Post-caesarean Haematomas, Septic Collections and Wound Disruptions– Re-Laparotomy Based on Abdominal Imaging
Akhila Vasudeva1, Sapna Vinit Amin2, Koteshwara Prakashini3, Sunanda Bharatnur4, Anjali Mundkur5
1 Associate Professor, Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
2 Associate Professor, Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
3 Professor, Department of Radiology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
4 Associate Professor, Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
5 Associate Professor, Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal University, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Akhila Vasudeva, Associate Professor, Department of Obstetrics and Gynecology, Kasturba Medical College, Manipal University, Manipal-576104, Karnataka, India.
E-mail: akhilavasudeva@gmail.com
Post-caesarean sepsis, Uterine wound dehiscence, Ultrasound, Vesical flap haematoma
Raising incidence of caesarean section is a global concern, especially in the low resource countries [1,2]. Inadequate aseptic precautions, improper surgical technique, indiscriminate use of antibiotics leading to increasing antibiotic resistance, suboptimal post-operative care and ascending genital infections all contribute to increasing incidence of post-caesarean abdominal sepsis. We present a series of six referrals in 12 months; who presented with post-caesarean haematomas, septic collections and uterine wound dehiscence. Decision for re-laparotomy had to be taken diligently taking clinical picture along with imaging findings.
All were primigravidae and caesareans done for suspected “Cephalopelvic disproportion”. Case details are summarized in [Table/Fig-1].
Clinical, imaging, operative details of six cases.
| Case | Clinical presentation | USG findings | CT/MRI | Indication for re-laparotomy | Laparotomy findings | Benefit of re-laparotomy |
|---|
| 1 | Severe atonic PPH and DIC, uterine artery embolization controlled PPH | Multiple haematomas throughout abdominal wall layers, UV fold and uterine cavity | Not done | Multiple non resolving haematomas | Consistent with USG findings | Beneficial and justified |
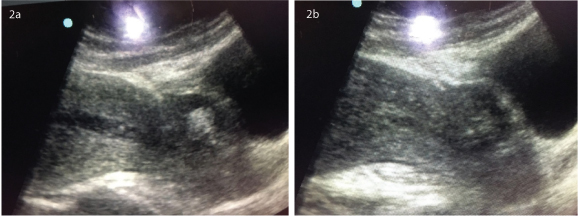
| 2 | Multiorgan failure and sepsis 2 weeks after caesarean | UV fold haematoma, suspected scar disintegrity but intact serosa [Table/Fig-2a&b] | CT : Reported scar dehiscence [Table/Fig-3c] | Suspected scar dehiscence and UV fold haematoma | Intact uterine scar, haematoma evacuated | Unclear, patient worsened and succumbed |
| 3 | Large abdominal wall haematoma hours after caesarean, a drop in Hb | Large abdominal wall haematoma of 8 cm | Not done | Clinical picture and a large haematoma in USG | Bleeding from inferior epigastric artery | Justified and life saving |
| 4 | Secondary PPH 2 weeks following caesarean | Complete uterine myometrial scar dehiscence with intact serosa | MRI [Table/Fig-3b]: Focal breech in uterine scar on right lateral aspect, with intact serosa | Clinical picture and USG findings | Consistent with MRI | Justified |
| 5 and 6 | Surgical Site Infection and intra abdominal septic collections 2 weeks after caesarean | USG inconclusive, as scars appeared hazy, irregular with peritoneal fluid collections | CT [Table/Fig-3a,d]: Reported as uterine scar dehiscence | Uterine scar dehiscence with intraabdominal sepsis | No dehiscence but uterine scar necrotic and sloughing. Extensive peritoneal adhesions | Benefit of re-laparotomy doubtful, as uterine scars could not be freshened or resutured, only thorough peritoneal lavage done |
(a) Haematoma seen bulging the UV fold of peritoneum, containing mixed echogenic areas. (b) Linearhypoechoic area seems to extend from the endometrial lining into the scar, raising the suspicion of myometrial scar dehiscence, however serosa is clearly intact.
(a-d) – Image showing CT/MRI pictures, with varying degrees of uterine wound disruption along with haematomatous/septic collection; with respective surgical findings for correlation. (a) CT scan of abdomen sagittal image showing a linear hypodense area (arrow) noted in the lower uterine segment extending from the endometrial cavity till the serosal surface s/o complete dehiscence along with ascites. On laparotomy, uterine scar was found inflamed, sloughing till serosa. However, no dehiscence demonstrated. (b) MRI pelvis coronal post contrast image (patient with secondary postpartum hemorrhage) showing focal breach in the endometrium and myometrium (black arrow) along right lateral aspect with intact serosa (double arrow) suggesting scar dehiscence, however no peritoneal fluid/ haematoma in uterovesical pouch. On laparotomy, a 2 cm rent was seen in the uterine scar from which pus, blood clots and debris were extruding, serosa intact. (c) Plain CT of pelvis showing a large well defined haematoma (arrows) anterior to the body of the uterus with no breech in myometrium. However in view of large haematoma, partial serosal side dehiscence was considered. On surgery, uterine wound was intact. Haematoma found in the uterovesical region and 300 gm of clot has been evacuated. (d) Abdominal CT showing focal hypodense area reported as possibly dehiscence in uterine scar (red arrows) with indistinct serosal lining however no haematoma anterior to uterus. Uterine scar was found to be necrotic, thin and sloughing, however showed no area of dehiscence on laparotomy.
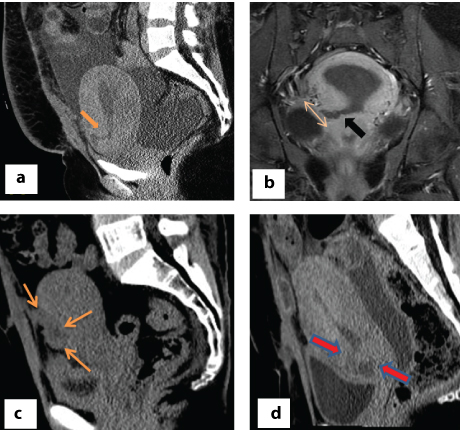
First two patients had severe atonic post-partum hemorrhage at caesarean, managed by oxytocics/ blood components at the referring hospital. First among them (Case 1) was managed by uterine artery embolization in our center, after which she seemingly settled. However, she was found to have multiple large non resolving haematomas which were clearly delineated by ultrasound. Decision for re-laparotmy was clear cut. Second patient (case 2) underwent re-laparotomy mainly based on the CT report showing scar dehiscence, although ultrasound showed intact serosa in the UV fold. Post-operatively, her renal failure worsened and unfortunately she succumbed. We were unsure whether the stress of major surgery and anaesthesia added onto her morbid condition with multiorgan failure. As in case 3, a bedside ultrasound along with clinical picture, is all that was necessary to take a decision on re-laparotomy.
As in Case 4, severe secondary Post Partum Haemorrhage (PPH) is usually associated with scar dehiscence near the angle and bedside ultrasound helped us clearly identify this dehiscence. Although, MRI helped in corroborating the finding, probably decision for re-laparotomy would be taken based on USG and clinical picture. In Case 5 and 6, ultrasound images were inconclusive unlike the above 4 cases. CT findings were non-specific. Re-laparotomies were performed with the intention of freshening the uterine edges followed by resuturing the uterine wound; which could not be performed. Benefit of a peritoneal lavage is controversial. Probably continued broad spectrum antibiotics may have improved their abdominal sepsis, even without re-laparotomy. This approach might benefit even those with some dehiscence of uterine scar.
All six patients underwent re-laparotomy. We tried to correlate ultrasound picture, other imaging modalities including CT/MRI, with that of intraoperative findings. Our aim was to know if our decision of re laparotomy was justified based on imaging findings.
It was our observation that clinical picture along with a bedside ultrasound in an experienced hand, were all that were necessary to take a decision for re-laparotomy, without additional help from further imaging techniques (CT/MRI). This is important in low resource settings. Ultrasound pictures of the uterine scar integrity were very clear where serosa was intact. However, when the serosa was infected sloughing; neither ultrasound nor CT could give us a clear picture of uterine scar. In these situations, as in our cases 5 and 6, literature is not clear on the benefit of re-laparotomy. We need more data as to how to manage these cases, as conservative management also has risks and uncertainty on the clinical improvement of patient. Large case series of such cases are needed; throwing light on the pattern of microbes causing intra-abdominal sepsis and their antibiotic sensitivity pattern. We would witness increasing number of post-caesarean sepsis in the future and hence we need clearer management guidelines.
Thus, any large collection like bladder flap haematoma >4-6 cm [1], sepsis unresponsive to adequate antibiotic therapy, or secondary PPH would justify re-laparotomy. But CT/MRI detected uterine scar dehiscence in a stable patient would not always warrant re-laparotomy [2,3]; as there may not be a dehiscence or patient may not additionally benefit from re-laparotomy even if there is a dehiscence. However, when infection does not subside with antibiotic therapy, laparotomy must be done in order to do a thorough peritoneal lavage and debridement of necrosed tissue. Samples can be sent for culture sensitivity so that appropriate antibiotic therapy is instituted.
It is known that imaging findings poorly correlate with surgical findings, when it comes to uterine dehiscence [4–6]. Presence of a large haematoma due to partial volume averaging of soft tissues, leads to poor visualization of uterine serosa. Scar dehiscence is presumed in presence of a large haematoma and a heterogenous appearing uterine wound on CT. MRI is known to have better sensitivity and specificity in diagnosing uterine wound dehiscence, as compared to ultrasonography and CT, although ultrasound can give clues for the diagnosis. T2 weighted MR will show hyperintense area throughout the thickness of uterine wall along with a large size fluid collection [7]. Specifically, MRI can help delineate serosal layer clearly thus helping to differentiate dehiscence from rupture [8,9]. This is important because scar rupture usually necessitates laparotomy.
Rodgers SK et al., have described imaging findings after caesarean section, including normal findings and findings in case of complications [8]. It is common to find a hypoechoic area of discontinuity in the myometrium at the caesarean scar site, especially in the first few weeks following the surgery. This should not be interpreted as dehiscence. On the contrary, a wide irregular gap along with a large haematoma seen in a patient with features of peritonitis/sepsis, would warrant a re-laparotomy.
To conclude, there is a huge burden of post-caesarean haematomas/sepsis, in the background of alarmingly increasing rate of caesarean section in developing countries. Clinical assessment along with a bedside ultrasound by an experienced sonographer; could be all that is necessary to take a decision on re-laparotomy. Decision for re-laparotomy should not be taken solely based on uterine wound dehiscence detected on CT/MRI.
[1]. Malvasi A, Tinelli A, Tinelli R, Rahimi S, Resta L, Tinelli FG, The Post-Cesarean Section Symptomatic Bladder Flap Haematoma: A Modern ReappraisalJ Matern Fetal Neonatal Med 2007 20(10):709-14. [Google Scholar]
[2]. Incebiyik A, Hilali NG, Camuzcuoglu A, Karakas E, Aydin H, Vural M, A conservative approach to uterine dehiscence cases without bleeding after cesarean: A review of 3 casesActa Medica Mediterranea 2013 29:403-05. [Google Scholar]
[3]. Mahajan D, Kang M, Sandhu MS, Jain V, Kalra N, Khandelwal N, Rare complications of cesarean scarIndian Journal of Radiology and Imaging 2013 23(3):258-61. [Google Scholar]
[4]. Rivlin ME, Patel RB, Carroll CS, Morrison JC, Diagnostic imaging in uterine incisional necrosis/dehiscence complicating cesarean sectionJ Reprod Med 2005 50(12):928-32. [Google Scholar]
[5]. Dhar RS, Misra R, Postpartum Uterine Wound Dehiscence Leading to Secondary PPH: Unusual SequelCase Reports in Obstetrics and Gynecology 2012 2012:1-3. [Google Scholar]
[6]. Brown CE, Dunn DH, Harrell R, Setiawan H, Cunningham FG, Computed tomography for evaluation of puerperal infectionsSurg Gynecol Obstet 1991 172(4):285-89. [Google Scholar]
[7]. Paspulati RM, Dalal TA, Imaging of complications following gynecologic surgeryRadio Graphics 2010 30(3):625-42. [Google Scholar]
[8]. Rodgers SK, Kirby CL, Smith RJ, Horrow MM, Imaging after cesarean delivery: acute and chronic complicationsRadiographics 2012 32(6):1693-712. [Google Scholar]
[9]. Maldjian C, Milestone B, Schnall M, Smith R, MR appearance of uterine dehiscence in the post-cesarean section patientJ Comput Assist Tomogr 1998 22(5):738-41. [Google Scholar]