist may also find it difficult to recognize the presence of tumour on gross examination of the nephrectomy specimen. It would pose even more diagnostic challenge, if it is partly obscured by an infective process [11].
Sometimes, it can be quite complex to distinguish a mucinous cystadenoma from a hydronephrotic kidney based on physical findings, laboratory data, and imaging studies, including ultrasonography, CT scan, and Magnetic Resonance Imaging. The final diagnosis is usually made only after tumour excision. The density of hydronephrotic kidney ranges from −10 to +20 HU on CT and such cystadenocarcinomas will also have a similar range of density, which makes it extremely difficult for the radiologist to differentiate between the two. In our patient, the density of the cystadenocarcinoma ranged from +10 to 20 HU and the radiologic features mimicked a PUJO with hydronephrosis. Mucinous cystadenocarcinomas of the kidney may therefore be under-diagnosed by various routine imaging studies [12].
Joshi and colleagues suggested that the formation of stones may be secondary to the mucin secretion from the cystic tumour [13]. They proposed that the secreted mucin may have caused neoplastic formations after fusing with sodium and calcium. The overall prognosis in such mucinous cystadenocarcinomas has been very poor, with more than 50% of these patients succumbing to the disease in the first two years [14]. The plane of dissection is also very difficult to obtain and hence, local recurrences are more common in such patients, as the possibility of intraoperative tumour spillage is much higher in such individuals. Such patients might benefit from adjuvant chemotherapy or radiotherapy, although controversial. Hsiang Ying and colleagues indicated that the standard therapy for mucinous cystadenocarcinoma would be radical nephroureterectomy and bladder cuff excision [15]. But ureterectomy is most likely to be missed out, as most of the times, the diagnosis is made later. Moreover, in view of dense adhesions with adjacent structures, careful manipulation is advocated in order to prevent a tumour spillage. Our patient had a minimal spillage of mucin during surgery and has been advised adjuvant chemotherapy.
Conclusion
Mucinous cystadenocarcinomas are rare tumours with aggressive behaviour and poor prognosis. A high index of clinical suspicion, prompt treatment and a tumour free resected margin offers a better prognosis. Since there is no definite adjuvant therapy, earlier diagnosis and appropriate treatment would be the most effective form of treatment in such patients. Moreover the clinical presentation with passage of mucus like material in urine was also very striking and should arouse the suspicion in the minds of the surgeon. In our patient, the classical history of passing gel like material in urine was grossly ignored by us pre-operatively, resulting in an on-table surprise. The whole purpose of this case report is to highlight the rarity of this tumour and also to raise a high index of clinical suspicion, in order to recognize this entity as a distinct possibility so that subtle gross appearance of such tumours should alert both the surgeon and the pathologist when they are dealing with such conditions.
[1]. Shah VB, Amonkar GP, Deshpande JR, Bhalekar H, Mucinous adenocarcinoma of the renal pelvis with pseudomyxomaperitoneiIndian J Pathol Microbiol 2008 51(4):536-37. [Google Scholar]
[2]. Han DS, Yuk SM, Youn CS, Park G, Sul HJ, Jang H, Primary mucinous cystadenocarcinoma of the renal pelvis misdiagnosed as ureteropelvic junction stenosis with renal pelvis stone: a case report and literature reviewWorld J Surg Oncol 2015 13:324 [Google Scholar]
[3]. Rao P, Pinheiro N, Franco M, Ra S, Costa H, Manzano J, Pseudo-myxomaperitonei associated with primary mucinous borderline tumour of the renal pelvicalyceal systemArch Pathol Lab Med 2009 133(9):1472-76. [Google Scholar]
[4]. Ongeti KW, Ogeng’O J, Saidi H, A horseshoe kidney with partial duplex systemsInternational Journal of Anatomical Variations 2011 4:55-56. [Google Scholar]
[5]. Jhobta R, Bawa AS, Attri AK, Kaushik R, Adenocarcinoma in Horseshoe kidney. Adenocarcinoma in Horseshoe kidneyYonsei Med J 2003 44(4):744-46. [Google Scholar]
[6]. Albert PS, D’Anna J, Papillary cystadenocarcinoma in horseshoe kidney Urology 1973 2(3):296-97. [Google Scholar]
[7]. Takehara K, Nomata K, Eguchi J, Mucinous cystadenocarcinoma of the renal pelvis associated with transitional cell carcinoma in the renal pelvis and the bladderInt J Urol 2004 11:1016-18. [Google Scholar]
[8]. Kaur G, Naik VR, Rahman MNG, Mucinous adenocarcinoma of the renal pelvis associated with lithiasis and chronic goutSingapore Med J 2004 45(3):125 [Google Scholar]
[9]. Sonmez FC, Esen HH, Tavlı L, Kılınç M, Well-Differentiated mucinous Cysta-denocarcinoma of the renal pelvisEur J Gen Med 2014 (Suppl 1):63-65. [Google Scholar]
[10]. Terris MK, Anderson RU, Mucinous adenocarcinoma of the renal pelvis in natives of IndiaUrolInt 1997 58:121-23. [Google Scholar]
[11]. Liwnicz BH, Lepow H, Schutte H, Fernandez R, Caberwal D, Mucinous adenocarcinoma of the renal pelvis: Discussion of the possible pathogenesisJ Urol 1975 114(2):306-10. [Google Scholar]
[12]. Mitome T, Yao M, Udaka N, Fusayasu S, Izumi K, Osaka K, Mucinous cystadenoma of a horseshoe kidney: A case report and literature reviewCan Urol Assoc J 2015 9(1-2):E30-32. [Google Scholar]
[13]. Joshi K, Jain K, Mathur S, Mehrotra GC, Mucinous adenocarcinoma of the renal pelvisPostgrad Med J 1980 56(656):442-44. [Google Scholar]
[14]. Han DS, Yuk SM, Youn CS, Park G, Sul HJ, Jang H, Primary mucinous cystadenocarcinoma of the renal pelvis misdiagnosed as ureteropelvic junction stenosis with renal pelvis stone: a case report and literature reviewWorld J Surg Oncol 2015 13:324 [Google Scholar]
[15]. Lee H-Y, Jang M-Y, Wu W-J, Shen J-T, Wang H-S, Chang S-F, Primary mucinous adenocarcinoma of the renal pelvisUrological Science 2014 25:65e-67. [Google Scholar]